課程資訊
Transcript of 課程資訊

台灣顱底外科醫學會第四屆第一次會員大會暨學術研討會地點:台北榮總致德樓第一會議室 (台北市石牌路二段 201 號)
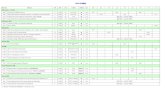
Scientific Program ( 97 年 11 月 15 日 星期六 )
時間 議程08:00~08:45 會員報到08:45~09:00 潘宏基理事長 Opening remark
學術演講 座長 演講者 題目9:00~9:20 曾漢民
魏志鵬鄭澄懋 Modified Orbitozygomatic Craniotomy for Medial Wing
Meningiomas: cadaver dissection and report of five
consecutive cases
9:20~10:00 杜永光顏玉樹
Professor
Hongo
Surgery for the Foramen Magnum Meningioma
09:50~10:00 discussion
10:00~10:30 施養性邱仲慶
杜永光 Surgical approaches to cavernous sinus lesions
10:30~10:4
5
Coffee break
10:45~11:15 高明見陳敏雄
潘宏基 Gamma Knife Surgery for the treatment of cavernous sinus
hemangioma and AV fistulas involving cavernous sinus
11:15~11:35 張承能關皚麗
侯勝博 Changing Paradigm in Skull Base Surgery- from open to
endoscopic
11:35~11:55 洪純隆陳幸鴻
沈炯祺 Neuroendoscopic history and future development
11:55~12:3
0台灣顱底外科醫學會第四屆第一次會員大會暨理監事選舉
12:30~14:0
0Lunch (中正一樓誠品生活廣場) (第三屆理監事:中正一樓蘇杭餐廳)
14:00-14:25 何青吟 張凱評 Identification of Macrophage Inflammatory Protein 3 as a
Novel Serum Marker for Nasopharyngeal Carcinoma from
cDNA microarray
14:25~14:50 邵國寧許永信
李明陽 Skull base reconstruction with free ALP flap
14:50~15:15 黃勝雄陳明德
顏玉樹 Endoscopic transnasal transclival odontoidectomy
15:15~15:40 陳翰容 劉安祥 Meningiomas of the craniovertebral junction
15:40~16:1
0
Coffee break(第四屆第一次理監事會議:選舉常務理監事及理事長 )
16:10~16:30 蘇泉發劉康渡
梁正隆 Gamma Knife Radiosurgery for skull base tumors
16:30~16:50 郭萬祐 駱子文 Gamma Knife Radiosurgery for Head and Neck Malignancy
1

任森利 Invading Base of Skull – The Tzu-chi Experience
16:50~17:05 陳冠助黃文成
張軒凱 Multiple meningiomas of different pathologic types in a
patient—a case report
17:05~17:20 蔣永孝 楊懷哲 Trigeminal Neuralgia: Review of current treatment and our
experience
17:20~17:35 鍾文裕 李政家 Vestibular evoked myogenic potential (VEMP) in
radiosurgery-treated patients with acoustic neuromas
17:35~18:00 Shuttle bus to 僑園餐廳18:00~ 晚宴
Modified Orbitozygomatic Craniotomy for Medial Wing Meningiomas: cadaver dissection and report of five consecutive cases
鄭澄懋
三軍總醫院
Abstract
Medial wing meningiomas reside on the medial sphenoid ridge, which is a one-centimeter cliff-like
bony structure where content of cavernous sinus, optic nerve, and cranial internal ceratoid artery are
closely bounded to each other. Historically, these cranial base meningiomas were treated with
traditional frontotemporal craniotomy and the outcome had not been promising largely because of the
excessive brain retraction. Cranial base approaches with modern microneurosurgical techniques yield
better results. However, these kind of cranial base approaches often cope with some extension of
zygomatic arch, which associated with somewhat morbidity. We report the methods and results of
using MOZC, without any resection of zygomatic arch, to access five consecutive large medial
sphenoid wing meningiomas.
The modified orbitozygomatic craniotomy (MORC) is a reform of skull base approach with the
characteristics of its simplicity and wide exposure. Since this approach was newly introduced to the
neurosurgical society lately in 2003, its clinical reports are few. The goal of this presentation is to
advocate its clinical feasibility. In the following five years, five consecutive patients harboring large
(> 4 cm) sphenoid wing meningiomas were treated with MORC. Total brain tumor removal was
achieved in all patients. There is no mortality in this series of follow-up. One patient was complicated
with the postoperative epidural hematoma and evacuated on the same operative day. All patients
returned to their own daily activity without neurological sequella. The MORC is the option of choice
in treating large upper-third clival lesion while the standard frontotemporal craniotomy is considered
to give less surgical rooms. To our knowledge, this is the first report of treating sphenoid wing
meningiomas with MOZC.
2

Surgery for the foramen magnum meningioma
Kazuhiro Hongo, Tetsuya Goto, Keiichi Sakai
Department of Neurosurgery, Shinshu University School of Medicine, Matsumoto, Japan
Even with the recent advancement of the skull base approaches and techniques, surgery for the
ventral foramen magnum remains challenging. To accomplish safe resection, microsurgical anatomy
of this region should be fully understood. To achieve a satisfactory result for removing the ventral
foramen magnum meningioma, adequate exposure with applying a skull base approach taken from the
inferolateral side, and gentle manipulation to dissect the tumor from the surrounding critical structures
without compressing the medulla oblongata are essential. The intraoperative electrophysiological
monitoring is also quite helpful.
In the presentation, key points for the surgical approach to this lesion as well as the anatomy of the
foramen magnum are shown. Representative cases of meningioma surgery will be presented.
3

杜永光尚缺
4

Gamma Knife Surgery for the Treatment of Cavernous Sinus Hemangiomas and AV Fistulas Involving the Cavernous Sinus
潘宏基David Hung-Chi Pan, M.D.
台北榮總神經外科Department of Neurosurgery, Taipei Veterans General Hospital
Introduction: Surgery for tumors or vascular lesions involving the cavernous sinus poses difficulty
due to the risks of excessive bleeding. This report presents our 15-year experience in Gamma Knife
surgery (GKS) for the treatment of cavernous sinus cavernous hemangiomas (CHs) and dural
arteriovenous fistulas (DAVFs). The characteristic imaging findings of CHs, differential diagnosis
from other benign tumors, radiosurgical methods, results and patients’ outcome are described.
Material and methods: A total of 444 patients with cavernous sinus lesions were treated by GKS at
the Taipei VGH between 1993 and 2008. Among them 265 were neoplasms and 179 were DAVFs.
Cavernous sinus hemangiomas account for 2% (6 patients) of all tumors in the cavernous sinus. These
rare but difficult tumors can be distinguished from more commom meningiomas based on the
characteristic MR finding that T2-weighted images show marked hyperintensity. The median age of
CH patients was 49y/o. Female was predominant with a male/female ratio of 2/4. Pre-treatment
manifestations included headache, visual loss, oculomotor and abducence palsies. Tumor volume
ranged 2.9-23.1ml. During radiosurgery, precise stereotactic targeting and irradiation using multiple
small shots to obtain a conformal, high-dose treatment were achieved. Average marginal / maximum
dose were 13/23 Gy respectively.
For the 179 DAVF patients, GKS was applied to treat AV shunts involving the wall of the
cavernous sinus. Feeders on the dural wall both from ICA and ECA were irradiated while optic nerves
were carefully protected. After treatment, patients were regularly followed by MRI/MRA and doppler
ultrasound to assess flow of the superior ophthalmic veins. Cerebral angiography was performed 2
years post-treatment to verify complete obliteration.
Results: Five of six cases with CHs had received regular MRI follow-up study (FU range 6-156,
mean 40 months). Clinically, all patients showed remarkable symptomatic improvement with
resolution of headache, diplopia or visual impairment. There was no complication or mortality. Tumor
volume measurement in follow-up MRI showed 80% reduction of the volume, with rapid regression
of the tumor within 3-6 months. For comparison, the average volume change of our 84 meningiomas
only showed 29% reduction. The statistical difference of volume changes between CHs and
meningiomas was significant (p=0.0023).
For the DAVF patients, 90% showed clinical improvement with disappearance of red eyes,
chemosis, or double vision. Follow-up in 105 patients based on Kaplan-Meier study showed 70% cure
rate in the first year and 90% in the second year. There was 6% with persisted symptoms or recurrence
2 years post-treatment.
Conclusion: GKS is a safe and effective alternative treatment for cavernous sinus hemangiomas and
dural AV fistulas. The characteristic MRI findings of CH before and after GKS allow us to select
proper cases for the treatment.
5

Changing Paradigm in Skull Base Surgery- from open to endoscopic
Sheng-Po Hao MD, FACS, FICS
Professor & Chairmen, Department of Otolaryngology Head and Neck
Chang Gung Memorial Hospital
Chang Gung University
Surgical approach is the cornerstone of a successful skull base surgery. For the anterior cranial base
lesions, craniofacial resection is the standard approach.
However, with the modern development of endoscope and vast advance of technology in navigation
system, an open wide field approach which usually carries unavoidable morbidity is no longer always
considered feasible. Rather, endoscopic approach, endoscopic resection and encoscopic reconstruction
seems justified if the oncological results is not inferior to open method. However, we have to keep in
mind that the only thing changed in endoscopic resection is the way to remove the tumor,
nevertheless, the extent of resection and the control of surgical margin remain exactly the same with
the open method. Thus, we may reach the same oncological results but having fewer surgical
morbidity. The future trend is to change the paradigm in skull base surgery from open to endoscopic.
6

沈炯祺尚缺
7

Identification of Macrophage Inflammatory Protein 3 as a Novel Serum Marker for
Nasopharyngeal Carcinoma from cDNA microarray
Kai-Ping Chang, M.D., Ph.D.; Ku-Hao, Fang, M.D.; Sheng-Po Hao, M.D., FACS
張凱評, 方谷豪, 侯勝博Department of Otolaryngology-Head & Neck Surgery, Chang Gung Memorial Hospital, Lin-Kou
Medical Center, Tao-Yuan, Taiwan
長庚紀念醫院林口醫學中心耳鼻喉部頭頸外科
Introduction: From differential expression profiles analyzed using cDNA microarray between paired
nasopharyngeal carcinoma (NPC) and pericancerous normal epithelium, we identified two sets of
genes which were up-regulated/ down-regulated in NPC tumors and associated with immune
response. Among these genes, we found the most up-regulated gene, macrophage inflammatory
protein (MIP)-3 might be a potentially novel tumor marker. We herein examine whether MIP-3 is a
biomarker for NPC, and whether it is involved in modulating NPC cell functions.
Materials & Methods: The study population comprises 275 NPC patients and 250 controls. MIP-3 levels in tissues and sera were examined by immunohistochemistry and ELISA, respectively. EBV
DNA load and EBV VCA IgA were measured by qRT-PCR and immunofluorescent assay,
respectively. MTT assays were done to investigate the role of MIP-3 on NPC cell proliferation.
Effects of MIP-3 on NPC cell motility were investigated by trans-well migration/invasion assays and
RNA interference.
Results: MIP-3 was over-expressed in NPC tumor cells. Serum MIP-3 levels were significantly
higher in untreated patients, recurrent patients and patients with distant metastases versus non-NPC
controls, patients with complete remission, and long-term disease-free patients. In the prospective
cohort, serum MIP-3 levels were significantly higher in untreated NPC patients with advanced TNM
stage versus early stage, and also correlated with EBV DNA load. Measurement of MIP-3, EBV
DNA and VCA IgA levels in serial serum/plasma samples from treated patients at 6-month intervals
revealed a high association between MIP-3 level, EBV DNA load and disease status. Among 155
consecutive NPC patients, subjects with pre-treated MIP-3 serum levels over 65 pg/ml had worse
prognoses for overall survival and distant metastasis-free survival in univariate and multivariate
analysis. Additionally, cell functional assays showed that MIP-3 had no obvious effect in the NPC
cell proliferation but contributed to migration and invasion of NPC cells, which could be effectively
inhibited by MIP-3 knock-down.
Conclusions: From the analysis derived from the results of cDNA microarray, we discovered the up-
regulation of MIP-3 and found that MIP-3 may be a novel biomarker and prognosticator for NPC
and is involved in migration and invasion of NPC cells.
Anterior Skull Base Reconstruction with Free Anterolateral Thigh Flap – NCKUH Experience
前側大腿皮瓣重建顱底缺損:成大醫院之經驗
Ming-Yang Lee E-Jian Lee8

Division of Neurosurgery, Department of Surgery, National Cheng- Kung University Hospital
李明陽 李宜堅成大醫院神經外科
Summary
Defects at the anterior skull base were not commonly found after head trauma and skull base tumor
resection. Reconstruction of the anterior skull base defect is paramount to prevent postoperative
complications such as cerebrospinal fluid (CSF) leakage and meningitis ascending infection from
underlying aerodigestive tract. Several reconstructive methods of the anterior skull base have been
reported .
From February 2004 to July 2008 the anterior skull base reconstructions were performed in 17
patients. In 9 patients the defects were related to the head and neck tumors and 8 patients related to the
severe head trauma with comminuted fractures in the anterior cranial base. Reconstructions with
galeopericranial flaps were used in fifteen patients and free anterolateral thigh (ALT) flap were
performed in two patients due to large head and neck defect and reoperation. There were no CSF
leakage and postoperative meningitis.
By a multidisciplinary surgical team approach, there is an increasing role for reconstruction of
complex anterior cranial base resection defects using microvascular surgical techniques.
9

Endoscopic Trans-nasal Trans-clival Odontoidectomy: A New Approach to Decompression
Jau-Ching Wu, M.D.1,2,3,4, Wen-Cheng Huang, M.D.1,2,3, Henrich Cheng, M.D., Ph.D.1,2,3,4 , Mu-Li Liang, M.D.1,3, Ching-Yin Ho, M.D., Ph.D.3,5, Yang-Hsin Shih, M.D.1,3, Yu-Shu Yen M.D.1,3
Objectives:
Endoscopic trans-nasal trans-clival resection of the odontoid process is less invasive than the standard
trans-oral odontoidectomy. We describe here our techniques that are less invasive but provided
successful decompression.
Presentations:
From September 2004 to April 2007, three consecutive patients with basilar invagination and
instability in the cranio-vertebral junction were enrolled in this report. The etiologies included
rheumatoid arthritis in two and trauma in one, and all presented with myelopathy and quadriparesis
prior to the interventions.
Interventions:
All of the three patients underwent an endoscopic trans-nasal trans-clival approach for anterior
decompression and resection of the displaced odontoid process and pannus, in order to decompress the
underlying medulla. Subsequently, they received occipital-cervical fixation by lateral mass screws and
bone fusion to ensure stability. Remarkable neurologic recovery was observed after surgery in all and
no adverse effects were noted.
Conclusions:
Compared to the standard trans-oral approach, the trans-nasal trans-clival endoscopic approach for
decompressing basilar invagination is a feasible and effective alternative that avoids common
disadvantages like prolonged intubation, excessive tongue retraction, and need for palatal incision.
10

Meningiomas of the craniovertebral junction
Ann-Shung Lieu, Shiuh-Lin Hwang and Shen-Long Howng
顱脊椎處腦膜瘤
劉安祥 黃旭霖 洪純隆Department of Neurosurgery, Kaohsiung Medical University Hospital
高雄醫學大學附設醫院 神經外科
Tumors of the foramen magnum are found infrequently and, due to their insidious onset, they resemble degeneration diseases of the central nervous system. Meningiomas are the most common benign tumors of the foramen magnum. They represent about 1.8% of all meningiomas. Most of these lesions can be resected using traditional posterior approaches, but some anterior and anterolateral lesions are difficult to be resected via traditional methods due to inadequate exposure. Therefore, management of lesions situated in the anterior foramen magnum, lower livus, and anterior aspect of the upper cervical area is a challenging issue for neurosurgeon. Mehtods of treating these lesion includes transoral, transuncodiscal, and lateral suboccipital approaches, the last of which has undergone several modifications including the for-lateral suboccipital, dorsolateral suboccipital transcondylar, and extreme lateral transcondylar variations. Lateral suboccipital approaches and modificational exposure can be satisfactory with minimal or no retraction of important neurovascular structures in the region.
11

Gamma Knife Radiosurgery for Skull Base Tumors
Cheng-Loong Liang, Kang Lu, Han-Jung Chen
Department of Neurosurgery, E-Da Hospital, I-Shou University, Kaohsiung
Tumors located at the skull base are among the most difficult problems that neurosurgeons
encounter. Management of patients with skull base tumors must take into account that complete tumor
removal is not possible with acceptable morbidity in many patients. Therefore, radiation therapy and
stereotactic radiosurgery (SRS) are commonly performed. The use of radiosurgery for patients with
skull base tumors has increased significantly over the past two decades. The goal of radiosurgery is
cessation of tumor growth and preservation of neurological function. The technique of radiosurgery
has evolved due to improved imaging, better radiosurgical devices and software, and the continued
analysis of results. In this report, the authors discuss technical concepts and present the preliminary
results of skull base radiosurgery treated by Gamma knife in E-Da hospital.
At our center we used Gamma Knife SRS for a variety of benign, extraaxial basal tumors. These
included schwannomas, meningiomas, hemangiomas, pituitary adenomas, craniopharyngiomas. For
properly selected patients with benign tumors (meningiomas, schwannomas, glomus tumors), tumor
control rates between 90 and 100% have been reported. Radiosurgery is also commonly performed for
patients with malignant skull base tumors as a palliative treatment and symptom relief is common,
especially for patients with cranial nerve involvement related to their tumor.
12

Gamma Knife Radiosurgery for Head and Neck Malignancy Invading Base of Skull – The Tzu-chi Experience
Tzu-wen Loh 1 , Tsung-lang Chiou1, Pao-sheng Yen2, Dai-wei Liu3, Peir-rong Chen4, Chain-fa Su1
駱子文 1 , 邱琮朗 1, 嚴寶勝 2, 劉岱瑋 3, 陳培榕 4, 蘇泉發 1
Department of Neurosurgery1, Department of Radiology2, Department of Radiation-Oncology3,
Department of Otolaryngology4, Buddhist Tzu-Chi Medical Center, Hualien, Taiwan, R.O.C.
花蓮慈濟醫學中心 神經外科 1, 影像醫學科 2, 放射腫瘤科 3, 耳鼻喉科 4
Introduction: Although less common, local invasion of head and neck malignancy into skull base
might be disclosed. This kind of extension remains challenging to skull base surgeons because of
vulnerability of nearby vital neurological strutures. Fortunately, lots of head and neck malignancy are
radio-sensitive. Thus, Gamma knife radiosurgery might hold an evolving position in treatment of
extensive skull base invasion of head and neck malignancy.
Materials & Methods: From November 2003 to August 2008, 10 patients with local skull base
invasion of head and neck malignancy were referred from our otolaryngology department. Before
referral, operations for radical excision were all applied to these patients. There were 3 women and 7
men in this group, and the mean age was 46.7 years old. The entities of disease diagnosis included
NPC in 3, buccal cancer in 2, hypopharyngeal cancer in 2, parotid gland tumor in 1, and salivary gland
neoplasm in 1 patient, and another patient suffered from olfactory neuroblastoma. The mean tumor
volume of skull base extension was 12.8 c.c. (range: 8.8 to 36.8 c.c.). Gamma knife radiosurgery was
arranged to these patients and the mean prescription dosage was 18.6 Gy (range: 18 to 20 Gy). Some
extensive tumor masses were so close to optic apparatus that dosage of 8 Gy was adapted as safe
upper limit of irradiation within the optic apparatus.
Results: The follow-up periods in these patients were 11 to 28 months. 5 patients encountered
mortality during follow-up due to primary disease progression. No marked neurological deficits were
noted within these patients.
Conclusions: From our preliminary experiences, Gamma knife radiosurgery might be a safe and
useful tool when dealing with local skull base invasion of head and neck malignancy. It might also be
put into consideration of co-operation between otolaryngologists and neurosurgeons, especially when
the skull base extension was around cavernous sinus, optic apparatus, or other important but
vulnerable structures. The long-term follow-up and evaluation is, nevertheless, still in necessity.
13

Multiple meningiomas of different pathologic types in a patient: a case report
Hsuan-Kan Chang, MD Li-Yu Fay, MD Chun-Fu Lin, MD Min-Hsiung Chen, MD, PhD
張軒侃, 費立宇, 林俊甫, 陳敏雄
Department of Neurosurgery, Neurological Institute,
Taipei Veterans General Hospital, Taipei, Taiwan, R.O.C.
台北榮總神經醫學中心神經外科
Abstract:
Multiple meningiomas(MM) are considered rare disease entity, which accounts for 5.9-10.9% of all
meningiomas from literature review. Most MM removed from the same person showed identical
pathological subtype. The authors report a case of multiple meningiomas with different pathologic
subtypes. The patient is a 67-years-old female with the initial presentation of right eye ptosis. MRI
revealed four spatially separated meningiomas located at right parasagittal, bilateral cavernous
sinuses, and left planum sphenoidale, respectively. The surgeons removed three of them in one
operation and pathology showed three different subtypes of meningiomas, namely meningothelial,
fibrous, and secretory types. Special immunohistochemistry such as progesterone receptor(PR), p53,
and MIB-1 LI were performed and compared with literature results.
14

Trigeminal Neuralgia: Review of current treatment and our experience
楊懷哲 劉康渡 鐘文裕 潘宏基
台北榮總神經外科
Trigeminal neuralgia (TN) is the most common facial neuralgia, and is considered to be one of the
most painful conditions to affect patients. TN is generally characterized by lancinating, unilateral,
paroxysmal pain occurring in the distribution of the fifth cranial nerve. Generally, TN can be diagnosed
by the typical patient history, a negative neurologic exam, and response to a trial of carbamazepine.
Imaging studies should be considered if the diagnosis is uncertain or neurologic abnormalities are
noted. Most cases are caused by compression of the trigeminal nerve root, usually within a few
millimeters of entry into the pons. The treatment modalities for the management of TN may be divided
into medical, surgical, and gamma-knife radiosurgery. Generally, response to drug therapy is good,
with over 80% of patients responding to some of the anticonvulsants. Percutaneous approaches to
trigeminal gangliolysis are considered to have less associated risk and less cost than open surgical
procedures. Open surgical procedures used in the treatment of TN include microvascular
decompression of the trigeminal root and retrogasserian rhizotomy. Additionally, because both of
these procedures have greater associated risks, morbidity, and mortality, they are customarily applied
only to younger patients in good health. Stereotactic radiosurgery has been established as an
alternative treatment for patients who do not respond to optimal medical management.
We began use of this technique at our center in 1995 and have evaluated outcomes serially.
Independently acquired data from 207 patients with idiopathic TN that had Gamma Knife radiosurgery
was reviewed. 29 patients received twice Gamma-kinfe treatment and 2 patients received three times
due to recurrent pain.The maximal radiosurgery dose was 80 Gy with a range of 70 to 90 Gy. One
hundred patients (48.3%) had prior surgery or radiofrequency treatment. Patients were followed to a
maximum of 10.5 years (mean, 28 months). Complete or partial pain relief was achieved in 58.5% of
patients at 1 year. The absence of prior surgery correlated with an increased proportion of patients in
complete or partial pain relief over time (65.4%). 5.8% of patients developed new or increased
subjective facial paresthesia or facial numbness. Radiosurgery for idiopathic TN was safe and effective
and is an important addition to the surgical armamentarium for TN.
15

Vestibular evoked myogenic potential (VEMP) in acoustic neuromas treated by Gamma-knife radiosurgery --- preliminary study
聽神經瘤經伽馬刀治療後之前庭誘發肌性電位---初步研究
李政家 楊懷哲 劉康渡 鍾文裕 潘宏基 王懋哲 蕭安穗台北榮民總醫院 神經外科 耳鼻喉科
Introduction The ventricular evoked myogenic potential (VEMP) test showed abnormal results in
80% of acoustic neuroma (AN). Although the sensitivity of VEMP was lower than that of ABR test, it
is useful in neurophysiology to classify the origin of ANs. Besides, pure tone audiogram (PTA) and
Calori test give us additional information to differentiate the nature of ANs. In this preliminary study,
we hope to study the VEMP in ANs treated by Gamma-knife radiosurgery.
Patients and methods Ten AN patients was recruited, and we performed PTA, Calori test, and
VEMP. We defined 30dB loss as abnormal PTA finding, canal paralysis (Jonkees’ formula) > 20% as
abnormal Calori test, and evoked potential ratio (EPr) >30% as abnormal VEMP results. We also
calculate the volume of tumors, to correlate the results of PTA, Calori, and VEMP test. Finally,
compare pre-GKS and post-GKS VEMP (EPr) results.
Results The PTA, Calori test , and VEMP test showed abnormal results in 80%, 60% and 60% ANs,
respectively. Hearing impairment, tinnitus, and dizziness were happened in 90%, 70%, 60% ANs,
respectively. PTA, Calori test, and VEMP results were not correlated each other. The larger tumor, the
more severe results in PTA, Calori test, and EPr were found. The tumor volume can be calculated = -
0.875 + 1.040*(PTA) + 2.350*(Calori test) + 2.175*EPr. Finally, all tests (PTA, Calori test, and
VEMP) are progressing in first month followed-up after Gamma knife radiosurgery.
Discussion All three tests can help use to differentiate the nature of tumors. The three tests are
independent in the small volume of tumor, although all tests are abnormal in large volume of tumor.
Our followed-up post radiosurgery still in proceed, and need more time to observe the outcome of the
ventricular functional recover.
*********************************************************************************
16

9:00~9:20
Name: 鄭澄懋 Cheng-Mao Cheng
(Also known as: Robert C.M. Cheng)
Professional Address: Division of Neurological Surgery
Tri-Service General Hospital,
e-mail: [email protected]
Date of Birth: 18 August, 1964
Education:
1990 Bachelor of Medicine
National Defense Medical Center, Taipei, Taiwan
Speical Training:
1988- 1990 Medical Internship
Tri-Service General Hospital, Taipei, Taiwan
1992- 1994 General Surgery
Tri-Service General Hospital, Taipei, Taiwan
1994-1997 Neurological Surgery Residency
Tri-Service General Hospital, Taipei, Taiwan
1997-1998 Neurological Surgery Chief Resident
Tri-Service General Hospital, Taipei, Taiwan
1998-1999 Visiting doctor of Neurological Surgery,
Pen-Hoo Army Hospital, Pen-Hoo, Taiwan
1999-2000 Attending doctor of Neurological Surgery,
Tri-Service General Hospital, Taipei, Taiwan
2001-2002 Reaserch fellowsip in skull base surgery and neuroradiology in Oregon Health &
Science University
2002-2007 Attending doctor of Neurological Surgery,
Tri-Service General Hospital, Taipei, Taiwan
Activity:
Member of Surgical Association, Republic of China
Member of Neurosurgical society, Taiwan
Interests: Mountain climbing, fishing, photography.
17

Research Experience:
1. Skull base Surgery
2. Spinal cord repair on rat
Division of Neurological Surgery
Tri-Service General Hospital
Advisor: Shinn-Zong Lin, Ph.D.
Presentation:
1. Cheng-Mao Cheng, Shinn-Zong Lin, Yung-Hsiao Chiang, Ming-Ying Liu:
Correlation of monitoring of laser Doppler flowmetry and intracranial pressure in severe head-
injuried patients: a preliminary result in Tri-Service General Hospital
Annual meeting of Surgical Society,R.O.C., 1998
Presented by Cheng-Mao Cheng
2. Cheng-Mao Cheng, Shinn-Zong Lin, Yung-Hsiao Chiang, Ming-Ying Liu:
Intracranial pressure monitoring in severe head-injured patients: a practical method
in delineation of adequate cerebral perfusion pressure and the preliminary result in Tri-Service
General Hospital.
11th Internaional Congress of Neurological Surgery, July 1997
Presented by Cheng-Mao Cheng
3. Cheng-Mao Cheng, Shinn-Zong Lin, Yung-Hsiao Chiang, Ming-Ying Liu:
The application of the stereotactiv craniotomy with removal of tumor under laser guide
Annual meeting of Surgical Society,R.O.C., 1997
Presented by Cheng-Mao Cheng
4 Cheng-Mao Cheng, Rochey Chao, Shinn-Zong Lin, Ming-Ying Liu:
Posterior atlantoaxial interarticular screw fixation as an alternative option for treatment of
type II Odontoid Fracture complicated by failure of anterior odontoid screw fixation—a case
report
Annual meeting of Surgical Society, R.O.C., 1996
Presented by Cheng-Mao Cheng
5. Cheng-Mao Cheng, Gregory J Anderson, Frank Hsu, Akio Noguchi, Aclan Dogan, Sean O
McMenomey:
Quantitative comparison of the supraorbital keyhole, pterional and supraorbital subfrontal
approaches to the parasellar region
Annual Meeting of North America Skull Base Society, California, USA, 2002
Presented by Cheng-Mao Cheng
6. Cheng-Mao Cheng, Frank Hsu, Akio Noguchi, Aclan Dogan, Sean O McMenomey, Johnny
B Delashaw:
Topography of skull base in relation to fisher’s segmental nomenclature of intracerebral
18

artery
Annual Meeting of North America Skull Base Society, California, USA, 2002
Presented by Cheng-Mao Cheng
Publication:
1. Cheng-Mao Cheng , Ming-Ying Liu, Bao-Chiien Chang, Cheng-Ti Cheng. Detection of radiation necrosis with Thallium-201 and
Technetium-99m DTPA single-photon emission computed tomography in a patient with irradiated malignant glioma. Annal of
Nuclear Medicine and Sciences.Vol. 10, No. 1, 5-8, 1997
2. Cheng CM , Chiang YH, Fan YM, Huang WS, Cheng CY. Localization of Abscess in Dural Graft with Fusion Image of Gallium-67
CT-SPECT. 核子醫誌 17:225-228, 2004
3. Cheng CM , Alpha fetoprotein producing immature teratoma of the pinel region without components of endodermal sinus tumour. J
of Clin Neuroscience 13: 257-259, 2006
4. Vijayabalan Balasingam , Gregory J Anderson , Neil D Gross , Cheng-Mao Cheng , Akio
Noguchi , Aclan Dogan , Sean O McMenomey , Johnny B Delashaw Jr , Peter E
Andersen. Anatomical analysis of transoral surgical approaches to the clivus.
J Neurosurg. 2006 Aug ;105 (2):301-8
19

9:20~10:00
Name: Kazuhiro Hongo, M.D., Ph.D.Address (office): Professor and Chairman
Department of Neurosurgery
Shinshu University School of Medicine
3-1-1 Asahi, Matsumoto 390-8621, Japan
Tel : +81-263-37-2690, Fax: +81-263-37-0480
E-mail: [email protected]
Date of Birth: December 10, 1953
Citizenship: Japanese
Medical School: Shinshu University School of Medicine
(April, 1974 - March, 1978)
Postgraduate Training & Professional Career:
1978 Junior Resident, Dept. of Neurosurgery, Shinshu Univ. School of Medicine
1979 Rotating Intern, Anesthesiology, Shinshu Univ. School of Medicine
1980 Fellow in Pharmacology, Shinshu Univ. School of Medicine
1981 Chief, Dept. of Neurosurgery, Matsumoto National Hospital
1982 Chief, Dept. of Neurosurgery, Shinonoi General Hospital
1984 Staff, Dept. of Neurosurgery, Shinshu Univ. School of Medicine
1986 Research Fellow, Dr. Kassell’s Cerebrovascular Research Laboratory, Dept. of Neurosurgery,
University of Virginia, USA
1988 Chief, Dept. of Neurosurgery, Showa-Inan General Hospital
1992 Assistant Professor, Dept. of Neurosurgery, Shinshu Univ. School of Medicine
1994 Associate Professor, Dept. of Neurological Surgery, Aichi Medical University
2001 Associate Professor, Dept. of Neurosurgery, Shinshu Univ. School of Medicine
2003 Professor and Chairman, Dept. of Neurosurgery, Shinshu Univ. School of Medicine
Fields of Research and Academic Interest:
Microsurgery of cerebrovascular diseases (AVM, aneurysm),
Skull base surgery (meningioma, neurinoma, etc.)
Microvascular decompression
Robotics surgery
Pharmacological research on cerebral vasospasm
20

10:00~10:30
Yong-Kwang Tu, M.D.,Ph.D.Birth Date:
April 9, 1948
Marital Status:
Married with 2 children (Spouse: Tso-Hsien Tu)
Current position:
Professor and Chairman, Department of Neurosurgery,
College of Medicine and Hospitals, National Taiwan University, Taipei, Taiwan
Medical education:
1976 M.D. School of Medicine, National Taiwan University, Taipei
1984 Ph.D. Institute of Clinical Medicine, National Taiwan University, Taipei
Postdoctoral training:
1976-1977 Resident in Internal Medicine
National Taiwan University Hospital, Taipei
1977-1980 Resident in Surgery (Neurosurgery)
National Taiwan University Hospital, Taipei
1980-1981 Chief Resident in Neurosurgery
National Taiwan University Hospital, Taipei
1984-1988 Fellow in Neurosurgery, Massachusetts General Hospital and
Harvard Medical School, Boston, U.S.A.
Academic Appointments
1987-1988 Instructor in Surgery (Neurosurgery), Harvard Medical School,
Boston, U.S.A.
1989-1991 Associate Professor in Neurosurgery (Non-tenure), National
Taiwan University
1991-1998 Associate Professor in Neurosurgery (Tenure), National Taiwan
University
1998- Present Professor in Neurosurgery (Tenure), National Taiwan University
2004- Present Chairman, Department of Neurosurgery, National Taiwan University
Other Appointments:
1982-1983 Chief, Department of Neurosurgery, King Fahd Hospital (Jeddah General
Hospital), Kingdom of Saudi Arabia21

1998-1999 Vice-President, Provincial Taoyuan Hospital, Taoyuan, Taiwan
1999-2000 President, Municipal Chung-Hsin Hospital of Taipei
2000-2001 Director, Taipei Stroke Center
Academic Societies:
2000-2002 Secretary General, International College of Surgeons
2001-2003 President, Taiwan Stroke Society
2001-2004 President, Asian-Oceanian Society for Skull Base Surgery
2003-2005 President, Taiwan Society for Skull Base Surgery
2005-2007 President, Taiwan Neurosurgical Society
2006-2009 President, International Congress on Cerebrovascular Surgery
2007-2011 President, Asian-Australasian Society of Neurological Surgeons
2009-2012 Second Vice President, World Federation of Neurosurgical Societies
22

10:45~11:15
Name: David Hung-Chi Pan, M.D.
Birth Date: Nov. 9, 1947, Male, Birth Place: Taiwan
Present Position:
(1) Director, Gamma Knife Center, Neurological Institute,
Taipei Veterans General Hospital, 1993 till now
(2) Chief, Division of Functional Neurosurgery, Neurological Institute, Taipei Veterans General
Hospital, 1989 till now
(3) Professor of Surgery, Faculty of Medicine, National Yang-Ming University, 2003 till now
(4) Delegate, Radiosurgery Committee, World Federation of Neurological Surgery (WFNS).
(5) President, Taiwan Society for Skull Base Surgery, 2007-2008
Experience:
(1) Resident, Department of Surgery, Taipei Veterans General Hospital, 1974-1977
(2) Attending Neurosurgeon, Neurological Institute, Taipei Veterans General Hospital,
1979-1989
(3) Clinical Fellow, Department of Neurosurgery, Karolinska Hospital, Sweden, 1981-1982
(4) Associate Professor, Faculty of Medicine, National Yang-Ming University, 1985 – 2003
Education: (1) Taipei Medical University, Taipei, Taiwan, 1966-1973
(2) Karolinska Institute, Stockholm, Sweden, 1981-1982
Society Membership:
(1) World Society for Stereotactic and Functional Neurosurgery since 1989
(2) International Stereotactic Radiosurgery Society since 1992
(3) Leksell Gamma Knife Society since 1992
(4) World Federation of Neurological Surgery, Radiosurgical Committee since 1995
(5) Taiwan Neurosurgical Society since 1993
(6) Chinese Medical Association (Taipei) since 1974
(7) Surgical Association, Taiwan since 1974
23

11:15~11:35
一、 基本資料 簽 名:
中 文 姓 名 侯 勝 博 英 文 姓 名HAO SHENG-PO
(Last Name) (First Name) (Middle Name)
國 籍 中華民國 性 別 男 □ 女 出生日期 1959 年 06 月 30 日聯 絡 電 話 (公).03-3281200 EXT 3966 (宅).02-27602407
傳 真 號 碼 03-3979361 E-MAIL [email protected]
二、 主要學歷 請填學士級以上之學歷或其他最高學歷均可,若仍在學者,請在學位欄填「肄業」。
畢/肄業學校 國別 主修學門系所 學位 起訖年月(西元年/月)
台北醫學院 中華民國 醫學系 醫學士 1978/ 09 至 1985/ 07
/ 至 /
/ 至 /
三、現職及與專長相關之經歷 指與研究相關之專任職務,請依任職之時間先後順序由最近者
往前追溯。服務機關 服務部門/系所 職稱 起訖年月(西元年/月)
現職: /
財團法人長庚紀念醫院 耳鼻喉部 副教授部長
2005/07至今
經歷: / 至 /
孫逸仙癌症中心 耳鼻喉科、頭頸外科 主任 1995/ 07 至 1997/07
財團法人長庚紀念醫院 耳鼻喉科 主治醫師 1989/ 07 至 1995/06
美國 Cornell University Memorial Sloan-Kettering
Cancer center
研究員 1993/ 06 至 1993/06
美國匹茲堡大學 耳鼻喉、頭頸外科及顱底醫學中心
研究員 1992/ 09 至 1993/06
四、專長 請自行填寫與研究方向有關之學門及次領域名稱。
鼻咽癌 口腔癌 顱底手術 頭頸部腫瘤
24

11:35~11:55
姓 名 : 沈炯祺 Chiung-Chyi Shen
性 別 : 男
出生日期 : 1961年2月18日
學 歷 : 國防醫學院80期畢業(76年班)
職 稱 : 台中榮總神經外科 主任
國立陽明醫學大學專任助理教授
國立國防醫學大學兼任助理教授
教師資歷 : 助教授字第007871號 (教育部)
求學及經歷
76年 畢業(大字第027214號)後分發至台中榮總擔任住院醫師,接受神
經外科專科醫師訓練,並通過醫師執照考試(醫字第015879號)
80年 升任神經外科住院總醫師
80年 通過外科專科醫師考試 (外專醫字第2709號)
81年 升任神經外科主治醫師
81年 獲選為台中榮民總醫院臨床教學績優醫師
82年 通過神經外科專科醫師考試 (神外專字第000257號)
82年 轉任台中空軍總醫院神經外科主任醫師
83年 借調嘉義榮民醫院神經外科主治醫師
84年 通過公務人員高等考試(全高字第3293號)
87年 獲選台中市優良醫師特殊貢獻獎25

87年 於中國醫藥學院醫學系授課
88年 上學期於中國醫藥學院醫學系授課
88.08 ~ 89.07赴美國哈佛大學附設醫院 麻省總醫院神經外科進修
89年 回國擔任神經外科主治醫師
90年至今於弘光科技大學授課
92年 於中山醫科大學醫學系授課
92年 於國立暨南大學生命科學研究所授課
93年 台中榮總神經外科主任
26

14:00-14:25
張凱評醫師 Kai-Ping Chang, MD, PhD
學歷:
長庚大學醫學系醫學士長庚大學醫學博士美國醫師資格 ECFMG證書
經歷:
長庚醫院林口醫學中心耳鼻喉部總醫師台灣耳鼻喉專科醫師台灣臨床腫瘤專科醫師台灣顱底外科醫學會創始會員
現任:
長庚醫院耳鼻喉部頭頸腫瘤外科主治醫師 長庚大學醫學系助理教授台灣頭頸部腫瘤醫學會理事美國耳鼻喉頭頸外科學會會員美國癌症研究協會會員
專長:
口腔癌手術 鼻咽癌治療 喉癌,下咽癌外科治療 頭頸部腫瘤外科頭頸癌分子醫學研究一般耳鼻喉科
27

14:25~14:50
姓 名:(中文) 李明陽Name:(英文) Ming-Yang Lee
(個人照片)職 稱:□ Professor □ Associate professor ■ Assistant professor
□ Lecturer ■醫師 _□Others________
單 位:(中文) 國立成功大學醫學院附設醫院外科部神經外科(英文): Department of Surgery, National Cheng-Kung University
Hospital
Appointments(現職):Clinical Assistant Professor in Surgery (Neurosurgery),
National Cheng Kung University Medical School.
Address : Neurosurgical Service, Department of Surgery (Neurosurgery),
National Cheng Kung University Medical Center and Medical School.
138 Shen-Li Road, Tainan, Taiwan.
E-mail: [email protected]
TEL:06- 235-3535 ext 5181 FAX:06- 276-6676
Education (學位):Ph.D. candidate: Biomedical Engineering, National Cheng Kung
University, Tainan, Taiwan.
Professional activities (經歷)
Fellowship in Neurological & Neurosurgical Departments, University of
Massachusetts Medical School, Worcester, MA, USA
Fellowship in Neurosurgical Departments, Brigham & Women Hospital, Boston,
MA, USA
Research Interest (研究興趣):
1. Biomechanics of Spine 2. Neurooncology 3. Cerebral blood flow and metabolism
28

14:50~15:15
Name: Yu-Shu Yen ( 顏玉樹 )
Date of Birth: October 10, 1962
Sex: Male
Birthplace: Chya-Yi, Taiwan, R.O.C. (中華民國,台灣,嘉義縣)
Citizenship: Taiwan, Republic of China
Family: Married, one son and one daughter
Office Address: Department of Neurosurgery,
Neurological Institute,
Veterans General Hospital-Taipei
No. 201, Sec 2, Shih-Pai Road,
Shih-Pai, Taipei, Taiwan 112
Republic of China
Telephone: (O) 886-2-8757491 ext. 9, 886-2-8712121 ext. 3147
Fax No.: (O) 886-2-8757588
Education:
7/1981 - 6/1988 Medical Department of China Medical College, Taichung, Taiwan
Internship: Chang-Gung Memorial Hospital, Lin-Cou, Taipei, Taiwan (July
1986 - June 1988)
Postgraduate Training:
7/1988 - 6/1990 Rotating Surgical Resident
Department of Surgery, Chang-Gung Memorial Hospital, Lin-Cou,
Tao-Yuan
7/1990 -6/1993 Neurosurgical Resident
Department of Neurosurgery, Neurological Institute, Taipei Veterans
General Hospital
7/1993 -6/1994 Chief Resident in Neurosurgery
Department of Neurpsurgery, Neurological Institute, Taipei Veterans
General Hospital
7/1996 – 6/1997 Research fellow in Neurosurgical and Pharmacology Departments, Shinshu
University School of Medicine,
Matsumoto, Japan
29

Hospital Appointments:
Since Feb. 1995 Attending Neurosurgeon
Department of Neurosurgery, Neurological Institute, Taipei
Veterans General Hospital
Academic Appointments:
Since July 1993 Lecturer of Neurology and Neurosurgery
National Defense Medical College, Taipei, Taiwan, R.O.C.
Since July 1993 Lecturer of Surgery
National Yang-Ming Medical College, Taipei, Taiwan,R.O.C.
Present Clinical Assistant Professor of Neurosurgery
National Defense Medical College, Taipei, Taiwan, R.O.C.
Present Clinical Assistant Professor of Neurosurgery
National Yang-Ming University, School of Medicine
Membership in Academic and Professional Organization:
Member of Surgical Association, Republic of China
Member of Neurological Society, Republic of China (Taiwan)
Member of Neurosurgical Association, R.O.C. (Taiwan)
Member of Taiwan Neurospinal Society
Member of Taiwan Neurooncology Society
Member of Taiwan Skull Base Society
Member of Taiwan Endoscope Society
Member of Taiwan Stroke Society
Organization of National Academic Society
July 2001 ~ June 2003 Vice Secretary General of Taiwan Neurospinal Society
Dec 2001 ~ Nov 2003 Vice Secretary General of
Neurosurgical Association, R.O.C. (Taiwan)
March 2003 ~ Feb 2005 Secretary General of Taiwan Stroke Society
Dec 2003 ~ Nov 2005 Secretary General of Taiwan Neurooncology Society
March 2005 ~ Board of directors of Taiwan Stroke Society
Organization of International Conferences/Symposia
Secretary General of the 4th Meeting of the Asian Society for Neuro-Oncology, Taipei (Grand Hotel),
Taiwan, November 4 ~ 6, 2005
Secretary General of 34th Annual Meeting of the International Society for Pediatric Neurosurgery (ISPN),
Taipei(Grand Hotel), Taiwan, September 10 ~ 14, 2006
30

15:15~15:40
一、基本資料
中文姓名 劉安祥 英文姓名Lieu Ann Shung
性別 男 出生年月日 51 年 8 月 21 日
E-mail [email protected]二、主要學歷
畢業學校 國別 主修學們系所 學位 起訖年月
高雄學大學 中華民國 醫學系 學士1981/09~1988/06
三、現職及專長
服務機關 服務部門 職稱 起訖年月
現職:
高雄醫學大學附設醫院 神經外科
加護病房
主任 2006~迄今
高雄醫學大學附設醫院 神經外科 主治醫師 1998~迄今
高雄醫學大學 外科學 助理教授 2006/01~迄今
經歷:
美國維吉尼亞大學 神經外科 研究員2003/08~2005/07
高雄醫學大學附設醫院 外科 住院醫師1988/08~1994/07
高雄醫學大學附設醫院 神經外科 總醫師1994/08~1996/07
高雄醫學大學 外科學 講師2000/08~2005/12
31

16:10~16:30
Name: Cheng-Loong Liang 梁 正 隆Office Address: Department of Neurosurgery, E-DA Hospital, #1 E-DA Road, Yan-Chau Shiang,
Kaohsiung County, 824, TAIWAN. Tel No: 886-7-6150011
Education:
(2004 APR. ~ OCT.) Fellowship, Center for Imagine-Guided Neurosurgery, Department of
Neurosurgery, University of Pittsburgh Medical Center, Pennsylvania, USA
(1998~2002) Master of Medical Sciences, Institute of Clinical Medicine, Chang Gung
University, Taiwan
(1984~1991) Doctor of Medicine, Chung Shan Medical University, Taiwan
Academic Appointment:
Lecturer, I-Shou University
Employment Record:
(2004~ ) Director, Gamma Knife Center, E-DA Hospital, I-Shou University
(2004~ ) Attending Neurosurgeon, Department of Neurosurgery, E-DA Hospital, I-Shou University
(1999~2004) Attending Neurosurgeon, Department of Neurosurgery, Chang Gung Memorial Hospital,
Kaohsiung Medical Center
(1993~1999) Resident, Department of Surgery and Neurosurgery, Chang Gung Memorial Hospital,
Kaohsiung Medical Center
Board Certification: 1998, Board of Surgery (Taiwan)
Board Certification: 1999, Board of Neurosurgery (Taiwan)
Professional Affiliations:
American Association of Neurological Surgeon (AANS) USA
Surgical Association of R.O.C. (Taiwan)
Medical Association of R.O.C. (Taiwan)
Neurological Association of R.O.C. (Taiwan)
Taiwan Neurosurgical Society
Taiwan Stroke Society
Honor and awards:
2001 Award of Professor Lee T.K., Taiwan Stroke Society
2003 Award of Professor Du S.B., Taiwan Stroke Society
32

16:30~16:50
駱子文慈濟大學醫學系畢花蓮慈濟醫學中心 神經外科 總醫師花蓮慈濟醫學中心 神經外科 專科醫師(今年考取)
16:50~17:05
張軒凱陽明大學醫學系畢業台北榮總 神經外科 住院醫師
17:05~17:20
楊懷哲台北醫學大學醫學系畢業台北榮總 神經外科 總醫師台北榮總 神經外科 專科醫師(今年考取)
17:20~17:35
李政家陽明大學醫學系畢業台北榮總 神經外科 住院醫師
33











![KANSAI...KANSAI UNIVERSITY GUIDE BOOK 20 1 FOR INTERNATIONAL STUDENTS [博士課程前期課程][博士課程後期課程] 法学・政治学専攻 法学部法学研究科 [博士課程前期課程][博士課程後期課程]](https://static.fdocument.pub/doc/165x107/60cdd8ea248bf6336e1d8f0e/kansai-kansai-university-guide-book-20-1-for-international-students-ecoeececoeoeec.jpg)





