usodehipoglicemiantesembarazo
-
Upload
lostinthestars -
Category
Documents
-
view
216 -
download
0
Transcript of usodehipoglicemiantesembarazo
-
8/12/2019 usodehipoglicemiantesembarazo
1/10
Review Article
The use of oral hypoglycaemic agents in pregnancy
R. I. G. Holt and K. D. Lambert
Human Development and Health Academic Unit, Faculty of Medicine, University of Southampton, Southampton, UK
Accepted 29 November 2013
Abstract
While insulin has beenthe treatment of choice whenlifestylemeasuresdo not maintain glycaemiccontrol during pregnancy,
recent studies have suggested that certain oral hypoglycaemic agents may be safe and acceptable alternatives. With the
exception of metformin and glibenclamide (glyburide), there are insufficient data to recommend treatment with any other
oral hypoglycaemic agent during pregnancy. There are no serious safety concerns with metformin, despite it crossing the
placenta.Whenused in thefirst trimester, there is no increase in congenital abnormalities andthere appears to be a reduction
in miscarriage, pre-eclampsia and subsequent gestational diabetes. Studies of the use of metformin in gestational diabetes
show at least equivalent neonatal outcomes, while reporting reductions in neonatal hypoglycaemia, maternal
hypoglycaemia and weight gain and improved treatment satisfaction. Glibenclamide effectively lowers blood glucose in
women with gestational diabetes, possibly with a lower treatment failure rate than metformin. Although generally well
tolerated, some studies have reported higherrates of pre-eclampsia, neonatal jaundice, longerstay in theneonatal care unit,
macrosomia andneonatal hypoglycaemia.Thereis a paucity of long-termfollow-up data on children exposed to oral agents
in utero. The AmericanCollege of Obstetrics and Gynecology and the UK National Institute of Health and Care Excellence
(NICE) have recommended that either metformin or glibenclamide can be used to treat gestational diabetes. Metformin is
also recommended for use in the pre-conception period by NICE. By contrast, the American Diabetes Association
recommends that both drugs should only be used during pregnancy in the context of clinical trials.
Diabet. Med. 31, 282291 (2014)
IntroductionDiabetes is the commonest medical condition in pregnancy,
affecting 215% of pregnant women, depending on the
population and ethnic group studied [1,2]. Even with mild
hyperglycaemia, it is associated with increased rates of
miscarriage and congenital abnormalities in the first trimester
and abnormal fetal growth and development in the latter half
of pregnancy, characterized by macrosomia, which is in turn
associated with an increased risk of operative delivery,
shoulder dystocia and birth trauma. Offspring of mothers
with diabetes also experience increased rates of perinatal
hypoglycaemia, jaundice and respiratory distress and long
-term risk of diabetes and obesity.There is a linear relationship between maternal hyperglyca-
emia andadverse fetal outcomes [3]and twolargerandomized
controlled trials in women with gestational diabetes have
shown the benefit of treating mild maternal hyperglycaemia
[4,5]. The epidemiological data, coupled with these and other
trials, have led to recommendationsthat women with diabetes
should aim for normoglycaemia during pregnancy [1].
Traditionally, insulin is added if dietary and lifestyle
measures fail to maintain normoglycaemia [6]. However, thisapproach is demanding both for pregnant women and their
healthcare teams. Over the last decade, several studies have
challenged this strategy and suggested that the use of certain
oral hypoglycaemic agents may be safe and acceptable
alternatives to the use of insulin, at least for women with
gestational diabetes [7,8]. This review will examine the use of
oral agents in pregnancy, with a particular focus on
metformin and glibenclamide (glyburide).
Methods
PubMed, other electronic databases and relevant guidelines
were searched to identify articles that included the keywordspregnancy, diabetes and each individual oral hypoglycae-
mic agent name. The paper reference lists were searched
manually for further information. Oral hypoglycaemic agent
manufacturers were contacted for information and the
summaries of product characteristics consulted.
Metformin
Metformin is widely used to treat Type 2 diabetes and poly-
cystic ovary syndrome. It is an insulin sensitizer, inhibitingCorrespondence to: Richard I. G. Holt. E-mail: [email protected]
282 2013 The Authors.
Diabetic Medicine 2013 Diabetes UK
DIABETICMedicine
DOI: 10.1111/dme.12376
-
8/12/2019 usodehipoglicemiantesembarazo
2/10
gluconeogenesis and hepatic glucose output, while increasingmuscle glucose uptake. Metformin is excreted unchanged in
the urine. In pregnancy, as the glomerular filtration rate is
increased by 40%, there is potential for the drug to be
eliminated faster [9]. Metformin crosses the placenta, leading
to fetal concentrations that are at least half the maternal level
[7]. Metformin is not teratogenic in rats and rabbits at doses
of up to 600 mg kg1 day1, equivalent to 26 times the
maximum recommended human dose [7].
Human studies
Use in pre-conception period
Although metformin is not licensed for use during pregnancy,
increasing numbers of women have conceived (either acci-
dentally or purposefully) while taking metformin for Type 2
diabetes or polycystic ovary syndrome.
Retrospective studies. Retrospective cohort studies of the use
of metformin in the first trimester [10,11] and throughout
pregnancy [12,13] did not find major congenital malforma-
tions, although the total number of women studied was low.
Early pregnancy loss was reduced in one study (8.8 vs.
41.9%) [12] and neonatal hypoglycaemia was less common
in another (18.5 vs. 24.5%) [11]. One study showed amarginally reduced birthweight in neonates born to women
taking metformin [10], while another found no difference
[11].
The last retrospective study compared the use of metfor-
min with sulphonylureas and insulin in 105 women with
gestational diabetes and 55 women with Type 2 diabetes
[13]. There was a higher incidence of pre-eclampsia in
metformin-treated women [32% vs. 7% (sulphonylurea) vs.
10% (insulin), P < 0.001] and a higher incidence of perina-
tal mortality (11.6%) compared with women not treated
with metformin (1.3%, P < 0.02). The age and BMI of the
metformin-treated women (32 years, 31.2 kg/m2) were
significantly higher thanthe other groups (sulphonylurea group
28 years, 22.8 kg/m2, insulin group 29 years, 24.8 kg/m2),
making it unclear whether the differences reflect an indepen-
dent treatment effect, as obesity and increasing age are risk
factors for adverse pregnancy outcomes.
Prospective studies. Prospective cohort studies have also not
demonstrated significant adverse effects or congenital mal-
formations with metformin treatment and indeed have
shown some benefit [1420]. Most studies showed significant
reductions in miscarriage and fetal loss [14,15,19,20],
particularly when the women continued metformin through-
out pregnancy [16,17]. In one study, the spontaneous
abortion rate was reduced from 62% to 26% after the same
women began metformin treatment (P < 0.0001) [14].
A further important finding of these studies was an up to
tenfold reduction in incident gestational diabetes in metfor-
min-treated women [14
16,18,19]. The incidence ofpre-eclampsia was either unchanged [15,20] or reduced in
women taking metformin throughout pregnancy [16,18,19].
Birthweight and height of infants of metformin-treated
women was largely unchanged [14,20], but, in one study, the
incidence of intra-uterine growth restriction was lower in
women who continued treatment throughout pregnancy
compared with those who stopped metformin in the first
trimester (2.2 vs. 21.8%, P = 0.026) [16]. In another study
that followed the offspring for 18 months, there was no
evidence of motor or social developmental delays, although
male infants were thinner than the control group at 6 months
[15].
Randomized controlled trials. These observational studies led
onto a number of randomized controlled trials of the use of
metformin in early pregnancy [2124]. The first of these was
a pilot study that was subsequently extended into a larger
multi-centre study of 274 pregnant women with polycystic
ovary syndrome who were allocated to treatment with
metformin (n = 136) or placebo (n = 138) [21,22]. The pilot
study showed a reduction in adverse pregnancy outcomes,
but this was not replicated in the larger study. Furthermore,
there was no difference in the incidence of gestational
diabetes, pre-eclampsia or pre-term delivery in metfor-
min-treated women. The authors subsequently reported thepost-natal effects on offspring exposed to metformin during
pregnancy. Growth, body composition and metabolic mea-
surements were reported for 25 of the 37 children in the pilot
study when they were aged 79 years. There were no
differences in height, weight or body composition between
those exposed to metformin, but fasting glucose concentra-
tion was higher in the metformin group and there was also a
trend towards higher systolic blood pressure and lower LDL
cholesterol concentration [25]. In the larger study, at 1 year
after birth, infants in the metformin group were heavier than
Whats new?
Increasing numbers of women with polycystic ovary
syndrome or Type 2 diabetes are conceiving while
taking metformin.
Observational and experimental studies suggest that
metformin is safe throughout pregnancy and mayconvey specific benefits, including reduced pregnancy
loss, less maternal weight gain and less neonatal
hypoglycaemia.
Many women taking metformin for gestational diabetes
require supplementary insulin.
Glibenclamide is an effective alternative to insulin for
the treatment of gestational diabetes, but concerns
remain over its safety because of increased rates of
neonatal jaundice and hypoglycaemia.
2013 The Authors.Diabetic Medicine 2013 Diabetes UK 283
Review article DIABETICMedicine
-
8/12/2019 usodehipoglicemiantesembarazo
3/10
those in the placebo group (10.2 1.2 vs. 9.7 1.1 kg,
P = 0.003) [26].
There was a ninefold marked reduction in the incidence of
gestational diabetes in a further study of 29 women with
polycystic ovary syndrome who were randomized to con-
tinue metformin throughout the pregnancy compared with
30 who discontinued treatment during pregnancy (3.4 vs.
30%) [23].Thelast randomized study evaluatedthe effectof metformin
in 160 women with polycystic ovary syndrome and infertility
treated from conception to 12 weeks gestation [24].
Compared with the 160 women in the placebo group, the
metformin group experienced a higher pregnancy rate (53.6%
vs. 40.4%,P = 0.006) and live birth rate (41.9% vs. 28.8%,
P = 0.014).
Type 2 diabetes
At present there are no completed randomized controlled
trials of the use of metformin in women with Type 2 diabetes,butan ongoing trial of 500pregnantwomen recruitedfrom 25
centres in Canada will examine whether the addition of
metformin to standard treatment with insulin is beneficial
(Clinical Trials Registry No; NCT 01353391).
Gestational diabetes
Retrospective observational studies. The first study of
women with gestational diabetes included both metformin
and glibenclamide and as well as women with Type 2
diabetes. It reported that perinatal mortality was lower in
women treated with insulin compared with those in the oral
hypoglycaemic agent groups; however, this was explained by
differences in glycaemic control [27]. By contrast, the second
study found no significant differences in maternal outcomes
between the metformin and insulin groups [28]. Further-
more, there was no difference in mean birthweight, macros-
omia or gestational age at delivery. The incidence of neonatal
hypoglycaemia was higher in the offspring of insulin-treated
women (P = 0.03), but is probably explained by the higher
baseline glucose in insulin-treated women. The third retro-
spective study, which included 293 women treated with
metformin, found lower rates of macrosomia (8.2 vs. 14.3%,
odds ratio 0.56; 95% CI 0.330.99) and Caesarean delivery
and did not highlight any safety issues [29]. Fewer womentreated with metformin required insulin than women treated
with diet and lifestyle advice alone (21% vs. 37%, odds
ratio 0.46; 95% CI 0.320.66).
Prospective observational studies. In a study of 100 women
treated with metformin and 100 treated with insulin, there
was less maternal weight gain in the metformin group, while
neonates had less prematurity, neonatal jaundice and admis-
sion to the neonatal unit (P < 0.01) [30]. The benefits were
also seen in a study of 465 women treated with metformin,
either alone (n = 249) or with insulin (n = 216). These
women were compared with 371 women treated with diet
alone and 399 women treated with insulin alone [31].
Metformin-treated women had fewer pre-term births (19.2%
insulin, 12.5% metformin, 12.1% diet, P = 0.005) and
improved neonatal outcomes, including hypoglycaemia
requiring intravenous dextrose and neonatal intensive care
unit admission compared with women treated with insulin(11.1% insulin, 5.1% metformin, 7.4% diet,P = 0.004). No
difference in outcome was seen between the metformin and
diet group. Again, firm conclusions cannot be drawn because
of baseline differences between groups.
Randomized controlled trials. The largest and most influen-
tial study of the use of hypoglycaemic agents in pregnancy is
the Metformin in Gestational Diabetes (MiG), which eval-
uated the effectiveness and safety of metformin in the
treatment of gestational diabetes [32]. It recruited 751
women with gestational diabetes who were randomly allo-
cated to open-label treatment with metformin (1000
2000 mg daily) or to insulin alone. Strict glycaemic targets
were set and, if these were not met, women treated with
metformin were offered supplemental insulin. Of the 363
women in the metformin group, 168 (46.3%) required
insulin, but the median doses were lower than in women
treated with insulin alone (42 vs. 50 units). The women who
required supplemental insulin were more overweight, more
likely to have a past history of gestational diabetes and have
higher fasting glucose when they entered the trial. Consistent
with its use outside pregnancy, about 10% of women treated
with metformin developed gastrointestinal side effects, but
there were no serious adverse effects of metformin.
There was no significant difference in the primary out-
come, which was a composite of neonatal complications,
including hypoglycaemia, respiratory distress, phototherapy,
birth trauma, low APGAR and prematurity (metformin:
32.0%, insulin 32.2%). When the individual components of
the primary outcome were analysed, severe neonatal hypo-
glycaemia occurred more commonly in the insulin group (30/
370) than in the metformin group (12/363, P = 0.008). By
contrast, the number of preterm births was higher in the
metformin group (12.1% vs. 7.6%, P = 0.04); however, the
mean gestation was only 1.7 days shorter in the metformin
group. There was one perinatal death secondary to Budd
Chiari syndrome in the insulin-treated group. There were nodifferences in the number of congenital abnormalities
between groups.
The only significantly different secondary outcome mea-
sures were maternal weight gain (metformin 0.4 vs. insulin
2.0 kg, P = 0.001) and treatment satisfaction in favour of
metformin. Neonatal well-being and anthropometric mea-
surements were not different; however, 2-year-old children of
metformin-treated mothers had more subcutaneous upper
limb fat, but no difference in total body fat, implying a more
favourable pattern of fat distribution [33].
284 2013 The Authors.
Diabetic Medicine 2013 Diabetes UK
DIABETICMedicine Oral hypoglycaemic agents in pregnancy R. I. G. Holt and K. D. Lambert
-
8/12/2019 usodehipoglicemiantesembarazo
4/10
Seven more recent but smaller trials have largely confirmed
the safety and efficacy of metformin in gestational diabetes
compared with insulin [3439]. The first of these compared
50 women treated with metformin with 50 treated with
insulin [34]. There was no difference in neonatal outcomes,
but there was a non-significant doubling of Caesarean
delivery in metformin-treated women. Similarly, in another
trial of 160 women, of whom 80 were randomized tometformin treatment, there were no differences in obstetric
or neonatal outcomes, although maternal weight gain was
lower in women treated with metformin (11.3 vs. 13.7%,
P < 0.001) and the neonates were smaller (3.3 vs. 3.4 kg,
P = 0.005) [35]. Glycaemic control was similar with both
treatments. A further study of 47 women treated with
metformin found less maternal weight gain (P = 0.002) and
marginally improved maternal glycaemic control after dinner
compared with 47 women treated with insulin alone [36].
Hypoglycaemia was reduced in neonates in the metformin
group (P = 0.032).
Two further studies comparing the use of metformin withinsulin also found no difference in maternal and neonate
variables between groups, including Caesarean delivery,
birthweight, APGAR scores at 5 min, respiratory distress
syndrome, hyperbilirubinaemia, neonatal hypoglycaemia
and neonatal intensive care unit admission [37,39].
In the first of three trials comparing metformin with
glibenclamide, 75 women with gestational diabetes were
randomly assigned to treatment with metformin and 74 to
glibenclamide [38]. More women taking metformin were
switched to treatment with insulin (34.7 vs. 16.2%,
P = 0.01). In those women who achieved satisfactory
glycaemic control, there was no difference in fasting or
postprandial glucose between groups. There were more
Caesarean deliveries in the metformin group (15% vs. 3%,
P = 0.02), but no difference in pre-eclampsia. There was no
difference in neonatal hypoglycaemia or macrosomia rates,
but mean birthweight was 200 g greater in the glibenclamide
group (P = 0.02).
In the next trial, the main finding was that the 40
metformin-treated women experienced less weight gain than
the 32 treated with glibenclamide (10.3 vs. 7.6 kg, P = 0.02)
[40]. Similar numbers, 8% in the metformin group and 10%
in the glibenclamide group, required additional insulin
therapy. Although the numbers are small, there were no
differences in glycaemic control, birthweight, macrosomia orneonatal hypoglycaemia. A further report by the same group
described the use of metformin and glibenclamide in 104 and
96 women, respectively, again finding no differences in
adverse neonatal outcomes [41]. Birthweight was about
200 g lighter in the metformin group, while neonatal blood
glucose levels were significantly higher.
In most of the trials, a significant proportion of metfor-
min-treated womenup to 46.3%have required supple-
mental insulin. In general, these women had higher baseline
BMI, more marked hyperglycaemia and earlier diagnosis
and treatment of gestational diabetes, and tended to be
older.
Sulphonylureas
Sulphonylureas act by increasing insulin secretion from the
pancreaticb-cells. Glibenclamide clearance during pregnancy
is increased, leading to plasma concentrations that are about50% lower during pregnancy with equivalent doses [42].
Historical perspective
Early studies indicated that treatment with sulphonylureas
was associated with an increased incidence of congenital
abnormalities and neonatal hypoglycaemia, but this was
likely caused by maternal hyperglycaemia [27]. A more
recent systematic review and meta-analysis that examined
first-trimester exposure to oral hypoglycaemic agents, includ-
ing studies of chlorpropamide (n = 8), tolbutamide (n = 6)
and glibenclamide (n =
4), found no significant effect onmajor malformations after adjustment for maternal glycae-
mic control [43].
Nevertheless, the recognition that sulphonylureas readily
crossed the placenta and stimulated fetal insulin secretion
caused concern because many fetal complications of diabe-
tes, including macrosomia and neonatal hypoglycaemia, are
caused by fetal hyperinsulinaemia.
Preclinical studies
An interest in sulphonylureas was rekindled when it was
recognized that the degree to which sulphonylureas crossed
the placenta differed between individual drugs because of
differences in molecular weight, drug clearance and protein
binding [44]. These findings, and those of the subsequent
clinical trial [45] described below, have been contradicted by
a clinical study of 40 women with gestational diabetes and
40 healthy pregnant women, which found that glibenclamide
crossed the human placenta, leading to fetal plasma concen-
trations that are ~70% of maternal plasma levels [42].
Langer randomized controlled trial
Unlike metformin, where the major clinical trial was
preceded by several observational studies, the use of gliben-clamide was largely stimulated by the publication of a
randomized clinical trial by Langer and colleagues in 2000
[45]. Four hundred and four women with gestational
diabetes, defined by the Carpenter and Coustan criteria,
were randomly assigned to receive insulin or glibenclamide.
The starting dose of glibenclamide was 2.5 mg daily and was
increased by 5 mg per week to a maximum of 20 mg daily if
necessary. The primary outcome variable was achievement of
adequate glycaemic control, defined as a mean blood glucose
of 5.05.9 mmol/l, a fasting blood glucose of 3.45.0 mmol/l,
2013 The Authors.Diabetic Medicine 2013 Diabetes UK 285
Review article DIABETICMedicine
-
8/12/2019 usodehipoglicemiantesembarazo
5/10
-
8/12/2019 usodehipoglicemiantesembarazo
6/10
age and parity [56]. It is interesting to note that, generally,
neonatal outcomes appear no worse in women who switched
to insulin [52,56], although, in one study, neonates were
more likely to require intravenous glucose to treat hypo-
glycaemia [54].
Randomized controlled trialsIn a Brazilian study, 27 women treated with insulin were
compared with 24 treated with glibenclamide and 19 treated
with acarbose [57]. Adequate glycaemic control was
achieved in 79% of the glibenclamide-treated women and
58% of women using acarbose. Large for gestational age
occurred in 3.7%, 25% and 10.5% of the neonates born to
mothers treated with insulin, glibenclamide and acarbose,
respectively. Six of the eight cases of neonatal hypoglycaemia
occurred in glibenclamide-treated women.
In a second smaller study from India, no differences in
glycaemia or birthweight were observed in 10 women treated
with glibenclamide and 13 treated with insulin [58].Following treatment commencement, there was no difference
in glycaemic measures or fetal outcomes. No hypoglycaemic
episodes were reported in either group.
In a further trial of 48 women with gestational diabetes
treated with glibenclamide and 49 treated with insulin, there
was no difference in maternal hypoglycaemia or Caesarean
delivery, but 28% of infants in the glibenclamide group were
more likely to experience an episode of hypoglycaemia (28
vs. 13%, P < 0.03) [59].
A randomized controlled trial examined neonatal body
composition in 82 infants born to 50 women treated with
insulin and 49 treated with glibenclamide [60]. Maternal
glycaemic control was similar between the groups, except after
dinner when glucose concentrations were lower in insu-
lin-treated women. There was no difference in neonatal fat
mass, BMI or ponderal index between groups. However,
macrosomia occurred more frequently in the glibenclamide
group (22% vs. 2.4%,P = 0.01). Furthermore, the glibencla-
mide group experienced a 4.9% increase in the rate of
intrauterine growth retardation (P < 0.01). There was no
difference in umbilical cord insulin and glucose concentration.
Thiazolidinediones
Thiazolidinediones are insulin sensitizers that activate thenuclear peroxisome proliferator activator receptor gamma
(PPARc), that in turn increases transcription of genes
regulating adipogenesis, glucose and lipid metabolism.
Several studies have shown that, similar to metformin,
thiazolidinediones improve insulin resistance and hyperan-
drogenism and are being used to treat polycystic ovary
syndrome [61].
PPARc plays a role in placental maturation and may
regulate placental fatty acid transport and storage and
hormone secretion [62]. Although thiazolinediones do not
appear to be teratogenic, they readily cross the placenta and
their use has been associated with fetal death and growth
retardation, secondary to placental dysfunction. There are
only limited data in human pregnancy [63 65] and so the use
of thiazolinediones is not recommended.
Alpha-glucosidase inhibitors
Alpha-glucosidase inhibitors reduce intestinal carbohydrate
absorption by inhibiting the cleavage of disaccharides and
oligosaccharides to monosaccharides in the small intestine.
As they reduce postprandial hyperglycaemia and less than
2% is absorbed (although drug metabolites may appear in
the maternal circulation), these agents may have potential
benefits in pregnancy. Animal studies have suggested no
harmful effects, but there are scanty data of its use in human
pregnancy [62]. There are theoretical concerns that the
reduced carbohydrate absorption may alter bowel flora and
alter inflammation or prostaglandin E secretion, with thepotential to induce labour.
Apart from the Brazilian study described above [57], two
other reports describe experience in 11 women [66,67]; in
one report, six women with gestational diabetes were
successfully treated [66], but the other reported that two of
the five women, who took acarbose early in pregnancy,
miscarried [67].
Although further studies are warranted, at present the use
of a-glucosidase inhibitors is not currently recommended
because of the lack of human pregnancy safety data.
Incretin-based treatmentsAt present, scant information exists for the use of incre-
tin-based therapies during pregnancy, but the available data
from animal studies suggest that these drugs should be
avoided. Although dideptidyl peptidase 4 (DPP-4) inhibitors
and glucagon-like peptide 1 (GLP-1) receptor agonists do
not appear teratogenic, there have been reports of growth
retardation and delayed ossification and other skeletal effects
in rats and rabbits.
SGLT-2 inhibitors
There are no human studies of the use of sodium-glucoseco-transporter 2 (SGLT-2) inhibitors in pregnancy, but
studies in rats have shown toxicity to the developing
kidney with an increased incidence and/or severity of renal
pelvic and tubular dilatations in the time period corre-
sponding to the second and third trimesters of human
pregnancy. At higher doses, the use of dapagliflozin was
associated with reductions in birthweight. As such, treat-
ment with SGLT-2 inhibitors during pregnancy is not
recommended.
2013 The Authors.Diabetic Medicine 2013 Diabetes UK 287
Review article DIABETICMedicine
-
8/12/2019 usodehipoglicemiantesembarazo
7/10
Recommendations
The US Food and Drug Administration (FDA) has classified
metformin and acarbose as category B drugs (does not
increase the risk of harm to the fetus) as animal studies have
failed to demonstrate a risk in pregnancy, but there are no
adequate well-controlled studies in pregnant women, while
all other oral hypoglycaemic agents are category C [eitherstudies in animals have revealed adverse effects on the fetus
(teratogenic or embryocidal or other) and there are no
controlled studies in women or studies in women and
animals are not available].
The American Diabetes Association (ADA) has cautioned
against the use of glibenclamide and metformin in preg-
nancy, but infers that, if a woman becomes pregnant while
taking either agent, she should continue this until insulin can
be initiated because of the known risk of hyperglycaemia
[68]. The guidelines currently recommend that both drugs
should only be used during pregnancy in the context of
controlled clinical trials. By contrast, the American Collegeof Obstetrics and Gynecology has recommended that either
drug may be considered to control hyperglycaemia in women
with gestational diabetes [6].
While acknowledging that there is no marketing authori-
zation specifically for pregnancy, the UK National Institute
of Health and Care Excellence (NICE) has recommended
that either metformin or glibenclamide can be used to treat
women with gestational diabetes. Metformin may also be
used in the pre-conception period and during pregnancy as
an adjunct or alternative to insulin, when the likely benefits
from improved glycaemic control outweigh the potential for
harm [1]. No other drugs are recommended.
Discussion
The aim of diabetes management in pregnancy is to achieve
normoglycaemia and meeting this goal is more importantthan the means by which it is achieved. However, with the
exception of metformin and glibenclamide, there are insuf-
ficient data to recommend treatment with any other currently
available oral hypoglycaemic agent during pregnancy. There
are also insufficient data about the use of glibenclamide
during the first trimester to recommend its use in women
with pre-existing Type 2 diabetes.
None of the studies of metformin in pregnancy have
highlighted any serious safety concerns, despite it crossing
the placenta. When used to treat women with polycystic
ovary syndrome, there is no increase in congenital abnor-
malities and there appears to be a reduction in miscarriageand pre-eclampsia. Most studies also suggest a reduction in
the later onset of gestational diabetes. While we await the
results of the use of metformin in women with Type 2
diabetes in pregnancy, these results should be reassuring to
women who conceive while taking metformin, and it seems
reasonable to continue metformin if a woman becomes
pregnant while taking the drug as it is likely that any
potential harm is outweighed by the risk of worsening
glycaemic control.
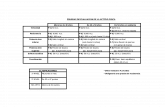
Table 1 Comparison of metformin and glibenclamide in pregnancy
Metformin Glibenclamide
Data available Observational and randomized controlled trial studiesin pre-conception period and during pregnancy
Observational and randomized controlledtrial studies during pregnancy
Maternal outcomesGlucose control Failure rate: up to 46% will require supplemental insulin
Less hypoglycaemia than insulinLess gestational diabetes in women treated throughout
pregnancy
Failure rate: 1621% will requiresupplemental insulin
Less hypoglycaemia than insulin
Pre-eclampsia Possibly reduced Possibly increasedWeight gain Less than insulin Similar to insulinTreatment satisfaction Better than insulin No data
Neonatal outcomesEarly pregnancy loss Possibly reduced No dataHypoglycaemia Less than insulin No difference from insulin
Timing of birth Discrepant findings but overall no effect No difference from insulinBirthweight No difference or marginally reducedNo difference or less intra-uterine growth restriction
No difference or lower rate of macrosomia
No differencePossible increase in intra-uterine growth
restrictionPossible increase in macrosomia
Jaundice No change Possibly increasedNeonatal unit admission Reduced Possibly longer stay
Long-term follow-up of infantsMotor or social development No evidence of delay No dataGrowth Thinner at 6 months
Heavier at 1 yearPossibly altered fat distribution at 2 yearsNo difference at 8 years
No data
288 2013 The Authors.
Diabetic Medicine 2013 Diabetes UK
DIABETICMedicine Oral hypoglycaemic agents in pregnancy R. I. G. Holt and K. D. Lambert
-
8/12/2019 usodehipoglicemiantesembarazo
8/10
While many of the studies of the use of metformin in
gestational diabetes are limited by small numbers, they are
similarly encouraging, showing at least equivalent neonatal
outcomes for metformin compared with insulin, while
reporting reductions in maternal hypoglycaemia and weight
gain and improved treatment satisfaction. Neonatal hypo-
glycaemia also appears reduced. There are discrepant find-
ings regarding the timing of birth, but these differences maybe influenced by other factors apart from treatment. These
studies provide evidence that metformin is an effective and
safe alternative to the use of insulin.
At present there are few reports of the long-term effects of
metformin on offspring exposed to the drug in utero. There
may be early differences in growth patterns and one small
study has observed increased glucose concentrations. Larger
long-term follow-up of these children is needed.
Several experimental and observational studies have dem-
onstrated that glibenclamide can effectively lower blood
glucose in women with gestational diabetes, possibly with a
lower treatment failure rate than metformin. Glibenclamideis generally well tolerated with few experiencing significant
side effects [50,53]. While many studies have not shown
differences in fetal and maternal outcomes between gliben-
clamide and insulin, they are limited in their power to
demonstrate differences. One commentary suggested that,
had the number of participants been doubled in the Langer
trial with similar results, the observed differences in glycae-
mic control between groups may have been significant [49].
By contrast, other studies have reported higher rates of
pre-eclampsia, neonatal jaundice requiring phototherapy,
longer stay in the neonatal care unit, macrosomia and
neonatal hypoglycaemia in women who were treated with
glibenclamide. There are no reports of the long-term effects
of glibenclamide on offspring exposed to the drug in utero.
When making a choice between metformin and glibencla-
mide, the benefits of less maternal weight gain, lower
birthweight and treatment satisfaction favour the use of
metformin over glibenclamide (Table 1). Although a greater
proportion appears to require supplementary insulin, the
addition of insulin to metformin is more straightforward
than the switch from glibenclamide. Although both metfor-
min and glibenclamide appear safe, there are some residual
concerns about glibenclamide that need to be resolved before
this drug can be recommended unreservedly. Furthermore,
the very premise that glibenclamide does not cross theplacenta [45] has been challenged [42]. It is unclear why
there have been discrepant results, but, if indeed glibencla-
mide does cross the placenta in significant quantities, the
potential to stimulate fetal insulin production is of concern.
With both drugs, many women do not achieve adequate
glycaemic control and require insulin. It is important to
minimize the time of hyperglycaemia and so doses should be
rapidly escalated to the maximally tolerated doses, while
being mindful of the risk of side effects. Consideration should
therefore be given to starting insulin concurrently with
metformin in women with high BMI, prior history of
gestational diabetes and high baseline glucose who have a
high chance of missing their glycaemic targets with metfor-
min alone.
In conclusion, recent studies have suggested that metfor-
min and glibenclamide agents may be safe and acceptable
alternatives to insulin in the treatment of gestational diabe-
tes, with the evidence favouring the use of metformin.
Funding sources
This review was funded by the University of Southampton.
Competing interests
RIGH was a member of the National Institute for Health and
Clinical Excellence (NICE) diabetes and pregnancy guideline
development group.
References
1 National Collaborating Centre for Womens and Childrens Health.
Diabetes in Pregnancy: Management of Diabetes and its Compli-
cations from Preconception to the Postnatal Period. London:
RCOG Press, 2008.
2 Confidential Enquiry into Maternal and Child Health.Pregnancy in
Women with Type 1 and Type 2 Diabetes in 20022003, England,
Wales and Northern Ireland. London: CEMACH, 2005.
3 Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U,
Coustan DRet al. Hyperglycemia and adverse pregnancy outcomes.
N Engl J Med2008; 358: 19912002.
4 Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS,
Robinson JS. Effect of treatment of gestational diabetes mellitus
on pregnancy outcomes. N Engl J Med2005;352
: 2477
2486.5 Landon MB, Spong CY, Thom E, Carpenter MW, Ramin SM,
Casey Bet al. A multicenter, randomized trial of treatment for mild
gestational diabetes. N Engl J Med2009; 361: 13391348.
6 Committee on Practice Bulletins Obstetrics, The American College
of Obstetricians and Gynecologists. Practice bulletin no. 137:
gestational diabetes mellitus.Obstet Gynecol2013; 122: 406416.
7 Lautatzis ME, Goulis DG, Vrontakis M. Efficacy and safety of
metformin during pregnancy in women with gestational diabetes
mellitus or polycystic ovary syndrome: a systematic review.
Metabolism2013; 62: 15221534.
8 Nicholson W, Baptiste-Roberts K. Oral hypoglycaemic agents
during pregnancy: the evidence for effectiveness and safety. Best
Pract Res Clin Obstet Gynaecol2011; 25: 5163.
9 Hughes RC, Gardiner SJ, Begg EJ, Zhang M. Effect of pregnancy
on the pharmacokinetics of metformin. Diabet Med 2006; 23:323326.
10 Kovo M, Weissman A, Gur D, Levran D, Rotmensch S, Glezerman
M. Neonatal outcome in polycystic ovarian syndrome patients
treated with metformin during pregnancy.J Matern Fetal Neonatal
Med2006; 19: 415419.
11 Bolton S, Cleary B, Walsh J, Dempsey E, Turner MJ. Continuation
of metformin in the first trimester of women with polycystic
ovarian syndrome is not associated with increased perinatal
morbidity.Eur J Pediatr 2009; 168: 203206.
12 Jakubowicz DJ, Iuorno MJ, Jakubowicz S, Roberts KA, Nestler JE.
Effects of metformin on early pregnancy loss in the polycystic ovary
syndrome. J Clin Endocrinol Metab2002; 87: 524529.
2013 The Authors.Diabetic Medicine 2013 Diabetes UK 289
Review article DIABETICMedicine
-
8/12/2019 usodehipoglicemiantesembarazo
9/10
13 Hellmuth E, Damm P, Molsted-Pedersen L. Oral hypoglycaemic
agents in 118 diabetic pregnancies.Diabet Med2000;17: 507511.
14 Glueck CJ, Wang P, Goldenberg N, Sieve-Smith L. Pregnancy
outcomes among women with polycystic ovary syndrome treated
with metformin. Hum Reprod2002; 17: 28582864.
15 Glueck CJ, Goldenberg N, Pranikoff J, Loftspring M, Sieve L,
Wang P. Height, weight, and motor-social development during the
first 18 months of life in 126 infants born to 109 mothers with
polycystic ovary syndrome who conceived on and continuedmetformin through pregnancy.Hum Reprod2004; 19: 13231330.
16 Nawaz FH, Khalid R, Naru T, Rizvi J. Does continuous use of
metformin throughout pregnancy improve pregnancy outcomes in
women with polycystic ovarian syndrome?J Obstet Gynaecol Res
2008; 34: 832837.
17 Khattab S, MohsenIA, Foutouh IA, Ramadan A,Moaz M, Al-Inany
H. Metformin reduces abortion in pregnant women with polycystic
ovary syndrome.Gynecol Endocrinol2006; 22: 680684.
18 Khattab S, Mohsen IA, Aboul F, I, Ashmawi HS, Mohsen MN, van
Wely M et al. Can metformin reduce the incidence of gestational
diabetes mellitus in pregnant women with polycystic ovary
syndrome? Prospective cohort study. Gynecol Endocrinol 2011;
27: 789793.
19 De Leo V, Musacchio MC, Piomboni P, Di Sabatino A, Morgante
G. The administration of metformin during pregnancy reducespolycystic ovary syndrome related gestational complications. Eur
J Obstet Gynecol Reprod Biol2011; 157: 6366.
20 Glueck CJ, Goldenberg N, Pranikoff J, Khan Z, Padda J, Wang P.
Effects of metformin-diet intervention before and throughout
pregnancy on obstetric and neonatal outcomes in patients with
polycystic ovary syndrome. Curr Med Res Opin 2013; 29: 5562.
21 Vanky E, Salvesen KA, Heimstad R, Fougner KJ, Romundstad P,
Carlsen SM. Metformin reduces pregnancy complications without
affecting androgen levels in pregnant polycystic ovary syndrome
women: results of a randomized study. Hum Reprod 2004; 19:
17341740.
22 Vanky E, Stridsklev S, Heimstad R, Romundstad P, Skogoy K,
Kleggetveit Oet al. Metformin versus placebo from first trimester to
delivery in polycystic ovary syndrome: a randomized, controlled
multicenter study.J Clin Endocrinol Metab 2010;95: E448
E455.23 Begum MR, Khanam NN, Quadir E, Ferdous J, Begum MS, Khan F
et al. Prevention of gestational diabetes mellitus by continuing
metformin therapy throughout pregnancy in women with polycys-
tic ovary syndrome. J Obstet Gynaecol Res 2009; 35: 282286.
24 Morin-Papunen L, Rantala AS, Unkila-Kallio L, Tiitinen A,
Hippelainen M, Perheentupa A et al. Metformin improves preg-
nancy and live-birth rates in women with polycystic ovary
syndrome (PCOS): a multicenter, double-blind, placebo-controlled
randomized trial. J Clin Endocrinol Metab2012; 97: 14921500.
25 Ro TB, Ludvigsen HV, Carlsen SM, Vanky E. Growth, body
composition and metabolic profile of 8-year-old children exposed
to metformin in utero.Scand J Clin Lab Invest2012; 72: 570575.
26 Carlsen SM, Martinussen MP, Vanky E. Metformins effect on
first-year weight gain: a follow-up study. Pediatrics 2012; 130:
e1222e1226.27 Ekpebegh CO, Coetzee EJ, van der Merwe L, Levitt NS. A 10-year
retrospective analysis of pregnancy outcome in pregestational
Type 2 diabetes: comparison of insulin and oral glucose-lowering
agents.Diabet Med2007; 24: 253258.
28 Tertti K, Ekblad U, Vahlberg T, Ronnemaa T. Comparison of
metformin and insulin in the treatment of gestational diabetes: a
retrospective, case-control study.Rev Diabet Stud2008; 5: 95101.
29 Gandhi P, Bustani R, Madhuvrata P, Farrell T. Introduction of
metformin for gestational diabetes mellitus in clinical practice: has
it had an impact? Eur J Obstet Gynecol Reprod Biol2012; 160:
147150.
30 Balani J, Hyer SL, Rodin DA, Shehata H. Pregnancy outcomes in
women with gestational diabetes treated with metformin or insulin:
a casecontrol study. Diabet Med2009; 26: 798802.
31 Goh JE, Sadler L, Rowan J. Metformin for gestational diabetes in
routine clinical practice. Diabet Med2011; 28: 10821087.
32 Rowan JA, Hague WM, Gao W, Battin MR, Moore MP.
Metformin versus insulin for the treatment of gestational diabetes.
N Engl J Med2008; 358: 20032015.
33 Rowan JA, Rush EC, Obolonkin V, Battin M, Wouldes T, HagueWM. Metformin in gestational diabetes: the offspring follow-up
(MiG TOFU): body composition at 2 years of age. Diabetes Care
2011; 34: 22792284.
34 Ijas H, Vaarasmaki M, Morin-Papunen L, Keravuo R, Ebeling T,
Saarela Tet al. Metformin should be considered in the treatment of
gestational diabetes: a prospective randomised study.BJOG2011;
118: 880885.
35 Niromanesh S, Alavi A, Sharbaf FR, Amjadi N, Moosavi S, Akbari
S. Metformin compared with insulin in the management of
gestational diabetes mellitus: a randomized clinical trial. Diabetes
Res Clin Pract2012; 98: 422429.
36 Spaulonci CP, Bernardes LS, Trindade TC, Zugaib M, Francisco
RP. Randomized trial of metformin vs insulin in the management of
gestational diabetes. Am J Obstet Gynecol2013; 209: 34.
37 Moore LE, Briery CM, Clokey D, Martin RW, Williford NJ, BofillJA,et al. Metformin and insulin in the management of gestational
diabetes mellitus: preliminary results of a comparison. J Reprod
Med2007; 52: 10111015.
38 Moore LE, Clokey D, Rappaport VJ, Curet LB. Metformin
compared with glyburide in gestational diabetes: a randomized
controlled trial.Obstet Gynecol2010; 115: 5559.
39 Tertti K, Ekblad U, Koskinen P, Vahlberg T, Ronnemaa T.
Metformin vs. insulin in gestational diabetes. A randomized study
characterizing metformin patients needing additional insulin. Dia-
betes Obes Metab 2013; 15: 246251.
40 Silva JC, Pacheco C, Bizato J, de Souza BV, Ribeiro TE, Bertini
AM. Metformin compared with glyburide for the management of
gestational diabetes. Int J Gynaecol Obstet2010; 111: 3740.
41 Silva JC, Fachin DR, Coral ML, Bertini AM. Perinatal impact of
the use of metformin and glyburide for the treatment of gestationaldiabetes mellitus. J Perinat Med2012; 40: 225228.
42 Hebert MF, Ma X, Naraharisetti SB, Krudys KM, Umans JG,
Hankins GDet al. Are we optimizing gestational diabetes treatment
with glyburide? The pharmacologic basis for better clinical
practice.Clin Pharmacol Ther 2009; 85: 607614.
43 Gutzin SJ, Kozer E, Magee LA, Feig DS, Koren G. The safety of
oral hypoglycemic agents in the first trimester of pregnancy: a
meta-analysis.Can J Clin Pharmacol2003; 10: 179183.
44 Elliott BD, Schenker S, Langer O, Johnson R, Prihoda T.
Comparative placental transport of oral hypoglycemic agents in
humans: a model of human placental drug transfer. Am J Obstet
Gynecol1994; 171: 653660.
45 Langer O, Conway DL, Berkus MD, Xenakis EM, Gonzales O. A
comparison of glyburide and insulin in women with gestational
diabetes mellitus. N Engl J Med2000; 343: 11341138.46 Langer O, Yogev Y, Xenakis EM, Rosenn B. Insulin and glyburide
therapy: dosage, severity level of gestational diabetes, and preg-
nancy outcome. Am J Obstet Gynecol2005; 192: 134139.
47 Jacobson GF, Ramos GA, Ching JY, Kirby RS, Ferrara A, Field DR.
Comparison of glyburide and insulin for the management of
gestational diabetes in a large managed care organization. Am
J Obstet Gynecol2005; 193: 118124.
48 Ramos GA, Jacobson GF, Kirby RS, Ching JY, Field DR.
Comparison of glyburide and insulin for the management of
gestational diabetics with markedly elevated oral glucose challenge
test and fasting hyperglycemia. J Perinatol2007; 27: 262267.
290 2013 The Authors.
Diabetic Medicine 2013 Diabetes UK
DIABETICMedicine Oral hypoglycaemic agents in pregnancy R. I. G. Holt and K. D. Lambert
-
8/12/2019 usodehipoglicemiantesembarazo
10/10