IndianJMedSci6611-3703196_101711
Transcript of IndianJMedSci6611-3703196_101711
-
7/24/2019 IndianJMedSci6611-3703196_101711
1/12
1
Indian Journal of Medical Sciences, Vol. 66, No. 1 and 2, January and February 2012
STRESS AND ITS RISK FACTORS IN MEDICAL STUDENTS: AN
OBSERVATIONAL STUDY FROM A MEDICAL COLLEGE IN INDIA
MADHUMITA NANDI, AVIJIT HAZRA1, SUMANTRA SARKAR, RAKESH MONDAL2,MALAY KUMAR GHOSAL3
ABSTRACT
OBJECTIVES: Stress in medical students is well established. It may affect academic
performance and lead to anxiety, depression, substance abuse, and burnouts. There
is limited data on stress in Indian medical students. We conducted an analytical
observational study to assess the magnitude of stress and identify possible stressors
in medical students of a teaching hospital in Kolkata.MATERIALS AND METHODS:This
questionnaire-based study was conducted in the Institute of Post Graduate MedicalEducation and Research, Kolkata with consenting undergraduate students of 3 rd,
6th, and 9th (final) semesters, during lecture classes in individual semesters on a
particular day. The students were not informed about the session beforehand and were
assured of confidentiality. The first part of the questionnaire captured personal and
interpersonal details which could be sources of stress. The rest comprised three rating
scales the 28-item General Health Questionnaire to identify the existence of stress,
the WarwickEdinburgh mental well-being scale to assess the mental well-being, and
the revised version of the Lubben social network scale to assess the social networking.
The responses and scores were compared between the three semesters as well asbetween various subgroups based on baseline characteristics. RESULTS: Data from
215 respondents were analyzed approximately 75% were male, 45% came from
rural background, 25% from low-income families, and 60% from vernacular medium.
Totally, 113 (52.56%; 95% confidence interval: 43.35-61.76%) students were found to
be stressed, without significant difference in stress incidence between the semesters.
About 60% of the female students were stressed in contrast to 50% of the males, but
this observed difference was not statistically significant. The mental well-being and
social networking of stressed respondents suffered in comparison to their non-stressed
counterparts. CONCLUSIONS:The stress incidence in medical students in this institution
ORIGINAL ARTICLE
Departments of Pediatrics, and 1Pharmacology, Instituteof Postgraduate Medical Education and Research,Kolkata, 2Department of Pediatrics, North Bengal MedicalCollege, Darjeeling, 3 Department of Psychiatry, MedicalCollege, Kolkata, West Bengal, India
Address for correspondence:Dr. Madhumita Nandi,6/6, Naren Sarkar Road, Barisha,Kolkata - 700 008, India.
E-mail: [email protected]
Access this article online
Quick Response Code: Website:
www.indianjmedsci.org
DOI:
10.4103/0019-5359.110850
PMID:
*****************************
[Downloaded free from http://www.indianjmedsci.org on Saturday, January 02, 2016, IP: 125.161.213.32]
-
7/24/2019 IndianJMedSci6611-3703196_101711
2/12
2 INDIAN JOURNAL OF MEDICAL SCIENCES
Indian Journal of Medical Sciences, Vol. 66, No. 1 and 2, January and February 2012
INTRODUCTION
Stress in medical students is an established
phenomenon encountered worldwide and such
students seem to be under duress at all stages
of their academic career, including pre-clinical,
paraclinical, and clinical years.[1-4]Their overall
psychological distress is consistently higher
than in the general population and may impact
on their academic performance.[5,6]Stress may
foster anxiety, substance abuse, burnouts
leading to abandonment of studies, depression,
and even suicidal ideation.[3,7,8]
There are many possible stressors to which
medical students may be exposed. [9,10] The
pressure of a rigorous academic curriculumcoupled with frequent examination schedule
is an obvious factor. Various other perceived
sources of stress include personal factors
such as staying away from family, adjustment
to unfavorable hostel conditions, parental
expectations, etc., The medical education
system in India and the infrastructure in
medical colleges are generally not conducive
to amelioration of distress or facilitation of
coping. In fact, despite occasional reports,[11-14]
there are limited data regarding the magnitude
of the problem itself from the whole of the
country in general and eastern India in
particular. In view of the rapid pace at which
new medical institutions are coming up in India,
it is important to generate data regarding the
magnitude of student distress and its impact
on academic performance, dropout rates, and
professional development.
With this background, this study was conceived
as an analytical observational study to assess
the level of stress in medical students in a
teaching hospital in India, during various stages
of their MBBS course, and to identify factors
potentially responsible for inducing stress.
MATERIALS AND METHODS
The population for this study comprised all
undergraduate (MBBS) medical students of
3rd, 6th, and 9th (nal) semesters of the Institute
of Post Graduate Medical Education and
Research, Kolkata. All students present in theirrespective class on the day of the study were
included. The participants were informed about
the nature and purpose of the study and were
assured of condentiality. It was explained that
responding to the questionnaire was voluntary
and there would be no monetary or other direct
benets from participation. Written informed
consent was obtained from each participant.
Those who refused were to be excluded. The
study protocol received clearance from the
Institutional Ethics Committee.
Permission was taken beforehand from
the teacher concerned on the day of the
study and the last 25 min of a 1-h lecture
class was utilized for conducting the survey.
The students were not informed about the
in India is high and is negatively affecting their mental well-being. Further multicentric
and longitudinal studies are needed to explore the incidence, causes, and consequences
of stress in our setting.
Key words:28-item general health questionnaire, medical students, revised Lubben social
network scale, stress, student distress, WarwickEdinburgh mental well-being scale
[Downloaded free from http://www.indianjmedsci.org on Saturday, January 02, 2016, IP: 125.161.213.32]
-
7/24/2019 IndianJMedSci6611-3703196_101711
3/12
3STRESS IN MEDICAL STUDENTS
Indian Journal of Medical Sciences, Vol. 66, No. 1 and 2, January and February 2012
session beforehand. Those agreeing to
participate were asked to ll up a pretested
anonymous questionnaire to capture personal
data (excluding name and age), academic
performance, and stress inducing physical,
emotional, and social factors. These included
information on gender, percentage score in
last university examination, average monthly
family income, rural or urban background,
medium of study in school, whether staying
in hostel, and the number of siblings. The
rest of the questionnaire comprised three
checklists the 28-item General Health
Questionnaire (GHQ-28), WarwickEdinburgh
mental well-being scale (WEMWBS), andrevised version of the Lubben social network
scale (LSNS-R).
The GHQ-28[15,16]was used to assess current
mental health. This questionnaire was originally
developed by Goldberg et al. in 1979,[15] as
a 60-point screening questionnaire. Since
then it has been extensively used in different
sociocultural settings and in different abridged
forms. The GHQ-28 was designed from the
results of principal components analysis
based on the original GHQ. Its advantage
is that it assesses changes in individuals
daily functioning related to distress and not
personality characteristics. The GHQ-28
has four subscales: Depression, anxiety,
somatic symptoms, and social withdrawal.Each subscale contains seven items. The
respondent has to answer whether he or
she has experienced a particular symptom
or behavior recently. Each item is rated on a
four-point scale typically designated as not
at all, no more than usual, rather more than
usual, or much more than usual and the
bi-modal (0-0-1-1) scoring method is commonly
used to estimate the occurrence of stress
related to the item. Total score can range from
0 to 28. Total scores that exceed 4 out of 28
suggest caseness or distress. GHQ-28 is the
most well-known and popular version of the
GHQ. Adaptations of GHQ-28 have been used
in various countries and in various settings.[17-19]
The WEMWBS is a measure of mental
well-being focusing entirely on positive aspects
of mental health.[20,21] The scale consists of
14 items covering both hedonic and eudemonic
aspects of mental health including positive
affect (feelings of optimism, cheerfulness,
and relaxation), satisfying interpersonalrelationships and positive functioning (energy,
clear thinking, self-acceptance, personal
development, competence, and autonomy).
Respondents are required to select the
response that best describes their experience
of each statement over the past 2 weeks on a
5-point Likert scale none of the time, rarely,
some of the time, often, and all of the time.
All items are scored positively and the score
on each item ranges from 1 to 5. The overall
score is calculated as sum of the scores for
individual items, with equal weights, implying a
minimum possible score of 14 and maximum of
70. A higher WEMWBS score thus indicates a
higher level of mental well-being.
The LSNS-R was used to gauge perceivedsocial support received from family and friends.
It was originally developed in 1988 and was
revised in 2002.[22,23] The total score on this
scale comprises an equally weighted sum
of scores on 12 items used to assess size,
closeness, and frequency of contacts in a
respondents social network. All items measure
the level of perceived support received from
[Downloaded free from http://www.indianjmedsci.org on Saturday, January 02, 2016, IP: 125.161.213.32]
-
7/24/2019 IndianJMedSci6611-3703196_101711
4/12
4 INDIAN JOURNAL OF MEDICAL SCIENCES
Indian Journal of Medical Sciences, Vol. 66, No. 1 and 2, January and February 2012
either family or friends, and the scores on
each item range from 0 to 5, with 0 indicating
minimal social integration and 5 indicating
substantial social integration. The total score
can therefore range from 0 to 60, with higher
scores indicating a greater level of social
support and lower risk for isolation. A score
less than 20 may indicate that the person has
extremely limited social networking and is at
high isolation risk.
Statistical analysis
The data were rst transcribed to an MSExcel
spreadsheet and then analyzed by Statistica
version 6 [Tulsa, Oklahoma: StatSoft Inc.,2001] and MedCalc version 11.6 [Mariakerke,
Belgium: MedCalc Software, 2011] statistical
software. Scores were not normally distributed
and have therefore been summarized by
median and interquartile range, in addition to
mean and standard deviation. Key proportions
have been expressed with 95% confidence
interval (95% CI). Subgroup comparisons
have been done between the three semesters
and by baseline characteristics. Scores
have been compared between subgroups by
MannWhitney U test (for 2-group comparison)
or KruskalWallis analysis of variance followed
by Dunns test for post hoc comparison (for
more than 2-group comparison). Categorical
data have been compared between subgroups
by Fishers exact test, with FreemanHaltonextension where necessary. All analyses
have been two-tailed andP< 0.05 has been
considered statistically signicant.
RESULTS
The institute has approximately 100 students
per year. None of the students present in class
on the day of the study refused participation,
but the response sheets of only those who had
lled up all four sections of the questionnaire
were analyzed. The responses of 74 students
in 3rd semester, 40 students in 6thsemester,
and 101 students in the 9 th semester were
analyzed (Total n= 215).
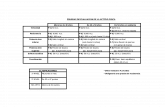
Table 1 shows the general characteristics
of the study population. It is noteworthy that
approximately 75% of the respondents were
male, 45% were coming from rural background,
25% from low-income (
-
7/24/2019 IndianJMedSci6611-3703196_101711
5/12
5STRESS IN MEDICAL STUDENTS
Indian Journal of Medical Sciences, Vol. 66, No. 1 and 2, January and February 2012
and 60% were unsatised with the available
social and recreational opportunities.
The frequency of these stressors was
equally applicable to all the three semesters
studied with few exceptions. Peer rivalry
appeared to peak during the nal semester
of study, while tension from political conicts
appeared to affect the 6thsemester students
most. There was no gender difference with
respect to the impact of these stressors, with
one exception. Of the 160 male students,
45 (28.13%) came from low-income families
in contrast to 8 (14.55%) of the 55 female
students (P = 0.047). Correspondingly,
52 (32.50%) of the male students felt
that financial constraints were negatively
influencing their academic performance,
in contrast to 9 (16.36%) of the female
students (P= 0.024).
There were no signif icant di f ferences
with respect to the occurrence of these
stress- inducing factors and basel ine
characteristics in the study participants, namely
with respect to ruralurban background,
stay in hostel versus home, English versus
vernacular medium background, and
presence or absence of siblings. However,
students from a rural background were more
Table 1: General characteristics of study cohort
Characteristic Overall(n=215) (%)
Semester 3(n=74) (%)
Semester 6(n=40) (%)
Semester 9(n=101) (%)
P value
Male gender 160 (74.42) 52 (70.27) 26 (65.00) 82 (81.19) 0.082
Rural background 95 (44.18) 28 (37.84) 14 (35.00) 53 (52.48) 0.071
Staying in hostel 152 (70.69) 54 (72.97) 24 (60.00) 74 (73.27) 0.270
Studied earlier in vernacular medium 129 (60.00) 42 (56.76) 20 (50.00) 67 (66.34) 0.156
From low-income families 53 (24.65) 14 (18.92) 10 (25.00) 29 (28.71) 0.342
No siblings at home 66 (52.80) 30 (40.54) 9 (22.50) 27 (26.73) 0.071
ThePvaluein the last column is from comparison between the three semesters by Fishers exact test (with Freeman-Haltonextension)
Table 2: Perceived frequency of individual stressors
Specifc question Overall(n=215) (%)
Semester 3(n=74) (%)
Semester 6(n=40) (%)
Semester 9(n=101) (%)
P value
Do you feel your socioeconomic status is coming inthe way of better performance in studies?
61 (28.37) 18 (24.32) 10 (25.00) 33 (32.67) 0.463
Are you satised with hostel/canteen facilities? 26 (12.09) 9 (12.16) 2 (5.00) 15 (14.85) 0.269
Are you satised with the library facilities? 49 (22.79) 20 (27.03) 6 (15.00) 23 (22.77) 0.347Are you satised with the examination system? 66 (30.70) 30 (40.54) 10 (25.00) 26 (25.74) 0.082
Do you feel there is excessive parental pressure toperform better?
31 (14.41) 10 (13.51) 7 (17.50) 14 (13.86) 0.816
Do you feel there is excessive competitive attitudeamong students?
137 (63.72) 46 (62.16) 24 (60.00) 67 (66.34) 0.732
Do you feel there is unhealthy peer rivalry andjealousy among students?
127 (59.06) 37 (50.00) 20 (50.00) 70 (69.31) 0.015
Do you feel the situation in the campus has becomeunhealthy due to excessive student politics?
174 (80.93) 58 (78.38) 38 (95.00) 78 (77.23) 0.030
Are you involved in a serious romantic relationship? 85 (39.53) 22 (29.73) 15 (37.50) 48 (47.52) 0.057
Are you satised with the social life/recreational
activities in college campus?
84 (39.06) 27 (36.49) 15 (37.50) 42 (41.58) 0.794
ThePvalue in the last column is from comparison between the three semesters by Fishers exact test (with Freeman-Haltonextension)
[Downloaded free from http://www.indianjmedsci.org on Saturday, January 02, 2016, IP: 125.161.213.32]
-
7/24/2019 IndianJMedSci6611-3703196_101711
6/12
6 INDIAN JOURNAL OF MEDICAL SCIENCES
Indian Journal of Medical Sciences, Vol. 66, No. 1 and 2, January and February 2012
likely than urban students to be staying in
hostel (P< 0.001), coming from a vernacular
medium background (P< 0.001), and belonging
to low-income families (P= 0.007), although
they did not feel that these factors impacted
their performance more than their urban
counterparts (32.63% for rural vs. 25.00% for
urban,P= 0.227).
On analyzing the GHQ-28 scores of the three
semesters separately, 35 students of 3 rd
semester (47.30%), 24 of 6thsemester (60.0%),
and 54 of 9 th semester (53.47%) scored
5 or more by bi-modal method. So a total
of 113 (52.56%; 95% CI 43.35-61.76%)students scored in the positive range of
stress by GHQ-28. Although the percentage
of stressed students in each semester was
quite high, there was no statistically signicant
difference in stress incidence on comparing
the three semesters (P= 0.480). By the same
parameter, 50% of the male respondents and
60% of the female respondents were stressed,
though this observed difference was not
statistically signicant (P= 0.214). As depicted
in Table 3, there was also no statistically
signicant difference in the incidence of stress
by the other baseline characteristics, with the
incidence being approximately 50% in each of
the baseline subgroups.
The numerical scores obtained by the various
instruments are summarized in Table 4.
With the exception of GHQ-28 anxiety
subscale score, which peaked in the final
semester and the LSNS-R friend component
score, which was least in the 6th semester,
there was no difference in scores across the
three semesters. There was no gender wise
difference in GHQ-28, WEMWBS, or R-LSNS
scores. There was also no signicant difference
in scores by ruralurban background, by hostel
versus home stay, low-versus high-income
families, and sibling status. In the R-LSNS
ratings, respondents who had studied in a
vernacular medium had higher median scorefor the family component and lower score
for the friends component than their urban
counterparts, and these differences were
statistically signicant (P= 0.014 and 0.040,
respectively). However, the median total scores
were comparable (P= 0.663).
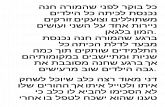
Finally, Table 5 summarizes the scores
obtained by stressed and non-stressed study
participants on the WEMWBS and revised
LSNS-R. As expected, the mental well-being
and social networking of stressed respondents
suffered in comparison to the non-stressed
students. Also, as expected, GHQ-28 total
score showed strong but negative correlation
Table 3: Frequency of stress occurrence (by score >4 on 28-item General Health Questionnaire) in various
baseline subgroups
Subgroup Number stressed (%) Subgroup Number stressed (%) P value
Male (n=160) 80 (50.00) Female (n=55) 33 (50.00) 0.214
Rural background (n=95) 54 (56.84) Urban background (n=120) 59 (49.17) 0.275
Staying in hostel (n=152) 81 (53.29) Staying at home (n=63) 32 (50.79) 0.766
Vernacularmedium (n=129)
45 (52.33) English medium (n=86) 68 (52.71) 1.000
Low-income family (n=53) 27 (50.94) Low-income family (n=162) 86 (53.09) 0.874
No siblings at home (n=66) 32 (48.48) Siblings at home (n=149) 81 (54.36) 0.461
ThePvalue in the last column is from comparison between the two subgroups concerned by Fishers exact test
[Downloaded free from http://www.indianjmedsci.org on Saturday, January 02, 2016, IP: 125.161.213.32]
-
7/24/2019 IndianJMedSci6611-3703196_101711
7/12
7STRESS IN MEDICAL STUDENTS
Indian Journal of Medical Sciences, Vol. 66, No. 1 and 2, January and February 2012
with the WEMWBS in the study cohort as a
whole [Figure 1] (Spearmans rank correlation
coefficient 8.21), although the correlation
with LSNS-R score was poor (Spearmans
rank correlation coefcient 3.11). There wasdirect and good correlation (Spearmans rank
correlation coefcient 5.04) between mental
well-being and social networking scores.
DISCUSSION
Assessing the stress burden in medical
students is important and such assessment
would be the rst step towards institution of
remedial measures. There is increasing interest
in the concept of positive mental health and
its contribution to all aspects of human life.
The World Health Organization has declared
positive mental health to be the foundation for
well-being and effective functioning for both
the individual and the community and dened
it as a state which allows individuals to realize
Table 4: Summary of scores obtained by study cohort on various study instruments
Scale Overall(n=215)
Semester 3(n=74)
Semester 6(n=40)
Semester 9(n=101)
P value
GHQ-28 somatic subscale score 2.01.98 2.02.09 1.0 1.51.58 2.12.02 0.223
1.0 (0.0-3.0) (0.0-3.0) 1.0 (0.0-2.0) 2.0 (0.0-4.0)
GHQ-28 anxiety subscale score 2.62.23 2.12.00 2.42.07 3.02.38 0.035
2.0 (1.0-4.0) 2.0 (0.0-4.0) 2.0 (1.0-4.0) 3.0 (1.0-5.0)
GHQ-28 social dysfunction subscale score 1.91.84 1.61.45 2.31.97 2.02.00 0.364
1.0 (0.0-3.0) 1.0 (0.5-2.0) 2.0 (0.5-4.0) 1.0 (0.0-3.0)
GHQ-28 depression subscale score 1.11.57 0.91.34 1.51.89 1.11.59 0.495
0.0 (0.0-2.0) 0.0 (0.0-1.0) 1.0 (0.0-2.5) 0.0 (0.0-2.0)
GHQ-28 total score 7.45.87 6.55.17 7.65.91 8.16.29 0.398
6.0 (2.0-12.0) 5.0 (3.0-8.0) 7.5 (2.0-11.5) 6.0 (2.0-13.0)
Warwick-Edinburgh mental well-being scale 50.310.92 50.79.24 47.89.87 51.012.33 0.093
51.0(44.0-58.0)
51.0(45.0-56.0)
49.0(42.0-54.0)
53.0(44.0-59.0)
Revised Lubben social network scale-familycomponent score
14.56.16 15.06.98 14.55.39 14.25.85 0.573
14.0
(11.0-19.0)
16.0
(9.0-20.0)
14.0
(11.0-19.0)
14.0
(11.0-17.0)Revised Lubben social network scale-friendscomponent score
18.05.89 19.95.13 16.76.4 17.25.90 0.005
18.0(15.0-22.0)
20.5(17.0-24.0)
18.0(12.0-21.0)
17.0(13.5-21.0)
Revised Lubben social network scale-totalscore
32.59.88 34.810.33 31.110.16 31.49.22 0.073
32.0(26.0-39.0)
35.5(27.0-43.0)
33.0(24.0-40.0)
31.0(27.0-37.0)
GHQ-28=General health questionnaire-28-item version, Values depict meanstandard deviation and median (interquartile range),TheP valuein the last column is from comparison between the three semesters by Kruskal-Wallis test
Table 5: Comparison of scores obtained by
stressed (by score >4 on 28-item General Health
Questionnaire) and non-stressed study participants
Specifc question Stressed(n=113)
Non-stressed(n=102)
P value
Warwick-Edinburgh mentalwell-being scale
46.610.78 54.49.59
-
7/24/2019 IndianJMedSci6611-3703196_101711
8/12
8 INDIAN JOURNAL OF MEDICAL SCIENCES
Indian Journal of Medical Sciences, Vol. 66, No. 1 and 2, January and February 2012
their abilities, cope with the normal stresses of
life, work productively and fruitfully, and make
a contribution to their community.[24,25] The
capacity for mutually satisfying and enduring
relationships is another important aspect of
positive mental health. Therefore in our study,
we assessed the stress burden in conjunction
with mental well-being and social networking.
There is no single universally accepted
instrument to quantify stress in medical
students. In addition to GHQ-28, various
other rating scales have been used, such as
the medical student stress prole[26] and the
Maslach burnout inventory-student survey.[27]
However, the later scales have not been
used widely in different sociocultural contexts.
Biomarkers have also been employed, such
as blood pressure, salivary cortisol, circulating
cytokines, and sperm count, but these are more
in the context of acutely stressful events such
as impending examinations.[12,28-30]
We therefore
settled for GHQ-28 which is not restrictive
to the context of an individual being solely a
medical student rather than a member of the
community in general. The GHQ is actually
available in multiple versions including 12,
28, 30, or 60 items. The 28-item version is
used most widely. This is not only because
of time considerations but also because
it has been used most widely in various
working populations, allowing for more valid
comparisons.
We included three different semesters
in our study as our intention was also to
examine whether the magnitude or profile
of stress change with advancement of the
academic career through predominantly
pre-cl in ical (3 rd semester 2 nd year),
mixed (6 th semester 3 rd year) , and
predominantly clinical (9thsemester 5thyear)
involvements. First-year medical students were
deliberately left out as we felt that they were
yet to be exposed to the full extent of the stressburden and were unlikely to have evolved
personal coping strategies. As it turned out, the
extent of stress and the possible determinants
appeared to be uniformly distributed for
students of all three semesters, unlike in an
earlier Indian study where stress was more
in the latter years compared to the 1styear of
study.[14]
This questionnaire-based survey revealed
a high rate of stress and emotional distress
in medical students, affecting 52.56% of
those studied. An earlier study on Indian
medical undergraduates, published more
than 10 years back, had revealed stress in an
even higher proportion (73%) of students. [14]
Studies from Iran[31]
and Saudi Arabia[32]
report
Figure 1: Scatter plot depicting correlation between28- i tem Genera l Hea l th Ques t ionna i re and
WarwickEdinburgh mental well-being scale scores inthe study cohort. The regression line is shown
[Downloaded free from http://www.indianjmedsci.org on Saturday, January 02, 2016, IP: 125.161.213.32]
-
7/24/2019 IndianJMedSci6611-3703196_101711
9/12
9STRESS IN MEDICAL STUDENTS
Indian Journal of Medical Sciences, Vol. 66, No. 1 and 2, January and February 2012
stress in over 60% of respondents. An US
study suggested psychiatric illness in 15-20%
of medical students needing some kind of
medical intervention.[33] A study on British
medical students, reported an incidence of
emotional disturbances in 31.2% of students.[34]
Some other studies have also revealed high
prevalence of depression and anxiety among
medical students, with levels of overall
psychological distress consistently higher than
in the general population.[4-8]
A higher percentage of female students
confessed to have stress compared to their
male counterparts, though the difference was
not statistically signicant. Some other studies
have also revealed higher prevalence of stress
in female students,[32-35] though the previously
mentioned Indian study does not reveal any
gender predilection.[14]Higher prevalence of
stress in female students could be due to their
experience of working in an environment still
largely populated by men than women, thoughthis scenario has changed considerably over
the years.
The possible inducers of stress in medical
students could be infrastructural factors such
as unsatisfactory living conditions in the hostel
and inadequate library facilities, academic
factors such as pressure of studies and
frequent examinations, and interpersonal
factors such as excessive competitive attitude
among students, political conicts, and jealousy
and peer rivalry over love affairs, all of which
could come in the way of natural friendship
and cooperation. Limited data are available
regarding the exact contribution of these
factors to student distress and its impact on
academic performance, dropout rates, and
professional development. [1,36] Low-income
family is another factor and socioeconomic
disparity among students, whether real or
perceived, could add to the difculties and the
emotional turmoil. However, it is noteworthy
that the extent of stress appeared to remain
at the same level in all the subgroups in our
study based on presence and absence of
these individual stressors. Such wide range of
stressors and additional ones have also been
reported in earlier studies. In a recent survey
on seven US medical schools, the authors
found a distinct relationship between pass/fail
grading and curriculum structure with well-being
among pre-clinical medical students.[37] The
British study identied talking to patients and
presenting cases, dealing with death and
suffering, and relationship with consultants
as common factors inducing stress in medical
students.[34]
Stress in medical students can have
professional ramications, including damagingeffects on empathy, ethical conduct, and
professional ism, as wel l as personal
consequences such as substance abuse,
burnouts, broken relationships, and suicidal
ideation. Therefore, it is the responsibility of
the society in general and medical schools
in particular, to acknowledge stress among
future doctors, identify sources of stress,
assess the individual students coping ability,
and undertake alleviatory measures.[38] Some
of the suggested stress reducing measures
could be improving the living conditions
and infrastructural facilities available to
students; reducing the incidence of campus
conicts; giving more importance to ongoing
academic performance rather than on marks
obtained in summative evaluations; and
[Downloaded free from http://www.indianjmedsci.org on Saturday, January 02, 2016, IP: 125.161.213.32]
-
7/24/2019 IndianJMedSci6611-3703196_101711
10/12
10 INDIAN JOURNAL OF MEDICAL SCIENCES
Indian Journal of Medical Sciences, Vol. 66, No. 1 and 2, January and February 2012
ensuring availability of well-trained student
counselors and specic programs to promote
stress resilience and self-care in medical
students. [2,4,6,39,40] Our study revealed a
direct correlation between mental well-being
and social networking scores. Therefore,
encouraging measures to improve social
networking on campus, such as college
festivals and sports, are also important
stress-alleviating measures. Efforts to reduce
student distress should be viewed as an
essential component of broader programs to
promote overall student well-being.
Our study has its share of shortcomings.
Although we included over 40% of the students
currently on our institutions rolls, conducting
the study as a multicentric survey would have
improved the generalizability of the ndings.
We were unfortunate that on the particular
survey date, we could obtain analyzable data
from
-
7/24/2019 IndianJMedSci6611-3703196_101711
11/12
11STRESS IN MEDICAL STUDENTS
Indian Journal of Medical Sciences, Vol. 66, No. 1 and 2, January and February 2012
2006;81:354-73.
2. Al-Dubai SA, Al-Naggar RA, Alshagga MA,
Rampal KG. Stress and coping strategies of
students in a medical faculty in Malaysia. Malays
J Med Sci 2011;18:57-64.
3. Dahlin M, Nilsson C, Stotzer E, Runeson B. Mental
distress, alcohol use and help-seeking among
medical and business students: A cross-sectional
comparative study. BMC Med Educ 2011;11:92.
4. Jurkat HB, Richter L, Cramer M, Vetter A,
Bedau S, Leweke F, et al. Depression and stress
management in medical students. A comparative
study between freshman and advanced medical
students. Nervenarzt 2011;82:646-52.
5. Haight SJ, Chibnall JT, Schindler DL, Slavin SJ.
Associations of medical student personality and
health/wellness characteristics with their medical
school performance across the curriculum. Acad
Med 2012;87:476-85.
6. Park J, Chung S, An H, Park S, Lee C, Kim SY,
et al. A structural model of stress, motivation,
and academic performance in medical students.
Psychiatry Investig 2012;9:143-9.
7. Prinz P, Hertrich K, Hirschfelder U, de Zwaan M.
Burnout, depression and depersonalisation-Psychological factors and coping strategies in
dental and medical students. GMS Z Med Ausbild
2012;29.
8. Fan AP, Kosik RO, Su TP, Lee FY, Hou MC,
Chen YA, et al. Factors associated with suicidal
ideation in Taiwanese medical students. Med
Teach 2011;33:256-7.
9. A l -Dabal BK, Koura MR, Rasheed P,
Al-Sowielem L, Makki SM. A comparative studyof perceived stress among female medical and
non-medical university students in Dammam,
Saudi Arabia. Sultan Qaboos Univ Med J
2010;10:231-40.
10. Hsieh YH, Hsu CY, Liu CY, Huang TL. The levels of
stress and depression among interns and clerks in
three medical centers in Taiwan: A cross-sectional
study. Chang Gung Med J 2011;34:278-85.
11. Behere SP, Yadav R, Behere PB. A comparative
study of stress among students of medicine,
engineering, and nursing. Indian J Psychol Med
2011;33:145-8.
12. Khaliq F, Gupta K, Singh P. Stress, autonomic
react iv i ty and b lood pressure among
undergraduate medical students. JNMA J Nepal
Med Assoc 2010;49:14-8.
13. Nagpal SJ, Venkatraman A. Mental stress among
medical students. Natl Med J India 2010;23:106-7.
14. Supe AN. A study of stress in medical students
at Seth G. S. Medical College. J Postgrad Med
1998;44:1-6.
15. Goldberg DP, Hillier VF. A scaled version of the
General Health Questionnaire. Psychol Med
1979;9:139-45.
16. Jackson C. The General Health Questionnaire.
Occup Med 2007;57:59.
17. Guthrie EA, Black D, Shaw CM, Hamilton J,
Creed FH, Tomenson B, et al. Embarking upon
a medical career: Psychological morbidity in rst
year medical students. Med Educ 1995;29:337-41.
18. Nagyova I, Krol B, Szilasiova A, Stewart RE,
van Djik JP, van den Heuval WJA. General Health
Questionnaire-28: Psychometric evaluation
of the Slovak version. Studio Pysholoiga2000;42:351-61.
19. Shariati M, Yunesian M, Vash JH. Mental health
of medical students: A cross-sectional study in
Tehran. Psychol Rep 2007;100:346-54.
20. Tennant R, Hiller L, Fishwick R, Platt S, Joseph S,
Weich S, et al. The Warwick-Edinburgh mental
well-being scale (WEMWBS): Development
and UK validation. Health Qual Life Outcomes
2007;5:63.21. Stewart-Brown S, Tennant A, Tennant R, Platt S,
Parkinson J, Weich S, et al. Internal construct
validity of the Warwick-Edinburgh mental well-being
scale (WEMWBS): A Rasch analysis using data
from the Scottish health education population
survey. Health Qual Life Outcomes 2009;7:15.
22. Lubben J, Gironda M. Measuring social networks
and assessing their benets. In: Phillipson C,
Allan G, Morgan D, editors. Social networks
[Downloaded free from http://www.indianjmedsci.org on Saturday, January 02, 2016, IP: 125.161.213.32]
-
7/24/2019 IndianJMedSci6611-3703196_101711
12/12
12 INDIAN JOURNAL OF MEDICAL SCIENCES
Indian Journal of Medical Sciences Vol 66 No 1 and 2 January and February 2012
and Social exclusion: Sociological and policy
perspectives. Farnham, Surrey, United Kingdom:
Ashgate Publishing Limited; 2004. p. 20-35.
23. Rubinstein RL, Lubben JE, Mintzer JE. Social
isolation and social support: An applied
perspective. J App Gerontol 1994;13:58-72.
24. Herman H, Saxena S, Moodie R, edi tors.
Promoting Mental Health: Concepts-emerging
evidence-practice: Summary Report. Geneva:
Department of mental health and substance abuse,
world health organization; 2004. Available from:
http://www.who.int/mental health/evidence/en/
promoting mhh.pdf. [Last accessed on 2012 Sep 3].
25. World Health Organization. Strengthening
mental health promotion [Fact Sheet No. 220],
2010. Available from: http://www.who.int/
mediacentre/factsheets/fs220/en. [Last accessed
on 2012 Sep 3].
26. ORourke M, Hammond S, OFlynn S, Boylan G.
The medical student stress prole: A tool for
stress audit in medical training. Med Educ
2010;44:1027-37.
27. Galn F, Sanmartn A, Polo J, Giner L. Burnout
risk in medical students in Spain using the
maslach burnout inventory-student survey. Int
Arch Occup Environ Health 2011;84:453-9.
28. Hulme PA, French JA, Agrawal S. Changes in
diurnal salivary cortisol levels in response to an
acute stressor in healthy young adults. J Am
Psychiatr Nurses Assoc 2011;17:339-49.
29. Kamezaki Y, Katsuura S, Kuwano Y, Tanahashi T,
Rokutan K. Circulating cytokine signatures in
healthy medical students exposed to academic
examinat ion st ress. Psychophysio logy
2012;49:991-7.
30. Lampiao F. Variation of semen parameters in
healthy medical students due to exam stress.
Malawi Med J 2009;21:166-7.
31. Koochaki GM, Charkazi A, Hasanzadeh A,
Saedani M, Qorbani M, Marjani A. Prevalence
of stress among Iranian medical students:
A questionnaire survey. East Mediterr Health J
2011;17:593-8.
32. Abdulghani HM, AlKanhal AA, Mahmoud ES,
Ponnamperuma GG, Alfaris EA. Stress and its
effects on medical students: A cross-sectional
study at a college of medicine in Saudi Arabia.
J Health Popul Nutr 2011;29:516-22.
33. Lloyd C, Gartrell NK. Psychiatric symptoms
in medical students. Compr Psychiatry
1984;25:552-65.
34. Firth J. Levels and sources of stress in medical
students. Br Med J 1986;292:1177-80.
35. Backovi DV, Zivojinovi JI, Maksimovi J,
Maksimovi M. Gender differences in academic
stress and burnout among medical students
in final years of education. Psychiatr Danub
2012;24:175-81.36. Dyrbye LN, Harper W, Durning SJ, Moutier C,
Thomas MR, Massie FS Jr, et al. Patterns of
distress in US medical students. Med Teach
2011;33:834-9.
37. Reed DA, Shanafelt TD, Satele DW, Power DV,
Eacker A, Harper W, et al. Relationship of
pass/fail grading and curriculum structure
with well-being among preclinical medical
students: A multi-institutional study. Acad Med2011;86:1367-73.
38. Dyrbye LN, Shanafelt TD. Commentary: Medical
student distress: A call to action. Acad Med
2011;86:801-3.
39. Jurkat H, Hfer S, Richter L, Cramer M, Vetter A.
Quality of life, stress management and health
promotion in medical and dental students.
A comparative study. Dtsch Med Wochenschr
2011;136:1245-50.40. Thomas SE, Haney MK, Pelic CM, Shaw D,
Wong JG. Developing a program to promote
stress resilience and selfcare in rstyear medical
students. Can Med Educ J 2011;2:e32-6.
How to cite this article:Nandi M, Hazra A, Sarkar S, MondalR, Ghosal MK. Stress and its risk factors in medical students: Anobservational study from a medical college in India. Indian J MedSci 2012;66:1-12.Source of Support: Nil. Conict of Interest:None declared.
[Downloaded free from http://www.indianjmedsci.org on Saturday, January 02, 2016, IP: 125.161.213.32]