67030963
-
Upload
stephaniedian -
Category
Documents
-
view
215 -
download
0
Transcript of 67030963

8/21/2019 67030963
http://slidepdf.com/reader/full/67030963 1/6
M A T E R N O - F E T A L M E D I C I N E
Correlation of myometrial thickness and the latency intervalof women with preterm premature rupture of the membranes
Lina AtarJavdan • Zahra Khazaeipour •
Fatemeh Shahbazi
Received: 19 September 2010 / Accepted: 11 January 2011/ Published online: 5 February 2011
Springer-Verlag 2011
Abstract
Objective To verify the hypothesis that a correlationexists between myometrial thickness (MT) and latency
interval (LI) in patients with preterm premature rupture of
membrane (PPROM).
Method Myometrial thickness was measured ultrasono-
graphically at the mid-anterior (MA), fundal, and posterior
parts of the uterus of pregnant women in the following
groups: PPROM [n = 45, mean (range), gestational age
(GA): 28.6 weeks (w) (24.0–33.0 w)], preterm nonlabor
control group (P-CTR) [n = 20, GA: 29.5 w (25.0–
32.0 w)] and term nonlabor control (T-CTR) [n = 27, GA:
38.4 w (37.0–41.0 w)].
Results There was a positive correlation between LI and
fundal MT (r = 0.34, P = 0.02), mid-MT (r = 0.47,
P = 0.001) and LUS (r = 0.74, P = 0.001). The results
were similar in the group of \30 w of GA, but in the group
of C30 w of GA, there was no association. The LUS MT
has more area under the ROC curve than MA MT and
fundal MT for prediction of LI of B8 days.
Conclusion Significant positive correlation between LI
and MT in patients with PPROM may result in a better
decision for taking care of infants of preterm birth.
Keywords PPROM Myometrial thickness
Latency interval
Pregnancy
Preterm birth
Introduction
Premature rupture of membranes (PROM) is defined as the
rupture of membranes before delivery signs are evidenced. It
has been reported that prevalence of PROM is 6–10%, of
which 80% happened after week 37 of pregnancy [1]. PROM
followed by pretermdelivery is the most prevalent reason for
prenatal morbidity and mortality in the USA [2, 3]. If PROM
happens before week 37 of pregnancy, it is called preterm-
premature rupture of membrane (PPROM). PPROM has
many reasons, but infection is the most common reason [4].
With PROM, morbidity and mortality increases. The major
risk is intra-uterine infection that causes PROM directly. By
reduction of pregnancy term, fetal morbidity and demise
increase as a result of preterm birth and fetal abnormality.
Despite the wide care during birth and increasing access to
infant intensive care unit, preterm birth and low weight of
infants is responsible for 75% of infant mortality [5]. Based
on the hypothesis that even one small delay during PPROM
to delivery is useful for the fetus, treatment of pregnancy
with PPROM occurred, in the absence of clinical symptoms
or experimental chorioamniotic [4].
Researchers have been investigating the factors that
cause preterm delivery such as digital examination of the
cervix, monitoring of uterine contraction at home and LUS
thickness [6–9]. Digital investigation of cervix and fre-
quency of uterine contractions for prediction has less value
[7]. Furthermore, digital investigation of cervix may
increase the risk of progressive infection [10].
It has been investigated that the clinical predictors of
early preterm delivery (PTD) including cervical change,
L. AtarJavdan
Women Hospital (Mirza Kuchakkhan Women Hospital),
Tehran University of Medical Sciences, Karimkhan Zand Street,
Tehran, Iran
Z. Khazaeipour (&) F. Shahbazi
Research Deputy of Imam Khomeini Hospital Complex,
Tehran University of Medical Sciences, Keshavarz Blvd,
14155-6388 Tehran, Iran
e-mail: [email protected]
1 3
Arch Gynecol Obstet (2011) 284:1339–1343
DOI 10.1007/s00404-011-1841-x

8/21/2019 67030963
http://slidepdf.com/reader/full/67030963 2/6
uterine contractions, vaginal bleeding and the birth activity
of fetus were neither sensitive nor specific. These pre-
monitory symptoms are only exact at the late stages in the
pathogenic procedure [11].
A few studies have investigated the correlation of
myometrial thickness (MT) with PPROM and delivery time
[12], but this correlation has not been well verified. Veri-
fication of the correlation between MT and longer latencyinterval of women with PPROM may assist clinicians in
providing consultation regarding management for women
presenting with PPROM and may result in a better decision
for taking care of infants after preterm birth.
Our aims were to study the correlation of MT and
latency interval (LI) and prediction ofLI and delivery, in
patients with PPROM.
Materials and methods
Study design
A prospective cohort study was performed in 92 pregnant
women enrolled in the following groups: exposure group
[n = 45, PPROM, gestation age (GA): 24–33 weeks (w)],
the control group, which consisted of healthy pregnant
women [preterm nonlabor control group (P-CTR, n = 20,
GA = 25–32) and term nonlabor control group (T-CTR,
n = 27, GA = 37–41)] referred to Mirza Kochakkhan
hospital between 2007 and 2009. The patients referred to
the hospital were aged 22–37 years, but the only inclusion
criterion was singleton pregnancy.
Fetal anomalies, asymmetric intrauterine growth retar-
dation (IUGR), weight\10% for GA based on ultrasono-
graphic evaluation, placenta abnormalities (low lying
placenta, abruptio placentae), degree of implantation of
placenta within the uterus, cervical cerclage in the absence
of sign and symptom of chorioamnionitis, fever more than
38C, fetal tachycardia and fetal heart beat abnormalities
(late deceleration or variable of heart beat) were excluded.
All the women who had the input qualifications were asked
to participate in this research and signed the informed
consent.
For diagnosis of PROM, both positive fern and nitrazine
tests at the time of admission by sterile speculum exami-
nation ‘‘to see amniotic fluid (AF)’’ were performed.
Ultrasonographic evaluation for women with PROM was
performed during 12 h.
All scans on women in the threatened PROM group
were performed abdominally via sonographic equipment
(focuda) using transabdominal curvilinear probe with a
3.5-MHz frequency. The amniotic fluid index (AFI) was
calculated and for oligohydramnios AFI\ 5 cm was
considered. With sonographic evaluation, myometrium was
identified as the echo homogeneous layer between the
serosa and the decidua.
MT was measured at three different parts: at the lower
uterine segment (LUS, 2 cm above the urinary bladder
reflection), mid-anterior (MA, with probe, 1 cm above the
patient’s navel) and fundal (beginning of the curved part of
the uterus) wall. Fundal thickness of the uterine body was
measured by placing the probe scans above the uterinefundus and all the bent parts of the uterine body were seen.
Each scan was measured separately; at least three mea-
surements of each part were performed and mean ± SE
was obtained. Both sonography and measurements were
performed by one researcher. Reliability of measurements
in the intraobserver was 93%.
Treatments of patients were performed by the treatment
group. All the patients received corticosteroid for fetal lung
maturation, and antibiotics (ampicillin/erythromycin)
according to the PPROM protocol [13]: intravenous
ampicillin (2-g dose every 6 h) and erythromycin (250-mg
dose every 6 h) for 48 h, followed by oral amoxicillin(250-mg dose every 8 h), erythromycin base (333-mg dose
every 8 h) for 5 days and intramuscular corticosteroids
(12 dose, every 24 h) for 2 days.
Patients \32 weeks received corticosteroid for lung
maturation and antibiotics (ampicillin/erythromycin). To
investigate the fetal abnormality or uterus contraction,
women were monitored daily by cardiotocography method.
Sonography (two times a week) and NST (daily) were
performed.
Data analysis was performed with the SPSS software
(SPSS Inc., Chicago, IL, USA). Normal distribution of data
were analyzed by one-sample Kolmogorov–Smirnov test. To
compare three group means, Kruskal–Wallis test and
ANOVA wereused, and for two group means Mann–Whitney
U test was used. Spearman’s q was used to identify correla-
tion. Quantitative variables were shown by mean ± SD.
Differences were considered significant when P\0.05.
Ethical issues
This research was based on Helsinki principle’s declara-
tions. Signed informed consent was obtained from each
patient and it was ensured that there was no loss or harm to
the patients.
All the information from the patients was kept
confidential.
Results
The mean of age for PPROM was 27.9 ± 4.7 years
(22–37 years); the mean for GA based on LMP was
28.6 ± 3.3 w (24–33 w).
1340 Arch Gynecol Obstet (2011) 284:1339–1343
1 3

8/21/2019 67030963
http://slidepdf.com/reader/full/67030963 3/6
The mean values of GA based on ultrasonography in the
first trimester in group T-CTR (37–41), group P-CTR
(25–32) and group PPROM (24–34) were 38.4 ± 1.27,
29.5 ± 2.23 and 28.6 ± 3.2, respectively (P = 0.002).
There were significant differences between T-CTR and
P-CTR (P = 0.001) and between T-CTR and PPROM
(P = 0.001).
The mean value of AF in the PPROM group (2–14 cm)was 5.9 ± 3.22, of which gravid 1, gravid 2, gravid 3,
gravid 4 and gravid 5 had 46.7, 26.7, 17.8, 8.9 and 8/9%,
respectively.
As much as 55.6% of them were without miscarriages
and 28.9% had miscarriage only once; 77.8% were without
a live birth at delivery, 13.3% with one live birth, 8.9%
with two live births, and 2.2% with one stillborn.
Regarding fetal presentation, 17.8% were breech pre-
sentations (n = 8) and 82.2% were cephalic presentations
(n = 37). Regarding placenta position, 20% were of fundal
position (n = 9), 33.3% of posterior position [15] and
46.7% of anterior position (n = 21). Demographic andclinical characteristics and the correlation between MT at
three different parts of the uterus (fundal, mid-anterior and
LUS) in T-CTR, P-CTR and PPROM groups are presented
in Table 1. There was no significant correlation between LI
and AF, but positive correlation between LI and MT at
three different parts as shown as follows: LUS (r = 0.74,
P = 0.001), MA (r = 0.47, P = 0.001), fundal (r = 0.34,
P = 0.02). In the group of GA B 30 w, no significant
correlation between LI and AF (r = 0.15, P = 0.4) was
found. Correlations between LI and MT were: MA,
r = 0.36, P = 0.049; LUS, r = 0.69, P\ 0.0001; and
fundal, r = 0.3, P = 0.08. In the group of GA[ 30 w, nosignificant correlation between any of the variables was
found. The correlations between LI with AF and MT at
three different parts in group 1 (AF B 5) and group 2
(AF[ 5) are presented in Table 2.
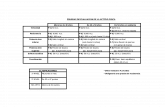
Figure 1 shows that for the latency interval of B8 days,
area under curve of LUS MT (0.92) was more than fundal
MT (0.65) and MA MT (0.70).
The sensitivity, specificity and thickness of MT in three
different parts of the uterus for LI of B8 days are presented
in Table 3.
Discussion
Based on sonography, GA showed significant differences
between the three groups (P = 0.002) and two groups as
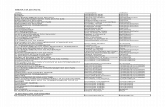
Table 1 Demographic and clinical characteristics and comparison between myometrial thickness at three different parts (fundal, mid-anterior
and LUS) in T-CTR, P-CTR and PPROM groups
Myometrial thickness T-CTR P-CTR PPROM P value
Age
Mean ± SD 28.3 ± 4.04 27.3 ± 4.96 27.9 ± 4.7 0.7
Median (range) 28 (23–35) 25 (22–37) 27 (22–37)
Gestational age (based on sonography)
Mean ± SD 38.4 ± 1.28 29.5 ± 2.23 28.7 ± 3.23 \0.0001
Median (range) 38 (37–41) 30 (25–32) 29 (24–34)
Fundal
Mean ± SD 8.3 ± 1.04 7.7 ± 1.11 8.2 ± 3.44 0.1
Median (range) 8.6 (6–10) 7.6 (5–10) 8 (2–19)
Mid-anterior
Mean ± SD 9 ± 1.66 7.7 ± 1.53 8.7 ± 4.37 0.04
0.002*
Median (range) 8.8 (6–14) 7.2 (5–12) 8 (2–22) 0.2
LUSMean ± SD 5.6 ± 1.35 6.4 ± 0.76 8.1 ± 4.25 0.002
0.006
Median (range) 5.3 (4.2–9) 6.5 (4–7.5) 7 (3.2–22) 0.002§
0.1||
* Comparison of P-CTR with T-CTR Comparison of T-CTR with PPROM Comparison of P-CTR with T-CTR§ Comparison of T-CTR with PPROM|| Comparison of P-CTR with PPROM
Arch Gynecol Obstet (2011) 284:1339–1343 1341
1 3

8/21/2019 67030963
http://slidepdf.com/reader/full/67030963 4/6
well (T-CTR and P-CTR, P = 0.001) (T-CTR and
PPROM, P = 0.001).
In contrast to Buhimschi results, which showed that the
fundal part of the myometrial of the PPROM group was
thicker than the other groups (P-CTR, P\ 0.001 and
T-CTR, P = 0.015) [12], we found that there were no
differences for fundal MT in these three groups.Buhimschi results showed that myometrium at the MA
part was thicker in the PPROM group than in the other
groups (P-CTR, P\ 0.001; and T-CTR, P = 0.025).
Similarly our results showed significant differences
(P = 0.04) for the MA MT of the three groups and
between two groups as well (T-CTR and P-CTR,
P = 0.002). However, dissimilar to Buhimschi results,
myometrium in the T-CTR was thicker than that in the
others (P-CTR, P\0.001; and T-CTR, P = 0.025).
LUS MT mean values in T-CTR (4.2–9, 5.6 ± 1.35)
was less than P-CTR (4–7.5, 6.4 ± 0.76) and PPROM
(3.2–22, 8.1 ± 4.25 mm); P = 0.002.
Comparison of LI in GA B 30 w ( M = 8.5, Q1–Q3 =
4.7–11.2) with GA[ 30 w ( M = 7, Q1–Q3 = 3–10) did
not show significant differences (P = 0.1). A few reports
have shown inverse correlation between gestational age at
rupture of membranes with LI [14, 17]. Similar to this
former report, Test et al. [16] reported that the duration of
the LI was significantly longer among women with
PPROM before 34 weeks as compared to PPROM after
34 weeks of gestation (5.78 vs. 2.02 days; P\ 0.001).
Manuck et al. [15] also suggested that LI does not appear to
worsen outcomes in pregnancies that are complicated by
PPROM.
LI has no significant correlation with AF, but it has a
significant and positive correlation with MT at three dif-
ferent parts: fundal, MA and LUS (r = 0.74, P = 0.001).
Similar results were seen for the group of B30 w preg-
nancy, but in the group of [30 w of pregnancy there was
no association. LI in two groups of AF B 5 cm and
AF[ 5 cm also have positive and significant correlation
with MT (MA, Fundal and LUS), but no association with
AF was seen. In contrast to our results, Test et al. [16]
reported that prolonged latency was a significant risk factor
for chorioamnionitis. Aziz et al. [18] suggested that earlier
gestational age at the time of PPROM is associated with
longer LI, which, in turn, is not associated with increased
neonatal sepsis or chorioamnionitis.
Our results present a positive correlation between MT in
fundal and LI (r = 0.34, P = 0.02), which is similar to the
results of Buhimschi (r = 0.43, P = 0.02) [12]. LI was
8 days ( M = 8 days) and MT for the LUS part (0.92) was
more than that for fundal (0.65) and MA (0.70) parts
(Fig. 1).A fundal MT of 6.9 mm was 79% sensitive and 39%
specific for the identification of women whose LI was
8 days and an MA MT of 5.5 mm was 89% sensitive and
42% specific for the identification of women whose LI was
8 days, while Buhimschi showed that a fundal MT was less
than 12.1 mm, 93.7% sensitive and 63.6% specific for the
identification of women whose LI was 5 days. Buhimschi
concluded that a thick myometrium in nonlaboring patients
with PPROM is associated with longer latency interval.
ROC Curve
1 - Specificity
1.00.75.50.250.00
S e n s i t i v i t y
1.00
.75
.50
.25
0.00
Source of the Curve
Reference Line
LUS
Mid Anterior
Fundal
Fig. 1 ROC curve represents the thickness sensitivity and specificity
(diagonal segments are produced by ties) for three different parts
(fundal, midanterior and LUS) of uterus for the women whose latency
interval was 8 days
Table 3 Represent the information based on Fig. 1
Myometrial thickness Mid-anterior LUS Fundal
Sensitivity 89% 89% 79%Specificity 42% 85% 39%
Thickness 5.5 mm 7.35 mm 6.9 mm
Latency interval 8 8 8
Table 2 The correlation between latency interval with amniotic fluid and myometrial thickness at three different parts in group 1 (AF B 5) and
group 2 (AF[ 5)
Myometrial thickness Mid-anterior LUS Fundal Amniotic fluid
Latency interval (group 1) r = 0.37, P = 0.039 r = 0.8, P\0.0001 r = 0.2, P = 0.2 No correlation
Latency interval (group 2) r = 0.81, P = 0.0001 r = 0.739, P = 0.003 r = 0.53, P = 0.047 r = 0.78,
P = 0.001
1342 Arch Gynecol Obstet (2011) 284:1339–1343
1 3

8/21/2019 67030963
http://slidepdf.com/reader/full/67030963 5/6
Sonographic evaluation of MT may represent an alternative
clinical tool for the prediction of a short LI in women with
PPROM [12].
Conflict of interest We declare that we have no conflict of interest.
References
1. French JL, Mc Gregor JA (1996) The pathology of premature
rupture of membranes. Semin Perinatol 20(5):344–368
2. Garite TJ (1985) Premature ruptures of the membranes the
enigma of the obstetrician. Am J Obstet Gynecol 151:1001–1005
3. Berkowitz GS, Papiernik E (1993) Epidemiology of preterm
birth. Epidemiol Rev 15:414–443
4. Daikoku NH, Kaltreider DF, Johnson TR Jr., Johnson JW, Sim-
mons MA (1981) Premature rupture of membranes and preterm
labor: neonatal infection and perinatal mortality risks. Obstet
Gynecol 58:417–425
5. Weitz BW (2001) Premature rupture of the fetal membranes.
MCN 26(2):86–93
6. Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, DasA et al (1996) The length of the cervix and the risk of sponta-
neous premature delivery. National Institute of Child Health and
Human Development Maternal Fetal Medicine Unit Network.
N Engl J Med 334:567–572
7. Owen J, Iams JD, Hauth JC (2003) Vaginal sonography and
cervical incompetence. Am J Obstet Gynecol 188:586–596
8. Yost NP, Owen J, Berghella V, Macpherson C, Swain M, Dildy
GA et al (2004) Second trimester cervical sonography: features
other than cervical length to predict spontaneous preterm birth.
Obstet Gynecol 103:457–462
9. Iams JD (2003) Prediction and early detection of preterm labor.
Obstet Gynecol 101:402–412
10. Lewis DF, Major CA, Towers CV, Asrat T, Harding JA, Garite
TJ (1992) Effects of digital examinations on latency period in
preterm premature rupture of membrane. Obstset Gynecol
80:630–634
11. Lockwood CJ (1995) The diagnosis of preterm labor and the
prediction of preterm delivery. Clin Obstet Gynecol 38:675–687
12. Buhimschi CS, Buhimschi IA, Norwitz ER, Sfakianaki AK,
Hamar B, Copel JA et al (2005) Sonographic myometrial thick-
ness predicts the latency interval of women with preterm pre-
mature rupture of the membranes and oligohydramnios. Am J
Obstet Gynecol 193 (3pt1):762–770
13. Mercer BM, Midovnik M, Thurnau GR, Goldenberg RL, Das AF,
Ramsey RD et al (1997) Antibiotic therapy for reduction of infant
morbidity after preterm premature rupture of the membranes. A
randomized controlled trial. JAMA 278:989–995
14. Davis JM, Krew MA, Gill P, Nelson KM, Hopkins MP (2008)
The role of continuous fetal monitoring in the management of
preterm premature rupture of membranes. J Matern Fetal Neo-
natal Med 21(5):301–304
15. Manuck TA, Maclean CC, Silver RM et al (2009) Preterm pre-
mature rupture of membranes: does the duration of latency
influence perinatal outcomes? Am J Obstet Gynecol 201(4)
p414.e1–e6
16. Test G, Levy A, Wiznitar A, Mazor M, Holcberg G, Zlotnik A
et al (2010) Factors affecting the latency period in patients with
preterm premature rupture of membranes. Arch Gynecol Obstet.
doi:10.1007/s00404-010-1448-7
17. Melamed N, Hadar E, Ben-Haroush A, Kaplan B, Yogev Y
(2009) Factors affecting the duration of the latency period in
preterm premature rupture of membranes. J Matern fetal neonatal
Med 22(11):1051–1056
18. Aziz N, Cheng YW, Caughey AB (2008) Factors and outcomes
associated with longer latency in preterm premature rupture of
membranes. J Matern fetal neonatal Med 21(11):821–825
Arch Gynecol Obstet (2011) 284:1339–1343 1343
1 3

8/21/2019 67030963
http://slidepdf.com/reader/full/67030963 6/6
Copyright of Archives of Gynecology & Obstetrics is the property of Springer Science & Business Media B.V.
and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright
holder's express written permission. However, users may print, download, or email articles for individual use.