5Antibiotic.pdf
-
Upload
dokezune-aun-lookchin -
Category
Documents
-
view
42 -
download
25
Transcript of 5Antibiotic.pdf
-
Antibiotic Smart Use: Interactive ShowcaseAntibiotic Smart Use: Interactive ShowcaseAntibiotic Smart Use: Interactive ShowcaseAntibiotic Smart Use: Interactive Showcase
-
..
..
MODERATORMODERATOR
-
.. ..
-
.. ..
-
. .
-
1 1. 4 1 .
.
4 Ph i l i ti Ab i d Physical examination: Abrasion wounds
at rt hand, no sign of inflammation
-
1 1. 4 1 .
.
4 Ph i l i ti Ab i d Physical examination: Abrasion wounds
at rt hand, no sign of inflammation
-
1 rabies vaccine rabies vaccine
-
1 rabies vaccine rabies vaccine
. Amoxicillin/clavulanate. cloxacillin. antibiotic
-
1 rabies vaccine rabies vaccine
. Amoxicillin/clavulanate. cloxacillin. antibiotic
-
Traumatic WoundsTraumatic Wounds Virtually all wounds are contaminated with bacteria, only a
small fraction (4.5-6.3%) developed traumatic wound
Best way to prevent wound infection Thorough wound cleansing
Appropriate closure (consider delayed primary closure in high-risk wound)
Radiographic imaging to evaluate foreign body
Appropriate antibiotic prophylaxis
Moran GJ, et al. Infect Dis Clin N Am 2008;22:117-43.
-
When to Give Prophylactic Antibiotics for Traumatic WoundWhen to Give Prophylactic Antibiotics for Traumatic Wound
Available data do not support prophylactic antibiotics in simple Available data do not support prophylactic antibiotics in simple wounds, but recommended in high-risk situations:
Immunocompromised patients (eg, poorly controlled p p ( g, p ydiabetes, steroid use, AIDS)
Open fractures or wounds into joints
Wounds involving tendons or cartilage
Grossly contaminated wounds that cannot be adequately y q ycleaned, esp. retained foreign body
Puncture wounds and crush injuries
Bite wounds
Oral wounds
Wounds with a significant delay (> 18 hours)Moran GJ, et al. Infect Dis Clin N Am 2008;22:117-43.
-
Prophylactic Antibiotics for Traumatic WoundProphylactic Antibiotics for Traumatic Wound Most settings for traumatic wound
Cloxacillin, dicloxacillin
1st cephalosporin: cephalexin
Grossly contaminated wounds, devitalized wound in immunocompromised patients:
Amox/clav
Intraoral wounds Penicillin 3-5 days for prophylaxis
7 10 days for treatment Bite wound Amox/clav
7-10 days for treatment of established infection
Moran GJ, et al. Infect Dis Clin N Am 2008;22:117-43.
-
Antimicrobial Agents for Animal Bite WoundsAntimicrobial Agents for Animal Bite WoundsSource of
BiteOrganism(s)
Likely to Cause Infection
Antimicrobial Agent
Oral Route Oral Alternatives
Intravenous Routeb,c
IV Alternatives for PenicillinAlternatives
for Penicillin-Allergy
Routeb,c for Penicillin-Allergy
D P ll A i illi E d d A i illi E d dDog, cat, or mammald
Pasteurella sp , S. aureus, Streptococci,anaerobes
Amoxicillin-clavulanate(Pasteurellaare resistant
Extended-spectrum cephalosporin or
Ampicillin-sulbactamf
Extended-spectrum cephalosporin or anaerobes,
Capnocytophagasp, Moraxella sp, Corynebacterium
are resistant to cephalexin, cloxacillin, erythromycin
or TMX-SMZ PLUSClindamycin
or TMX-SMZ PLUSClindamycinCorynebacterium
sp, Neisseria sp erythromycin, clindamycin)
Clindamycin ClindamycinORMeropenem
I f i f bi i hi h 50 80% i f i f d h bi
AAP. Redbook 2012
Infection after cat bites is as high as 50-80%; infection after dog or human bites are 10-15%
-
Antimicrobial Agents for Animal Bite WoundsAntimicrobial Agents for Animal Bite WoundsSource of Bite
Organism(s) Likely to
Cause
Antimicrobial Agent
Oral Route Oral Alternatives Intravenoub
Intravenous Infection for Penicillin-
Allergic Patientsas Routeb,c Alternatives for
Penicillin-Allergic Patients
Reptile Enteric gram-i
Amoxicillinl l
Extended-spectrum h l i
Ampicillin-lb f
ClindamycinSnegative
bacteria, anaerobes
-clavulanate cephalosporin or TMP-SMZPLUSCli d i
sulbactamf
PLUSGentamici
PLUSGentamicinORMClindamycin n Meropenem
AAP. Redbook 2012
-
Antimicrobial Agents for Human Bite WoundsAntimicrobial Agents for Human Bite WoundsS f O i ( ) A ti i bi l A tSource of
BiteOrganism(s)
Likely to Cause
Infection
Antimicrobial Agent
Oral Route Oral Alternatives for
Intravenous Routeb,c
Intravenous Alternatives for
Infection Penicillin-Allergic Patientsa
Penicillin-Allergic Patients
H S i A i illi E d d A i illi E d d Human Streptococcisp. Esp. Streptococcus
i
Amoxicillin-clavulanate
Extended-spectrum cephalosporin
Ampicillin-sulbactamf
Extended spectrum cephalosporin or TMP SMZanginosus,
S. aureus, Eikenellacorrodens
or TMP-SMZPLUSClindamycin
TMP-SMZPLUSClindamycinORcorrodens,
Haemophilussp, anaerobes
Clindamycin ORMeropenem
AAP. Redbook 2012
-
* ( 6 . )* ////
()
() () ()
() 6 . 5 .
() /
/
steroid
Amoxicillin-clavulanate (500:125) 30-
steroid
50 mg/kg/day 2 Ciprofloxacin
+ Clindamycin ( metronidazole)
Dicloxacillin 25 mg/kg/day 4 Cephalexin 25-50 mg/kg/day 3 Roxithromycin Clindamycin
3
-
Amoxicillin/Amoxicillin/ClavulanateClavulanate PreparationsPreparations
SyrupSyrup 4:1 Amox/Clav 156 (125/31)
7 1 A /Cl 228 (200/28) 7:1 Amox/Clav 228 (200/28)Amox/Clav 457 (400/57)
14:1 Amox/Clav ES (600/42.9) 14:1 Amox/Clav ES (600/42.9)
TabletTablet 2:1 Amox/Clav 375 (250/125) 4:1 Amox/Clav 625 (500/125)
7 1 A /Cl 1 G (875/125) 7:1 Amox/Clav 1 G (875/125) 14:1 Amox/Clav SR (1000/62.5)
-
2 2. 13 - year- old boy, underlying Ewing sarcoma left femur post incision biopsy Last ChemoRx 7 days before 1 day PTA, He developed high grade of fever and decreased appetite At ER he was found to be hypotensive and tachycardiaPhysical ExaminationPhysical Examination V/S: T 39.3o C, P 150/min (not full), BP 70/40 mmHg, RR 25/min G/A: drowsiness, mild pale, capillary refill 4 sec Left femur: mild swelling, no redness Other : WNL
-
2He received NSS load 20cc/kg/dose x 2 dose, dopamine 20 mcg/kg/min and then transfer to ICUInvestigation CXR: no definite pulmonary infiltration CBC :Hb 7.7 g/dl, Hct 22.8% WBC
100 cell/mm3 (N 26.9 %, L ( ,10.2%, Mo 62%, Eo 0.9%), ANC 0 plt 12 000 cell/mm30, plt. 12,000 cell/mm
U/A : PH 6.5, sp.gr. 1.010, protein C 0 1 /neg, sugar neg, WBC 0-1 /HPF
, RBC 0 /HPF Lactate 9.7 mmol/L
-
2Which is the appropriate empirical Which is the appropriate empirical antibiotic treatment in this patient ?antibiotic treatment in this patient ?
-
2Which is the appropriate empirical Which is the appropriate empirical antibiotic treatment in this patient ?antibiotic treatment in this patient ? Ceftazidime + amikacin. Ceftazidime + amikacin Meropenem. Meropenem Piperacillin tazobactam + vancomycin. Piperacillin-tazobactam + vancomycin
-
2Which is the appropriate empirical Which is the appropriate empirical antibiotic treatment in this patient ?antibiotic treatment in this patient ? Ceftazidime + amikacin. Ceftazidime + amikacin Meropenem. Meropenem Piperacillin tazobactam + vancomycin. Piperacillin-tazobactam + vancomycin
-
Initial assessment and investigations1 P f i d lli IV th t 1. Presence of indwelling IV catheters 2. Symptoms or signs suggesting an infection focus
Respiratory system GI Skin Perineal region/GU Oropharynx CNSRespiratory system, GI, Skin, Perineal region/GU, Oropharynx, CNS3. Previous positive microbiology results 4 Routine investigations4. Routine investigations
Blood testing to assess bone marrow, renal and liver function, Coagulation screen, CRP, Blood cultures including cultures from indwelling IV catheter, Urinalysis and culture, g g ySputum microscopy and culture, Stool microscopy and culture, Skin lesion (aspirate/biopsy/swab), CXR
5. Further investigations (profound/prolonged neutropenia/following allografts)
( )High-resolution chest CT (despite 72 h of appropriate antibiotics) Broncho-alveolar lavage
-
Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2012 Intravenous ATB administration within 1 hour of recognition of septic shock (grade 1B) and severe sepsis recognition of septic shock (grade 1B) and severe sepsis without septic shock (grade 1C) The choice of empiric antibiotics for febrile neutropeniashould be based on local antibiotic susceptibility datashould be based on local antibiotic susceptibility data.
Clinical Guideline for NICE by the National Collaborating Centre for Cancer (2012)Critical Care Medicine 2013 ; 41( 2) :580-637
-
Empirical Antibiotic For Serious Systemic InfectionsIn nosocomial acquired or suspect resistant GNR and life threatening, immunocompromised host
C
In nosocomial acquired but not life threatening or i i d i h d i
Carbapenem
community acquired with suspected resistance BL inhibitor (Cefoperz/sulbact, Pip/taz) 4th Gen Cephalosporin
In community acquired and normal host 3rd Gen Cephalosporin*
4 Gen. Cephalosporin
3 Gen. Cephalosporin
May add aminoglycoside in more seriousAdd V if t MRSA Add Vanco. if suspect MRSA
Add Metronidazole if suspect anaerobes
-
http://www.ped.si.mahidol.ac.th/
-
Evaluation of guideline for treatment of febrile neutropenia in pediatric cancer at Siriraj Hospital.
A total of 148 FN episodes in 90 patients
62% responded to initial treatment without changing of antibiotics
p j p
patients The predominant underlying
malignancy was acute leukemia. About
without changing of antibiotics. Of all episodes, 91.2% were able to
complete treatment according to the g y50% had ANC less than 100 cells/mm3 at the beginning and at
p gCPG.
The mortality rate was 1.4%. reassesment on day 3 of treatment.
The causes of infection with ANC
-
Progression Progression
H/C (16/6/56) H/C (16/6/56) P. aeruginosa
H/C (17/6/56): NG U/C (17/6/56): NG
Treatment Meropenem x 7 days + Amikacin x 5 days
Ceftazidime x 7 days
-
Pseudomonas aeruginosa Bloodstream Infection: Importance of Appropriate Initial Antimicrobial Treatment
I i i i i l i i bi l Inappropriate initial antimicrobial treatment as an independent predictor for hospital mortality (30.7% versus 17.8%; P = 0.018).
Initial treatment with combination antimicrobial agents directed against P. aeruginosa was statistically more g g ylikely to provide appropriate treatment than was
thmonotherapy.Antimicrob Agents Chemother 2005; 49:1306-1311
-
3 3. 2 3
trauma Physical Examination
T 38o C, AF 2x2 cm no bulging, g g Right hip : warm and swelling, decrease movement of right leg
screaming when passive movement of right hip Others: unremarkableOthers: unremarkable
-
3Investigation g CBC (30/8/56): Hb 12 g/dl, Hct 36% WBC 18,900 CBC (30/8/56): Hb 12 g/dl, Hct 36% WBC 18,900
cell/mm3
(N 73.1%, L 20.6%, Mo 5.1%, Eo 0.9%,Ba 30.3%), plt. 420,000 cell/mm3
ESR 84 mm/hr CRP 26 06 mg/L ESR 84 mm/hr, CRP 26.06 mg/L H/C : pendingH/C : pending
-
3Film both hip
U/S Hip : joint effusion in right hip
-
3 antibiotics
-
3 antibiotics
. Cloxacillin. Cefazolin. Cefotaxime
-
3 antibiotics
. Cloxacillin. Cefazolin. Cefotaxime
-
Septic arthritisCli i l if t ti Clinical manifestations: Neonates and young infantseo ates a d you g a ts Septicemia or fever without a focus Joint or extremity: swelling, red, warm Pain: limitation of use of the involved extremity
(pseudoparalysis), pain on manipulationp p y p p Postural changes: positional preferences
Hip: flex and externally rotate
-
Septic arthritis: M l i hild < 3 More commonly in children < 3 years. Boy: girl 2:1 Mode of infection:
Hematogenous spread: most commonHematogenous spread: most common Contiguous spread: complication of osteomyelitis.
Infection from the metaphysis to the joint by transphysealvessels. (obliterate by 18 mo of age) Some joint capsules cover the metaphysis: hip, shoulder, elbow and ankle
Direct inoculationBone and joint infections in children. Pediatr Clin N Am 2005
-
Septic arthritis: Site of infection:
Monoarticular joint involvement: > 90%C it hi k d kl Common sites: hip, knee, and ankle
Polyarticular involvement: Polyarticular involvement: Neonates N. gonorrhea, N. meningitidis, Salmonella spp.
And occasionally S. aureus
-
Investigations Leukocytosis: 20-35% of cases ESR and CRP: elevated in most patients
CRP: peaks within 36 -50 hr of onset of infection normal within 7-10 days of successful treatment
ESR: peaks within 3-5 days of onset of infection normal within up to 30 days of successful treatment
Blood culture: positive in approximately 40 % Synovial fluid:
WBC count >50,000 cells/microL, with a predominance (>90%) of polymorphonuclear cellsC l i i i i l 0 60% Culture: positive in approximately 50 to 60%
Confirmed bacterial etiology in 50-70% of cases
unkila-kallio L, et al. Pediatrics 1993;92(6):800-4 Pkknen M, Peltola H. Pediatr Clin North Am. 2013 ;60(2):425-36
-
Imaging Investigations Plain radiographs:
widening of joint space capsular swelling evidence of widening of joint space, capsular swelling evidence of osteomyelitis
Ultrasonography: Useful and more available to detect joint effusion
Magnetic resonance imaging (MRI): Magnetic resonance imaging (MRI): Highly accurate for detecting of joint effusion, but not
practical.
-
Septic arthritisAge Common pathogen Empirical AntibioticsAge Common pathogen Empirical Antibiotics
0-3 mo Staphylococcus aureusStreptococcus agalactiae
antistaphylococcal agent (vancomycin ornafcillin/oxacillin) +p g
Gram-negative enteric bacteriaNeisseria gonorrheaC did
3rdgen.cephalosporin eg: cefotaxime orgentamicin
Candida< 5 y Staphylococcus aureus
Streptococcus pyogenes Age < 2 y3rdgen cephalosporin: cefotaxime +/-Streptococcus pyogenes
Salmonella sppStreptococcus pneumonia
3 gen.cephalosporin: cefotaxime /gentamicin Age 3-5 y
Kingella kingaeHaemophilus influenza type b
Cloxacillin or Cefazolin +/- gentamicin
>5 y Staphylococcus aureus Cloxacillin or cefazolin +/ gentamicin (severe >5 y Staphylococcus aureusStreptococcus pyogenes
Cloxacillin or cefazolin +/- gentamicin (severe case)
Neisseria gonorrhea(sexually active adolescents)
Cefotaxime or ceftriaxone
-
Surgical Treatment Indication for arthrotomy :
f Prompt drainage for hip and shoulder Large amount of fibrin debris or loculationsLarge amount of fibrin debris or loculations Concomitant with osteomyelitis Lack of clinical improvement after 48 hours of
tibi ti th i t t iti lt antibiotic therapy or persistent positive cultures despite appropriate antimicrobial therapy and multiple needle aspirations
-
Sequential Oral Antibiotic Therapy Good clinical response to parenteral antibiotics:
Afebrile for 48 to 72 hours Local signs and symptoms of infection are reduced considerably.g y p y Normal peripheral leukocyte count
D ESR d CRP l l Decrease ESR and CRP level.
Usually after 7 -10 days of intravenous therapy. Ability to swallow, retain, and absorb an appropriate oral medication. I t t l tibi ti f ti In neonates: parenteral antibiotics for entire course
-
Duration of Therapy Generally 2 - 6 weeks depending on
Organism: S aureus 3 wks S. aureus 3 wks S. pneumoniae, K. kingae, or N. meningitidis 2-3 wks Enterobacteriaceae or other unusual organisms: longer course
Clinical resolution of signs and symptoms: Clinical resolution of signs and symptoms: Longer duration in hip
Resolution of inflammatory markers.
-
History Treatment y OR: Arthrotomy Rt. hip Finding: g
Pus in right hip 2 ml Medial femoral head cartilage have Medial femoral head cartilage have
some destruction Anterolateral cartilage smooth and g
whitish surface
Pus from Rt.hip p E.coli, ESBL neg
H/C : no growthH/C : no growth Stool c/s : no growth
-
Progression Treatment
Cefotaxime (300 MKD) x 4 wk Cefotaxime (300 MKD) x 4 wk. +Amikacin (15 mkd) x 5 days
30/8 6/9 13/9 20/9 27/9ESR 84 95 61 54 20CRP 26.06 32.47 7.92 4.1 0.18
f/u film hip : normal alignment , no bony destruction
-
Septic ArthritisLong-term complications
Avascular necrosisRisk factors for long-term complications
Age < 6 months Limb length disparities Pseudarthrosis (false joint)
Concomitant osteomyelitis Involvement of high risk joints: hip or Pseudarthrosis (false joint)
Joint dislocations and joint deformity
Involvement of high risk joints: hip or shoulder
Delay in appropriate initial management deformity Delay in appropriate initial management (decompression and initiation of antibiotics) by 4 days or longerantibiotics) by 4 days or longer.
Enterobacteriaceae and S. aureusGutierrez KM. In:Long SS, Pickering LK, Prober CG, eds.
Principles and Practiceof Pediatric InfectiousDiseases,3rd ed . 2009:484492
-
4 4. 2 6
2 BT 39.5 oC, others : unremarkable CBC : Hb 12 g/dl, Hct 36%, wbc 10,300 cells/mm3(N 70, L 28, M
2), platelet 276,000 UA : WNL Hemoculture Hemoculture
24
Hemoculture Streptococcus pneumoniae
-
4
-
4
hemoculture oral amoxicillin
. hemoculture , oral amoxicillin 80-90 mg/kg/d 24 .g g
. hemoculture , 24 . , hemoculture ,
Ceftriaxone 50 mg/kg IV
-
4
hemoculture oral amoxicillin
. hemoculture , oral amoxicillin 80-90 mg/kg/d 24 .g g
. hemoculture , 24 . , hemoculture ,
Ceftriaxone 50 mg/kg IV
-
Management of a Previously Management of a Previously Healthy Infant (Healthy Infant (2828--90 90 Days) with Days) with Healthy Infant (Healthy Infant (2828 90 90 Days) with Days) with
FWS (T FWS (T >> 3838..00c)c)
Baraff LJ. Ann Emerg Med 2000;36:602-614.
-
LowLow--risk Criteria for Febrile Infantsrisk Criteria for Febrile Infants
Clinical criteria Previously healthy term infant
Laboratory criteria WBC count 5 000Previously healthy, term infant
with uncomplicated nursery stay
Nontoxic clinical appearance
WBC count 5,00015,000/mm3,
-
Management of a Previously Healthy Child (3 36 months) Healthy Child (3-36 months)
with FWS
Baraff LJ. Ann Emerg Med 2000;36:602-614.
-
The Child not Appear Toxic, T > 39oC
Baraff LJ. Ann Emerg Med 2000;36:602-614.
- Active prospective, hospital-based surveillance study (2008-2009) p p , p b d dy ( ) Fever without a Source in Thai Infants and Children 28 days to
-
Occult Pneumococcal Occult Pneumococcal BacteremiaBacteremiaM j i f hild i h l l b i Majority of children with occult pneumococcal bacteremiaresolves without therapy
A t ti i f th Child H it l i A retrospective review from the Childrens Hospital in Boston, children with occult pneumococcal bacteremia
No ATB Received ATB
Persistent fever 76.1% 23.9%
Persistent bacteremia 17.0% 1.6%
Hospitalization 50.0% 11.7%
Lee GM, et al. Arch Pediatr Adolesc Med. 1998;152:624-628.
-
Risk of Bacterial Meningitis in Occult Risk of Bacterial Meningitis in Occult BacteremiaBacteremia
Baraff LJ. Ann Emerg Med 2000;36:602-614.
-
Revisit for Occult Pneumococcal Revisit for Occult Pneumococcal BacteremiaBacteremia Febrile : Children who were well but persistently febrile at the Febrile : Children who were well, but persistently febrile at the
revisit and did not receive antibiotics at the initial visit 33-42 % chance of persistent bacteremia
4.4 % chance of meningitis
4% chance of meningitis despite initial oral antibiotic therapy
High risk of SBI in patients with + H/C for S. pneumoniae who are febrile on revisit
Sh ld d f ll i l ti ( id LP i i f t )Should undergo a full sepsis evaluation (consider LP in infants)
Should receive parenteral antibiotics tailored to susceptibility
Oral antibiotic may be an alternative y
Total duration 7-10 days
Bachur R, et al. Pediatrics 2000;105:502-9.
-
Revisit for Occult Pneumococcal Revisit for Occult Pneumococcal BacteremiaBacteremia
Afebrile : Well-appearing, afebrile children who did not receive antibiotics at the initial visit with + H/C for S. pneumoniae ~ 9 % risk of persistent bacteremia
Another H/C before antibiotic therapy p
Can be managed with antibiotics as an outpatient with close F/U
Antibiotic regimens should provide coverage for resistant g p gS. pneumoniae
Bachur R, et al. Pediatrics 2000;105:502-9.
-
Antimicrobial Susceptibility of Antimicrobial Susceptibility of S. S. pneumoniaepneumoniae Isolates Causing IPD, Isolates Causing IPD, Central Thailand, Central Thailand, 20092009--20122012
Antimicrobial agents n Susceptibility (%)
Susceptible Intermediate Resistant
Penicillin 234 89 7 6 0 4 3Penicillin 234 89.7 6.0 4.3
Cefotaxime 234 95.7 2.6 1.7
Cefditoren*,# 82 90.2 6.1 3.7
Cefdinir# 80 50.0 7.5 42.5
Erythromycin 193 45.6 3.1 51.3
Azithromycin# 82 26 8 1 2 72 0Azithromycin# 82 26.8 1.2 72.0
Clarithromycin# 82 26.8 6.1 67.1
Clindamycin 34 67.7 0.0 32.3
Tetracycline 99 41.4 0.0 58.6
TMP-SMZ 145 32.4 9.0 58.6
Ofl i 95 97 9 1 0 1 1Ofloxacin 95 97.9 1.0 1.1
Levofloxacin 14 100.0 0.0 0.0
Linezolid 95 97.9 0.0 2.1
Vancomycin 131 100 0.0 0.0
Phongsamart W, et al. The 31st ESPID Meeting, Milan, Italy, May 28 - June 1, 2013
-
5 5. A 4-year-old girl who has a chronic tracheostomy due to subglottic stenosis 3 days PTA she developed high grade fever with increased respiratory
distress, purulent tracheal secretions. History of recurrent hospitalizationPhysical examinationPhysical examination T39.5 o c, P 120/min (full), BP 100/60 mmHg, RR 40/min G/A: looked sick, dyspnea, tachypnea, subcostal retraction HEENT: pharynx mild injection, Lungs: coarse crepitation at right lung
-
5Investigation
CBC : Hb 12.3 g/dl, H t 35 1% WBC 16 000 / 3 Hct 35.1%, WBC 16,000 /mm3
(N 71%, L22%, Mo7%), plt. 339,000/ mm3
Sputum from treachalSputum from treachalsecretions: Gram stain reveals numerous WBC and gramnumerous WBC and gram-negative rods
Chest X-ray: as shown
-
5What is the BEST choice for empiric What is the BEST choice for empiric
tibi ti th f thi ti t? antibiotic therapy for this patient?
-
5What is the BEST choice for empiric What is the BEST choice for empiric
tibi ti th f thi ti t? antibiotic therapy for this patient? . Ampicillin-sulbactam. Piperacillin-tazobactam. Clindamycin+Ceftriaxone
-
5What is the BEST choice for empiric What is the BEST choice for empiric
tibi ti th f thi ti t? antibiotic therapy for this patient? . Ampicillin-sulbactam. Piperacillin-tazobactam. Clindamycin+Ceftriaxone
-
Comparison of antibacterial spectraAmp/Sulb Pip/Tazo Ceftriaxone
Serratia sp. 0 + +Proteus mirabilis + + +Citrobacter sp 0 + +Citrobacter sp. 0 + +Aeromonas sp. + + +Ps. aeruginosa 0 + +
E. coli/Klebs sp. ESBL+ 0 + 0Enterobacter sp. 0 + +Acinetobacter sp + + 0Acinetobacter sp. + + 0
The Sanford Guide to Antimicrobial Therapy 2012
-
Treatment outcome of TAZ/PIPC and SBT/ABPC as initial i i l th f i ti i d empirical therapy of aspiration pneumonia caused
by Klebsiella pneumoniae (NI)
TAZ/PIP group SBT/ABP group pEffective rate 91.7% (11/12) 25.0% (3/12) 0.003Survival rate 91 7% (11/12) 58 3% (7/12) 0 155Survival rateAfter 30 days
91.7% (11/12) 58.3% (7/12) 0.155
Early treatment success rate
91.7% (11/12) 41.7% (5/12) 0.027
J Infect Chemother (2012) 18:715721.
-
6 6. 3 5 2
Physical examination
o V/S : T 38o c, P 110/min, BP 100/60 mmHg, RR 30 /min G/A : Alert, mild dyspnea HEENT : pharynx mild injection, no oral ulcer, no conjunctivitis
RS : fine crepitation on both lungs decreased breath sounds RS : fine crepitation on both lungs, decreased breath sounds on RLL,
-
6
-
6CXR
-
6Investigation Investigation CBC Hb 10 9 /dl H t 32 6% WBC CBC: Hb 10.9g/dl, Hct 32.6%, WBC
6 530/mm3 (N 53 2% L 42 9% Mo 6,530/mm (N 53.2%, L 42.9%, Mo 3.5%, Eo 0.2%, Ba 0.2%), Plt. 3 5%, o 0 %, a 0 %),199,000/mm3
-
6
-
6
. Levofloxacin. Cefotaxime + azithromycin + oseltamivir. Cefotaxime + azithromycin
-
6
. Levofloxacin. Cefotaxime + azithromycin + oseltamivir. Cefotaxime + azithromycin
-
Community-Acquired Pneumonia (CAP) in ChildhoodEtiologic agents:Etiologic agents: Viruses: most common pathogens30% - 67% of cases esp. in
children < 1 yr (77%) Bacteria:
Streptococcus pneumoniae and Haemophilus influenzae type b (Hib) t (Hib): most common
Mycoplasma pneumoniae and Chlamydia pneumoniae: up to 1/3 of cases.Bacteremia: < 10%
23%- 33% of cases of pneumonia mixed bacterial and viral infections. Bacteremia: < 10%
Michelow IC, et al. Pediatrics 2004;113(4):7017.Cilla G, et al. J Med Virol 2008;80(10):18439.
mixed bacterial and viral infections.
-
Microbial causes of CAP in childhoodAge Etiologic agents
Birth-3 weeks Group B streptococci p pGram-negative enteric bacteriaListeria monocytogenesy g
3 wk3 mo Chlamydia trachomatisRSV RSV Parainfluenza viruses esp.type 3 Streptococcus pneumoniaeStreptococcus pneumoniaeStaphylococcus aureusBordetella pertussisBordetella pertussis
Pediatr Clin N Am 60 (2013) 437453.
-
Age Etiologic agents4 mo- 4 y RSV, parainfluenza viruses, influenza virus,
adenovirus, rhinovirusHaemophilus influenzaeStreptococcus pneumoniaeMycoplasma pneumoniaeMycobacterium tuberculosis
5-15 y Mycoplasma pneumoniaeChlamydia pneumoniaeChlamydia pneumoniaeStreptococcus pneumoniae Influenza A or B, adenovirus adenovirus Nontypeable Haemophilus influenzaeMycobacterium tuberculosisMycobacterium tuberculosis
Pediatr Clin N Am 60 (2013) 437453.
-
Incidence and Etiology of ALRI in Hospitalized Children < 5 yrin Sa Kaeo and Nakhon Phanom, Thailand.,
N = 28,543 hospitalizations from 2005-2010 Blood cultures were collected from 28% of cases (n= 7,975)
( ) 1.8% (n=145) were positive blood cultures. Most common pathogens:
Salmonella, non-typhoid 15%Streptococcus pneumoniae 13% Streptococcus pneumoniae 13%
Haemophilus influenzae 10%
Hasan R, et al. PIDJ 2013 Sep 11 [Epub ahead of print] E.coli 9%
-
Incidence and Etiology of ALRI in Hospitalized Children < 5 yr
25Hospitalized Children < 5 yr
in Sa Kaeo and Nakhon Phanom, Thailand.
16.7
20
16
17.9
16
20
St t i
n=145
11 91212 11 9
1616
11 9
15
Streptococcus pneumoniae
Escherechia coli
Haemophilus influenzae
Acinetobacter baumanii11.9
7 7
12
10.3
12 11.9
8 7 7
11.9
10
Acinetobacter baumanii
Salmonella, non-typhoid
Staphylococcus aureus
Klebsiella spp
4
7.7
4.8
7.1
3.8
7.1
3.8
7.1
4.8
7.7
4.85
Moraxella cattarrhalis
Burkholderia pseudomallei
2.6
0 01.3
00
-
Mycoplasma pneumoniae and Chlamydophila pneumoniae in children with community-acquired pneumonia in Thailandwith community acquired pneumonia in Thailand A prospective surveillance study: Dec 2001- Nov 2002 N 245 2 15 N = 245, age: 2-15 yr. 17.5% of CAP (n=43) were caused by atypical pathogens.
46 5% (20/43) were children aged 2 5 yr 46.5% (20/43) were children aged 2-5 yr. Rates of current infection:
M pneumoniae 14 3%M. pneumoniae 14.3%C. pneumoniae 2.8%Coinfection 0 4%Coinfection 0.4%
Among children with CAP: prevalence of atypical pneumonia Age 2-5 yr 11% Age 2 5 yr. 11% Age > 5 yr. 36% S. Lochindarat, et al. INT J TUBERC LUNG DIS 2007;11(7):814819
-
Parapneumonic effusion 2%12% children with pneumonia developed
parapneumonic effusions. most frequently (50%) related to bacterial pneumoniamost frequently (50%) related to bacterial pneumonia
S. pneumoniae, S. pyogenes, S. aureus and H. influenzae type b
Up to 20% of mycoplasma pneumonias. 10% of viral pneumonias 10% of viral pneumonias.
IDSA Guidelines CID 2011;53(7):e25.
-
Mycoplasma pneumonia:extrapulmonary involvement
skin: erythematous maculopapular rash, erythemanodosum or urticaria to the Stevens Johnson nodosum or urticaria to the Stevens-Johnson syndrome.
Other extrapulmonary manifestations: Hemolytic
anemia polyarthritis pancreatitis hepatitis pericarditianemia, polyarthritis, pancreatitis, hepatitis, pericarditis, myocarditis, and neurologic complications
-
Empiric Therapy for Pediatric Community-Acquired Pneumonia (CAP)All age Bacterial pneumonia Atypical pneumonia Influenza
pneumoniaFully immunized : Hib, PCV Penicillin resistance in
Ampicillin or penicillin G;alternatives:ceftriaxone or
If atypical pneumonia in doubt Add AzithromycinOR
Oseltamivir or zanamivir
Penicillin resistance ininvasive strains ofpneumococcus is
ceftriaxone or cefotaxime
ORClarithromycinErythromycin,
minimal Doxycycline for children.> 7 y Levofloxacin
Not fully immunizedPenicillin resistance in
Ceftriaxone or cefotaxime
As above As above
invasive strains ofpneumococcus is significantsignificant
IDSA Guidelines CID 2011;53(7):e25.
- Antimicrobial Susceptibility of S. pneumoniae, Siriraj Hospital, 2008N 170 (32 4% f hild 5 )N=170(32.4%fromchildren
-
Progression Cefotaxime Ciprofloxacin Cefotaxime
AzithromycinCiprofloxacin
-
Follow upFollow up
TreatmentCefotaxime+ Azithromycin x 5 days
Ciprofloxacin x 7 days
Mycoplasma titers 1: 1280 1wk later Mycoplasma titer > 1: 20,480
-
Macrolide-Resistant Mycoplasma pneumoniae (MRMP) First isolated from pediatric patients in 2000. Mutation at A2063G A2063T or A2064G of the 23S ribosomal RNA Mutation at A2063G, A2063T, or A2064G of the 23S ribosomal RNA
gene confers high resistance to macrolides (MIC90 > 64) Prevalence of MRMP:
In Japan (children): 5.0% in 2003 to 87% in 2011 In Korea: 2.9% in 2003 to 63% in 2011
In China (children & adult): > 80% In China (children & adult): > 80% In U.S.: 8.2% In Europe: 3% in Germany, 10% in France, 26% in Italy and 32% in Israel
-
Macrolide-Resistant Mycoplasma pneumoniae(MRMP) Infection in a 2011Outbreak Among Japanese Childrenin a 2011Outbreak Among Japanese Children
Among 202 M. pneumoniae isolates from M pneumoniae associated pneumonia patients M. pneumoniaeassociated pneumonia patients,
176(87.1%) were MRMP.
Takafumi Okada, et al. CID 2012:55:1642-9
-
7 7. 3 1 .
3 PE: T 38.5oC, Lt. ear: tympanic membrane:
injected and mild bulging injected and mild bulging, no perforation p
Others : WNL
-
7
-
7
. Cefdinir. Amoxicillin/clavulanate, 90 mg/kg/day of
amoxicillin. Amoxicillin 50 mg/kg/day
-
7
. Cefdinir. Amoxicillin/clavulanate, 90 mg/kg/day of
amoxicillin. Amoxicillin 50 mg/kg/day
-
Diagnosis of AOM Clinicians should diagnose AOM in children who present with (B)
Moderate to severe bulging of the TMNew onset of otorrhea not due to acute otitis externa New onset of otorrhea not due to acute otitis externa
Clinicians should diagnose AOM in children who present with (C) Mild bulging of the TM and recent (
-
TM Characteristics in AOMNormal TM TM Characteristics in AOM Opaque Red, yellow or cloudy
Normal TM Translucent/transparent Gray or pink color
Bulging or full position Reduced mobility but may respond to positive
pressure on pneumatic otoscopy
Neutral position Fully mobile with pneumatic otoscopy N ff i pressure on pneumatic otoscopy
Effusion present No effusion
- Bacterial Etiology of Acute Otitis Media in Young Children (3 mo-
- Antimicrobial Susceptibility of S. pneumoniae, Siriraj Hospital, 2008( f h ld )N=170(32.4%fromchildren
-
Acute otitis media Risk for DRSP:Risk for DRSP:
>> Recent antimicrobial exposure Recent antimicrobial exposure (within 3 mo)>> Young age (> Day-care attendance
Dowell. PIDJ 1999;18:1-9.
-
Betalactamase producing organisms in Thailand
100% of M. catarrhalis BUT high rate of gspontaneous clinical resolution
48.8% of H. influenzae Overall, H. influenzae isolates are susceptible to
regular and high dose amoxicillin 58 82%*regular and high-dose amoxicillin 58-82%**AAP. Pediatrics 2013;131:e964e999.
Critchley et al. J Chemother. 2002. 14: 147-154Srifuengfung S, et al. Southeast Asian J Trop Med Public Health 2007;38(4):732-6
AAP. Pediatrics 2013;131:e964 e999.
-
Bacteria causing AOM in North America, 2012
-
Recommendations for Initial Management for Uncomplicated AOMAge Otorrhea
WithUnilateral or
Bilateral AOM Bilateral AOM
Without OtorrheaUnilateral AOM
Without OtorrheaAOM With Severe
Symptoms *6 2 A tibi ti A tibi ti A tibi ti A tibi ti th 6 mo - 2 y Antibiotic
therapyAntibiotictherapy
Antibiotictherapy
Antibiotic therapy orObservation with close F/U**
2 Antibiotic Antibiotic Antibiotic therapy or Antibiotic therapy or2 y Antibiotictherapy
Antibiotictherapy
Antibiotic therapy orObservation with close F/U**
Antibiotic therapy orObservation with close F/U**
* Toxic-appearing , persistent otalgia > 48 h, T 39C in the past 48 h, or uncertain access to F/U** Joint decision-making with parents/caregiver If observation is offered ensure F/U and begin Joint decision making with parents/caregiver, If observation is offered, ensure F/U and begin antibiotics if worsens or fails to improve within 48 - 72 h of onset
AAP. Pediatrics 2013;131:e964e999.
-
Recommended Antibiotics for AOM First line:A i illi Amoxicillin
If the child has not received amoxicillin in the past 30 daysNo concurrent purulent conjunctivitis
(narrow spectrum, effective, safe, low cost, acceptable taste)( p p ) Amox/Clav
If th hild h i d i illi i th t 30 d If the child has received amoxicillin in the past 30 days With concurrent purulent conjunctivitis (more likely NTHi )History of recurrent AOM unresponsive to amoxicillin
Reassess the patient within 48 - 72 hours to determine whether a change in therapy is needed
AAP. Pediatrics 2013;131:e964e999.
-
Recommended Antibiotics for AOM
Levofloxacin or linezolid may be indicated in refractory casesAAP. Pediatrics 2013;131:e964e999.
Levofloxacin or linezolid, may be indicated in refractory cases
-
Pichichero ME. Am Fam Physician 2000;61(8):2410-6
-
Duration of Therapy for AOM and F/Upy O ti l d ti i t i ll d Optimal duration is uncertain, usually recommend
10 days10 days < 2 y and children with severe AOM : 10 daysy y 2-5 y with mild to mod AOM: 7 days > 6 y with mild to mod AOM: 5-7 days
AAP. Pediatrics 2013;131:e964e999.
-
- ( 80%) ( ) -
Common cold
group A (Acute Otitis Media AOM) (Acute rhinosinusitis) - Common cold
- Acute viral rhinosinusitis- pharyngitis- acute bronchitis :
- group A beta hemolytic streptococcus - 39 C - - -
(Acute Otitis Media, AOM) otoscope - - 2 AOM 2 -
(Acute rhinosinusitis) - URI sinusitis facial pain, postnasal drip, purulent discharge- URI 10 - 5-6 X-Ray
>3 3
-
2 (1) Amoxicillin 50-90 mg/kg/day 2-3 10 3 90 mg/kg/da
1 - Amoxicillin 50 mg/kg/day 1-2 10
3 (1) Amoxicillin 50-90 mg/kg/day 2 10-14 5-7 3 high dose (90 mg/kg/da )
90 mg/kg/day
(2) penicillin Type I hypersensitivity Cefdinir 14 mg/kg/day 1-2 Cefditoren 10 mg/kg/day 2-3 (3) penicillin Type I azithromycin 10 mg/kg/day 5 mg/kg/day
- penicillin Type I cephalexin 20 mg/kg/dose ( 500 mg/dose) 2 10 - Penicillin type I Roxithromycin 5-8 mg/kg/day ( 300 mg/day) 2 10 azithromycin 12 mg/kg/day ( 500
/d ) 5 l ith i 15
dose (90 mg/kg/day) (2) penicillin Type I hypersensitivity Cefdinir 14 mg.kg/day 2 cefditoren 18 mg/kg/day 2 (3) ) penicillin Type I Azithromycin clarithromycin levofloxacin 10 mg/kg/day
4 clarithromycin 15 mg/kg/day 10 72 amoxicillin/clavulanate (Amoxillin 80-90 mg/kg/day) 2 cefdinir, cefditoren (18 mg/kg/day) levofloxacin (10-20 mg/kg/day)
mg/dose) 5 clarithromycin 15 mg/kg/day ( 250 mg/dose) 2
3-5 amoxicillin/clavulanate (Amoxillin 90 mg/kg/day) 2 cefdinir, cefditoren + clindamycin levofloxacin)
levofloxacin (10 20 mg/kg/day)
1.IDSA Guideline for GAS Pharyngitis 2012.CID2. AAP Guideline for AOM 2013. Pediatrics3. IDSA Guideline for ABRS 2012. CID
-
Indications for antibiotics (Acute Otitis Media, AOM) otoscope
- - 2 AOM 2
- -
-
Siriraj Guidelines: Antibiotics Amoxicillin 50-90 mg/kg/day 2-3 10 3
90 mg/kg/day t I i illi h iti it non-type I penicillin hypersensitivity:
- Cefdinir 14 mg/kg/day 1-2 Cefditoren 10 mg/kg/day 2-3 T I i illi h iti it Type I penicillin hypersensitivity
- Azithromycin 10 mg/kg/day 5 mg/kg/day 4 clarithromycin 15 mg/kg/day 10 - clarithromycin 15 mg/kg/day 10
72
- Amoxicillin/clavulanate (Amoxillin 80-90 mg/kg/day) 2 cefdinir, cefditoren (18 mg/kg/day) levofloxacin (10-20 mg/kg/day) , ( g g y) ( g g y)
-
8 8 A previously healthy 9 months old infant 8. A previously healthy 9-months old infant 2 days PTA She developed vomiting twice times/day and three 2 days PTA, She developed vomiting twice times/day, and three
episodes of non bloody diarrhea. She has been afebrile. She refuses fluids but still alertfluids but still alert.
Physical examination T 36.5 o c, P 120/min (full), BP 80/60 mmHg, RR 30/min G/A: Alert, dry lip, no sunken eye ball, capillary refill < 2 sec, no rash Res/CVS : WNL Abd : soft no distension no hepato-splenomegaly active bowel soundsAbd : soft, no distension, no hepato splenomegaly, active bowel sounds
-
8Treatment: She received ORS and motilium syrupTreatment: She received ORS and motilium syrupAnd F/U stool c/s report at OPD 3 days laterp yInvestigation CBC: Hb11.7g/dl, Hct 35.3%,
Wbc 8 560 cell/mm3 (N 60 % L Stool c/s : Salmonella gr.c
Wbc 8,560 cell/mm (N 60 %, L 38%, Eo 0.8%,Mo 0.9%, Ba 0.3%), Plt. 388,000 cell/mm3
Stool exam : WBC 3-5, no RBC Stool exam : WBC 3 5, no RBC
-
8Which of the following is the most Which of the following is the most
i t t t t f thi i f t?appropriate treatment of this infant?
-
8Which of the following is the most Which of the following is the most
i t t t t f thi i f t?appropriate treatment of this infant?. Ceftibuten 9 mg/kg/d x 3 days. No antibiotics. Ciprofloxacin 40 mg/kg/d x 3 days
-
8Which of the following is the most Which of the following is the most
i t t t t f thi i f t?appropriate treatment of this infant?. Ceftibuten 9 mg/kg/d x 3 days. No antibiotics. Ciprofloxacin 40 mg/kg/d x 3 days
-
Antibiotics for treating salmonella gut infections 12 trials involving 778 participants (with at least 258
infants and children) There were no significant differences in length of illness There were no significant differences in length of illness,
diarrhoea or fever between any antibiotic regimen and placebo.
Antibiotic regimens resulted in more negative cultures Antibiotic regimens resulted in more negative cultures during the first week of treatment.
Sirinavin S, Garner P. The Cochrane Collaboration 2009
-
Antibiotics for treating salmonella gut infections Relapses were more frequent in those receiving
antibiotics, and there were more cases with positive cultures in the antibiotic groups after 3 positive cultures in the antibiotic groups after 3 weeks.
Adverse drug reactions were more common in the antibiotic groups (Peto odds ratio 1.67, 95% CI 1.05 to 2.67).1.05 to 2.67).
Sirinavin S, Garner P. The Cochrane Collaboration 2009
-
Empirical ATB Therapy in Acute Diarrhea Consider in those without clue of viral infection
Severe or Persistent Dysentery Age < 6 monthsAge < 6 months Immunocompromised/ Underlying disease
(Otherwise treat only Cholera and Shigella) Choices
Norfloxacin (or ciprofloxacin) TMP/SMX (Neomycin not proven effective)y p Third gen cephalosporin
-
Comparison of the efficacy of ceftibuten and norfloxacin in the treatment of acute gastrointestinal infection in children
A prospective randomized study at an ID hospital in Thailand. Ceftibuten was compared with norfloxacin, both given orally for 5 days for treatment of acute gastroenteritis in children.
170 cases were included: 88 cases were treated with ceftibuten and 170 cases were included: 88 cases were treated with ceftibuten and 82 cases with norfloxacin.
No statistically significant differences in either comparison (p > 0.05). Neither complications nor clinical relapses were observed.
Southeast Asian J Trop Med Public Health 1999 ;30(4):764-9.
-
Inappropriate Use of ATB in Diarrhea Not shorten illness Unnecessary cost Risk for A/ERisk for A/E Prolong shedding (Salmonella) Increase Risk of HUS (STEC) Create drug resistance problem
More than 80% of acute diarrhea are from viral/ or self-limited
-
9 9. 8
5 5 / clinic ORS, paracetamol, motilium clinic ORS, paracetamol, motilium
. 1 .
Physical examination: T 39.5o C, P 140/min, BP 90/60 mmHg
Alert, dry lips, AF 1x1 cm no bulging, no hepatosplenomegaly, Skin - no rash CNS: Alert, pupil 2 mm BRTL, no facial palsy
Motor : equally movement both, grade V/V allq y gStiffness of neck and brudzinskis sign : negative
-
9Investigations CBC :Hb 11
g/dl Hct Stool
Exam : WBC 0 1 no RBCg/dl, Hct32% WBC 12,060
3 (
Exam : WBC 0-1, no RBC C/S : pending
cell/mm3 ( N 41.6 %, L
H/C: pending CSF
51.8%, Mo 6.3%, Ba0.3%), plt. 175,000 /mm3
WBC 6 /mm3, RBC 840/ mm3
Protein 19 mg/dl sugar 87/91 mg/dlp U/A : PH 6.5, sp.gr.
1 020 t i
Protein 19 mg/dl, sugar 87/91 mg/dl Gram stain: no organism found
1.020, protein neg, sugar
C/S : pending
-
9
-
9
. Cefotaxime. Cefotaxime + Ciprofloxacin . stool Rotavirus Ag, antibiotic
-
9
. Cefotaxime. Cefotaxime + Ciprofloxacin . stool Rotavirus Ag, antibiotic
-
Progression Progression Aft i i l tibi ti After empirical antibiotic
cefotaxime200 /k /d 48 h
TreatmentCefotaxime (31/8 6/9/56) 200 mg/kg/day x 48 hr.
Patient still had high grade f b di h d
Cefotaxime (31/8-6/9/56) x 7 days
fever, but diarrhea and vomiting decreased Ciprofloxacin iv was
added H/C report : gram
negative rod
-
Progression Progression TreatmentC f t i (31/8 6/9/56) 7 Cefotaxime (31/8-6/9/56) x 7 days
Stool c/s : no growth CSF c/s : no growth
H/C (1 2/9/56) S l ll C Ciprofloxacin iv
(1-6/9/56) x 6 days
H/C (1,2/9/56) : Salmonella gr.C
Bactrim (6-21/9/56) x 15 days
H/C ( 4/9/56) : no growth / ( / / ) g
-
Children with Invasive NonChildren with Invasive Non--TyphoidalTyphoidal SalmonellaSalmonella infection, infection, SirirajSirirajHospital, Hospital, 20062006--2011 2011 (n = (n = 8080))
Data N (%)
Median age (range) 12 months (11 days 13.9 years)
Underlying conditionsUnderlying conditionsPreviously healthyImmnunodeficiency
Hematologic malignancies
42 (52.5)
10 (12 5)Hematologic malignanciesSLEHIVInterleukin-12 deficiency
10 (12.5)6 (7.5)4 (5.0)1 (1.2)y
OthersBiliary atresiaCongenital heart diseases
( )
5 (6.3)5 (6.3)
ThalassemiaG-6-PD deficiencyOthers
1 (1.2)2 (2.5)4 (5.0)
Clinical manifestationsFeverDiarrhea
79 (98.7)43 (53.8)
HepatomegalySplenomegaly
( )7 (8.7)4 (5.0)
Saihongthong S, Phongsamart W, et al. 15th International Congress on Infectious Diseases ,Bangkok , Thai land, June 13-1 6 , 2012
-
Children with Invasive NonChildren with Invasive Non--TyphoidalTyphoidal SalmonellaSalmonellainfection, infection, SirirajSiriraj Hospital, Hospital, 20062006--2011 2011 (n = (n = 8080))
Data N (%)
Laboratory resultsLaboratory resultsWBC (cells/mm3)
< 5,0005 000 15 000
15 (18.7)43 (53 8)5,000-15,000
> 15,000Thrombocytopenia
43 (53.8)22 (27.5)22 (27.5)
OutcomeRecurrence (NTS bacteremia)Complications (1 meningitis with subdural empyema 1 septic
2 (2.5)2 (2 5)Complications (1 meningitis with subdural empyema, 1 septic
shock)Death
2 (2.5)2 (2.5)
Saihongthong S, Phongsamart W, et al. 15th International Congress on Infectious Diseases ,Bangkok , Thai land, June 13-1 6 , 2012, # Abstract No. 45.065
-
229 children 018 years in 2001-2010 with culture-proven invasive Salmonella infections, 98.6% were non-typhoidal Salmonella
di ( Q ) 0 ( 9 ) h 63 i l Median age (IQR) was 10 (19.5) months, 63% were previously healthy
Di h f d i 40% f Diarrhea were found in 40% of cases 23% presented with fever without source
53% f h h d WBC i hi l li i (5000 15 000 53% of the cases had WBC within normal limits (500015,000 cell/mm3)
The overall case fatality rate 4 8% The overall case fatality rate 4.8%
Punpanich W, et al. Pediatr Infect Dis J 2012;31(8):e105-10.
-
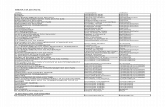
Antimicrobial Resistance among Invasive Antimicrobial Resistance among Invasive SalmonellosisSalmonellosis, , SirirajSiriraj Hospital Hospital 20062006--2011 2011 and QSNICH and QSNICH 20012001--20102010
Si i j H it l QSNICH
(n = 80 NTS1 and 2292)
76.368.3
SirirajHospital QSNICH
tance
2550
34
4 12.533.9
15.2 17.43%
Resis
1. Saihongthong S, Phongsamart W, et al. 15th International Congress on Infectious Diseases Bangkok , Thai land, June 13-1 6 , 2012.2. Punpanich W, et al. Pediatr Infect Dis J 2012;31(8):e105-10.
-
Susceptibility Testing for Susceptibility Testing for SalmonellaSalmonella Decreased ciprofloxacin susceptibility/Nalidixic acid resistant is
correlated with delayed responses, clinical failures, and i d li i i i CIP f S hiincreased mortality among patients receiving CIP for S. typhiand NTS
CLSI/NCCLS: CLSI/NCCLS: CLSI 2004 screen extra-intestinal Salmonella with CIP MICs 1 g/mL
for NAL resistance. If NAL resistance, lab was instructed to indicate to clinicians that FQ treatment might not be efficacious
CLSI 2012: NAL screening does not detect all mechanisms of FQ resistance CIP should also be tested and interpreted using the new resistance, CIP should also be tested and interpreted using the new susceptible MIC break point of 0.06 g/mL or zone size 31 mm with disk diffusion
Humphries RM, et al. CID 2012;55(8):110713.
-
Treatment of Invasive SalmonellosisTreatment of Invasive Salmonellosis Salmonella meningitis: high rates of mortality, complications and
relapse1 UK1: imaging, document sterilization, Cefotaxime/ceftriaxone +
ciprofloxacin > 4 wks or > 3 wks after 1st sterile (repeat after Rx D4)
PIDST 2013-20142: combination of Cefotaxime/ceftriaxone + /ciprofloxacin 4-6 wks
High rates of Ceftotaxime/ceftriaxone resistanceConsider adding ciprofloxacin in suspected/proven
invasive Salmonellosis pending for susceptibility results
O i f f i / f i FQN i Options for cefotaxime/ceftriaxone + FQN resistance: Co-trimoxazole if susceptible, Imipenem, or Azithromycin
1. Price EH, et al. J Antimicrob Chemother 2000;46:653-5.2. Meningoencephalitis Guideline 2013-2014.