The role of angiostatins in diabetic complications
Transcript of The role of angiostatins in diabetic complications

ISSN 1990�7508, Biochemistry (Moscow) Supplement Series B: Biomedical Chemistry, 2014, Vol. 8, No. 2, pp. 94–107. © Pleiades Publishing, Ltd., 2014.Original Russian Text © A.A. Tykhomyrov, S.I. Shram, T.V. Grinenko, 2014, published in Biomeditsinskaya Khimiya.
94
1 INTRODUCTION
Angiogenesis is a process of formation of new bloodvessels from pre�existing ones. In a normally function�ing adult organism the intensity of blood vessel forma�tion is minimal. Activation of this process is observedonly during endometrial proliferation, maturation ofthe follicle, corpus luteum and placenta, as well as inwound healing, regeneration of damaged tissues andischemia�stimulated formation of collateral vessels.Angiogenesis is strictly controlled by a large number ofpro�angiogenic (VEGF, PDGF, bFGF, EGF, MMP,fibrinogen, fibronectin, etc.) and anti�angiogenic(AS, ES, TSP�1, PF4, PEDF, TGF�β1, PAI�1, α2�AP,TIMP, etc.) factors [1−3]. Impairments of the angio�
1 To whom correspondence should be addressed. Abbreviations used: rAAV—recombinant adeno�associated vec�tor; AGE—advanced glycation end products, α2�AP—α2�anti�plasmin, AS—angiostatins; BRB—blood retinal barrier,CVD—cardiovascular diseases, DM—diabetes mellitus, DN—diabetic nephropathy, DR—diabetic retinopathy, EGF—epi�dermal growth factor, ES—endostatins, bFGF—basic fibro�blast growth factor, HGF—hepatocyte growth factor, HIF�1α�hypoxia�induced factor, ICAM�1—intercellular adhesion mol�ecule 1; IL�1β—interleukin�1β, K—kringle, MCP�1—mono�cyte chemotactic protein 1; MMP—matrix metalloproteinases;eNOS—endothelial nitric oxide synthase, PAI�1—plasmino�gen activator inhibitor 1; t�PA—tissue plasminogen activator;u�PA—urokinase type plasminogen activator; PDGF—plateletderived growth factor; PEDF—pigment epithelium�derivedfactor, PF4—platelet factor 4; Pg—plasminogen, PKC—pro�tein kinase C, Pm—plasmin, ROS—reactive oxygen species;STZ—streptozotocin, TNF�α—transforming growth factor α,TNF�β1�transforming growth factor β1, TIMP—tissue inhibi�tors of metalloproteinases, TSP 1—thrombospondin 1;VEGF—vascular endothelium growth factor.
genic balance promote the development of variouspathologies. The mechanisms of pathological angio�genesis have been most comprehensively studied insuch processes as tumorigenesis and metastasis [4, 5],atherosclerosis [6], peptic ulcer [7], and in someautoimmune diseases [8, 9]. Vascular disorders associ�ated with diabetes mellitus (DM) are known to be themain causes of various diabetic complications: neur�opathy, retinopathy, nephropathy, cardiovascularpathologies [10]. Hyperglycemia accompanied by thedamage and dysfunction of endotheliocytes and acti�vation of inflammatory processes is also combinedwith impaired functioning of the hemostatic systemand the imbalance of the regulatory system that con�trols angiogenesis [11]. Currently performed studieson pathogenic mechanisms of endothelial dysfunctionin diabetes are extremely important for the develop�ment of new approaches for the treatment and correc�tion of vascular disorders [12].
During two last decades special attention ofresearches was paid to angiostatins (AS), the pro�teolytic fragments of plasminogen (Pg), which areconsidered as the most powerful endogenous angio�genesis inhibitors. The first studies of their physiolog�ical effects demonstrated that AS produced by varioustypes of tumor cells via limited proteolysis and Pg werethe factors limiting progression of the primary tumorand suppressing its metastasis [13, 14]. It has beenfound that the static effect of AS on the tumor is basedon their ability to inhibit proliferation of endothelialcells [15]. Now, there is evidence that indirect effectsof AS are realized through their regulation of synthesis
The Role of Angiostatins in Diabetic ComplicationsA. A. Tykhomyrova, S. I. Shramb, 1, and T. V. Grinenkoa
aPalladin Institute of Biochemistry of the National Academy of Sciences of Ukraine, Kyiv, UkrainebInstitute of Molecular Genetics, Russian Academy of Sciences,
pl. Kurchatova 2, Moscow, 123182 Russiatel.: +7 (499)196�02�13; e�mail: [email protected]
Received September 4, 2013
Abstract–Angiogenesis, a process of formation of new blood vessels form pre�existing vessels, is regulated bya large number of peptide factors. Imbalance of pro� and anti�angiogenic factors appears to be the majorcause of vascular abnormalities leading to various complications in diabetes mellitus. Angiostatins, kringle�containing fragments of plasminogen/plasmin, are among of the most potent physiological inhibitors ofneovascularization. In this review we focus on the colligation and analysis of the available data on peculiaritiesof production of angiostatins and their functioning in diabetes mellitus conditions. Special attention is paidto the role of angiostatins in the pathogenesis of typical diabetic complications, including retinopathies,nephropathies, and cardiovascular diseases.
Keywords: angiostatins, kringle domains, plasminogen, diabetes mellitus, vascular abnormalities
DOI: 10.1134/S1990750814020140

BIOCHEMISTRY (MOSCOW) SUPPLEMENT SERIES B: BIOMEDICAL CHEMISTRY Vol. 8 No. 2 2014
ANGIOSTATINS IN DIABETES 95
of growth factors and cytokines [16, 17]. Results ofnumerous studies indicate that the physiological func�tions of AS are broader than previously believed [18,19]. Various cells normally producing AS were identi�fied and changes in their levels not only in cancer, butalso in other diseases were reported [20–22]. It is espe�cially interesting that impairments in the activator–inhibitor balance of proteases involved in the AS for�mation from Pg can play a leading role in the etiologyof a number of diabetic complications [23]. For exam�ple, insufficient local AS production that accompanieshyperglycemia causes activation of retinal microvas�cular growth, and which, in turn, leads to to progres�sion of retinopathy [24]. In contrast, intense AS gen�eration in the myocardial tissue, aorta and coronaryartery walls prevents the formation of vascular collat�erals and is considered as the most important etiolog�ical link in the development of coronary heart diseaseand myocardial infarction risk in diabetic patients[25]. AS deficiency in the kidney in the early stages ofdiabetic nephropathy and their abnormally high con�tent in the end�stage of this disease, in combinationwith the imbalance of other regulators of angiogenesisis one of the causes of severe functional abnormalitiesin the kidneys [26, 27]. However, information regard�ing molecular mechanisms underlying AS involve�ment in the pathogenesis of vascular abnormalities inDM is rather fragmentary and often contradictory.Meanwhile, clear understanding of the general princi�ples and specific mechanisms involving AS in thedevelopment of endothelial dysfunction and inflam�matory reactions accompanying diabetes is veryimportant for the development of methods of diagno�sis and therapy of various diabetic complications.
In this review we have attempted to systematize andanalyze currently available literature data on the fea�tures of AS formation in various organs and tissues inDM, their involvement in molecular mechanisms ofthe development of diabetic complications such as ret�inopathy, nephropathy and cardiovascular disease,and the prospects of AS use as principally new agentsfor the prophylaxis and treatment of certain diabeticcomplications.
1. ANGIOSTATINS ARE PRODUCTSOF LIMITED PROTEOLYSIS
OF PLASMINOGEN
Pg is a proenzyme of plasmin (Pm; EC 3.4.21.7),the key protease of the fibrinolytic system. Availabledata clearly indicate that the physiological role ofPg/Pm is not limited to their fibrinolytic activity. Pgbinding to receptor proteins and its subsequent con�version into Pm on the cell surface provide theinvolvement of these proteins in the regulation ofmany cellular processes, both in normal and in patho�logical conditions (tissue remodeling, angiogenesis,inflammation, carcinogenesis, etc.) [28–30]. Pg wasfound in various human organs and tissues, but its
highest concentration was detected in the plasma(about 0.2 μM) [31]. Pg is most intensively synthesizedby hepatocytes, but its mRNA has been also detectedin other tissues [32]. The native form of Pg (Glu�Pg) isa single chain glycoprotein with a molecular mass(Mm) of 92 kDa; it consists of 791 amino acid residues(Glu1�Asp791) and contains up to 2% of carbohy�drates. The Pg molecule consists of seven domainsincluding the N�terminal peptide (NTP), five kringledomains (K1�K5) and the C�terminal serine protein�ase domain (SP) [33, 34]. Pg conversion into Pminvolves cleavage of the peptide bond Arg561�Val562by tissue plasminogen activator (t�PA) or urokinase�type Pg activator (u�PA) [35]. This is accompanied byactive site formation in the Pm molecule, in whichHis603, Asp646, and Ser741 play the key role [36].Intramolecular interactions between NTP and C5promote maintenance of a compact closed conforma�tion of Pg [37]. Hydrolysis of the Pm peptide bondLys77�Lys78 leads to NTP cleavage and formation ofLys�Pg (Lys78�Asn791), which has an extendedopened conformation and is more easily activated toPm than Glu�Pg [38].
Kringle domains are characterized by a relativelyhigh homology. Each kringle domain consists of about80 residues and is stabilized by three disulfide bonds.The kringle domains contain specific binding sites forω�aminocarboxylic acids (lysine, 6�aminohexanoicacid, etc.) known as lysine�binding sites [39]. Finestructural differences and ligand specificity of thesesites have been elucidated for each of the five kringledomains [40]. The kringle domains are involved inPg/Pm interactions with various plasma proteins(fibrinogen, fibrin, antiplasmin (α2�AP), histidine�rich glycoprotein, tetranectin, thrombospondin), pro�teins of plasma membrane of endotheliocytes andblood cells except for red blood cells, and also withextracellular matrix proteins (fibronectin, laminin)[41−44]. They play an important role in the mecha�nisms regulating the rate of fibrin clot destruction byPm [45].
Isolated Pg fragments containing different sets ofthe kringle domains can be produced in vitro by lim�ited proteolysis by pancreatic elastase [46], chymot�rypsin [47], pepsin [48], metalloproteinases [49], andPm (at high pH) [50] (Fig. 1).
During the two last decades, it was found that frag�ments Pg/Pm containing kringle domains exhibit spe�cific functions, which are not typical for the precursormolecule. The first information about their ability toinhibit angiogenesis was obtained in 1994 by O’Reillyet al. studying causes of intense neovascularizationand growth of metastases after surgical removal of theprimary tumor [13]. A protein isolated from urine ofmice with transplanted Lewis lung carcinoma exhib�ited antitumor activity. It was identical to a fragment ofPg consisting of the first four kringle domains. The iso�lated protein demonstrated potent anti�angiogenic

96
BIOCHEMISTRY (MOSCOW) SUPPLEMENT SERIES B: BIOMEDICAL CHEMISTRY Vol. 8 No. 2 2014
TYKHOMYROV et al.
properties: it completely arrested the growth of newblood vessels in the growing metastatic tumor. Cur�rently, the term “angiostatin” defines a group of Pgfragments containing kringle domains (K1�3, K2�3,K1�4, K1�4,85, K1�5), as well as individual kringles,
which decrease angiogenesis. The inhibition of thisprocess is based on the ability of Pg fragments to sup�press proliferation and migration of endotheliocytes.Isolated fragments obtained by proteolysis, as well asrecombinant proteins, showed varying activity (table).
Glu�plasminogen
Plasmin Elastase
Micro�plasminogen Mini�plasminogen
Pepsin
Chymotrypsin
Elastase
K1�4,85 K1�4
K1�3 K4 K5
K K2�3
1
2
3 4 5
12
3 4 5
4 5
12
3
1
2
3 4 5
12
3
Fig. 1. The main pathways of angiostatins formation during limited proteolysis of Glu�plasminogen by various proteases.
The effect of plasminogen fragments (angiostatins) on proliferation and migration of endotheliocytes [51–56]
Plasminogen fragments
Inhibition of endotheliocyte proliferation Inhibition of endotheliocyte migration
effect IC50, nM effect IC50, nM
K1 + 320 +/– >1000
K2 + <K1, K3 + >100
K3 + 460 + >100
K4 – – + 500
K5 +++ 50 +++ 50
K1�3 +++ 70 +/– >1000
K2�3 + ≈K2 ++ 100
K1�4 ++ 135 +++ 50
K1�4,85 +++ 10 +++ 0.05
K1�5 +++ 0.05 + 600

BIOCHEMISTRY (MOSCOW) SUPPLEMENT SERIES B: BIOMEDICAL CHEMISTRY Vol. 8 No. 2 2014
ANGIOSTATINS IN DIABETES 97
For example, it was demonstrated that K5 could effec�tively suppress both proliferation and migration ofendotheliocytes, while K1�3 and K1�4 selectivelyaffect only proliferation or migration of these cells.The highest antiproliferative activity was reported forK1�5 and the product of Pm proteolysis, consisting ofthe first four kringle domains and 85% of the K5amino acid sequence (K1�4,85). They suppress prolif�eration and migration of endotheliocytes in picomolarconcentrations. Impairments of the structural integ�rity of the first four kringle domains by the reduction ofdisulfide bonds resulted in the loss of their activity,whereas the reduction of K5 stimulated its activity.These results indicate that the biological activity ofthese fragments strongly depends on the structure ofkringle domains and their effects can be realized viadifferent molecular mechanisms.
At least seven protein targets of AS have been iden�tified on the surface of the endotheliocyte plasmamembrane: F1F0 ATP�synthase, angiomotin, integrinαvβ3, annexin II, HGF�receptor (c�met), proteogly�can NG2, β�actin [15, 57]. It was found that AS bind�ing to ATP�synthase leads to the induction of apopto�sis. However, subsequent molecular events accompa�nying interactions with other molecular targets andinvolving various signaling pathways require moredetailed study. Suppression of the endotheliocyte acti�vation by AS may also occur indirectly. AS are physio�logical antagonists of VEGF; they are involved in reg�ulation of expression of this pro�angiogenic factor. Forexample, it was shown that AS reduced the VEGFlevel [58], and inhibited VEGF/bFGF�induced acti�vation of mitogen�activated kinases ERK1 and ERK2[59]. In the retinal capillary cells AS simultaneouslyreduced the VEGF level and stimulated the produc�tion of another potent suppressor of angiogenesis,PEDF [60].
It is believed that the anti�angiogenic effect of krin�gle�containing fragments of Pg determines their anti�tumor activity. The effectiveness of AS was demon�strated using various experimental tumor models inmice: hemangioendothelioma, glioma, liver cancer,lung cancer, breast cancer, ovarian cancer, colorectalcancer. However, high clearance of systemicallyadministered AS (mainly determined by the rate oftheir elimination by the kidneys) necessitates regularadministration of high doses of angiostatics sufficientto achieve a significant therapeutic effect. Develop�ment of approaches, which would improve the effi�ciency of the angiostatic action of Pg fragments, is oneof priorities in therapy of cancer and a number of vas�cular disorders [61].
In vivo AS formation from Pg occurs in plasma, inthe extracellular matrix and on the cell surface andinvolves metalloproteinases (MMP)�2, �3, �7, �9, �12,and �19, and cathepsin D (K1�4), MMP�3 (K5) andneutrophil elastase (K1�3) [62]. Serine proteinasewith Mm of 13 kDa secreted by glioma cells causes the
formation of K1�5. Pm formed on the surface of cellsfrom Pg, activated by t�PA or u�PA, may also serve asthe source of AS in the body. Pm autolysis with forma�tion of K1�4,85 was observed in the presence of phos�phoglycerate kinase secreted by HT1080 fibrosarcomacells and cysteine or reduced glutathione as donors ofsulfhydryl groups [63]. AS formation by autolysis ofPm complexed with β�actin exposed on the plasmamembrane surface was detected in a prostate cancercell culture [64]. It is suggested that AS generationmay occur on the surface of many other cells present�ing actin (normal fibroblasts, endothelial and smoothmuscle cells, platelets, macrophages, etc.) [65]. Thus,various cell types can form AS either by secreting pro�teolytic enzymes, or by exposing cofactor proteinsinvolved in this process on the cell surface.
Using highly sensitive immunochemical methods,AS were detected in various human body fluids:plasma and serum, urine, ascite and ophthalmic fluid.In normal plasma, they are present in very low con�centrations (6–8 nM) or are not detected at all [61]. Ina number of cancers their level increases depending onthe tumor progression [66].
AS exhibit a wide range of pharmacological activi�ties and their effects are not limited by endothelio�cytes. It was found that AS inhibit HGF�induced pro�liferation and migration of smooth muscle cells invitro and in vivo [67]. The K1�4 and K1�3 fragmentsinfluence neutrophil migration induced by chemok�ines and HIV�Tat�protein [68]. Human recombinantK1�3 reduces the degree of macrophage infiltration inexperimental models of atherosclerosis. K1�3 dose�dependently blocked chemoattractant�inducedmigration of murine macrophages and human mono�cytes in a dose�dependent manner by disruption ofactin cytoskeleton rearrangement underlying filopo�dia/lamellipodia formation and cell locomotion [18].It was demonstrated that AS inhibit osteoclast activity,thus inhibiting bone resorption [69].
A broad spectrum of modulating effects of AS fordifferent cell types suggests the involvement of thesemolecules in various normal and pathophysiologicalprocesses. It was found that the development ofpathologies associated with activation of inflamma�tory processes (rheumatoid arthritis, DM, psoriasis,atherosclerosis, peptic ulcer disease, etc.) is accompa�nied by qualitative and quantitative changes in levels ofAS [7–9, 70, 71]. The anti�inflammatory and anti�adhesive effects of AS were first discovered by Chava�kis et al., who found that AS inhibited the integrin�mediated leukocyte adhesion to extracellular matrixproteins and the endothelium, and migration of leu�kocytes across the endothelium [72]. The same studyalso demonstrated that AS reduced activation ofNFκB, as well as NFκ�associated expression of thetissue factor (TF), a potent inducer of thrombogene�sis. These observations determine prospects of AS asmarkers of pathologies of various etiology and the

98
BIOCHEMISTRY (MOSCOW) SUPPLEMENT SERIES B: BIOMEDICAL CHEMISTRY Vol. 8 No. 2 2014
TYKHOMYROV et al.
development of effective approaches to their treat�ment [73].
2. ANGIOSTATINS IN DIABETIC RETINOPATHY AND CORNEAL LESIONS
Retinopathy followed by subsequent maculardegeneration develops in 50–98% of DM patientswithin 15 years after diagnosis and is the most com�mon diabetic complication. Diabetic retinopathy(DR) has several stages of development, each of whichis manifested by certain pathological factors. Earlystages of DR are characterized by the appearance ofmicroaneurysms accompanied by increased perme�ability of the BRB. The latter pathological conditionsare complicated by macular edema, ischemic changes(focal occlusion of capillaries), dilation of venules,basal membrane thickening, pericyte degeneration at
an abnormally high level of proliferation of fibroblastsand endothelial cells. It should be noted that the clin�ical manifestations of DR in patients with insulin�dependent and insulin�resistant DM differ signifi�cantly: insulin�dependent DM is accompanied byproliferative angioretinopathy, and insulin�resistantDM, by maculopathy. The main problems in the treat�ment of this complication are associated with retinaldetachment and intraocular hemorrhage, and so pro�phylaxis of retinal neovascularization is a prioritydirection of therapeutic approaches [74].
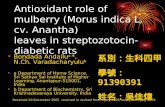
A complex cascade of metabolic rearrangementsshown in Fig. 2 precedes changes at the cellular level,leading to impairments of angiogenesis. Retina is astructure with a relatively high metabolic activity, thehigh level of cellular respiration and oxygen require�ments, so the diabetes�induced tissue ischemia canlead to irreversible consequences. It is known that
Hyperglycemia
Inflammation Proteases Polyol pathway of
ROS
Proliferative
Vitreous hemorrhage
Fibrosis Deterioration orDiabetic
Increased
PKC activation
macularedemaloss of vision
diabeticretinopathy
glucose oxidationAGE
Pg
AS
VEGF
(IL�1β, TNF�α, ICAM�1)Hypoxia
(HIF�1α) (u�PA, Pm, MMP)
vascularpermeability
Fig. 2. The angiostatin effect on the main pathogenetic mechanisms of diabetic retinopathy (solid arrow—activation or increasedexpression, dashed arrow—inhibition), (modified from [76, 77]).

BIOCHEMISTRY (MOSCOW) SUPPLEMENT SERIES B: BIOMEDICAL CHEMISTRY Vol. 8 No. 2 2014
ANGIOSTATINS IN DIABETES 99
conditions of prolonged hypoxia and hyperglycemiafavor accumulation of advanced glycation end prod�ucts (AGE), which are potent inducers of oxidativestress. AGE trigger irreversible biochemical changes inthe structure of proteins, activate endotheliocytes, andprovoke fibrosis of diabetic tissues, and also causeexcessive production of free radicals, including ROS,which, in turn, activates the main pathways of celldamage. It is known that ROS, synergistically withHIF�1α, increased expression of both VEGF and itsreceptor. VEGF is a potent angiogenic factor, alsoknown as the VPF (vascular permeability factor), andits angiogenic potential is 50 thousand times higherthan that of histamine [75–77].
Acting even at ultralow concentrations, VEGFgreatly enhances the permeability of retinal microves�sels [78]. Elevated expression of VEGF in the ischemicretinal tissue leads to accelerated proliferation ofendotheliocytes followed by the formation ofmicrovessels with impaired structure. It is also sug�gested that the VEGF induced retinal microvascularangiopathies affecting metabolism of occlusin, a tightjunction protein. VEGF activates PKC, particularly,its isoform PKCβ. Phosphorylation, abnormal redis�tribution of occlusin, ubiquitination and VEGF�induced endocytosis of this protein, cause impair�ments of the structure of tight junctions and subse�quent increase in vascular permeability and disruptionof BRB [79]. It was shown that intravitreal administra�tion of a gene expression construct encoding K1�4decreased the retinal content of VEGF in diabetic ratsand had a protective effect on the components of tightjunctions that resulted in normalization of capillarystructures [24].
Imbalance in the system of angiogenesis regula�tion, due to impairments of numerous feedback con�nections between its main components, leads to thedevelopment of local vascular pathologies. For exam�ple, activation of MMP�2 and MMP�9 involved in thedegradation of the tight junctions and enhancing vas�cular permeability, also leads to increased levels of ASdue to limited proteolysis of Pg. IL�1β is one ofinflammatory mediators, which is sharply increased inthe diabetic retina; on the one hand, it enhancesVEGF�induced microvascular permeability andinduces apoptosis via the activation of factor NF�κB,and on the other hand, it activates synthesis of Pg, thesource of AS [80, 81].
Laser photocoagulation is known to be a successfulapproach to the DR therapy and prevention of futurevision loss. One of the mechanisms underlying thepositive effects of photocoagulation is an increase inthe level of endogenous AS in the retinal tissueaffected by reduced content of VEGF. It was shownthat the observed changes in the balance of regulatoryfactors occur locally: the photocoagulation proceduredoes not affect the levels of circulating plasma AS. It issuggested that generation of AS from Pg, which is syn�
thesized in adequate amounts by retinal and vitreousbody cells, can be carried out in situ by metalloelastaseof activated macrophages [82].
A currently developed complex approach to theDR therapy combines the use of conventional laserphotocoagulation and targeted delivery of a gene con�struct with the vector providing long�term expressionof an angiostatic transgene. For expression of DNAencoding AS (K1�4), Lai et al. used a rAAV�based vec�tor (rAAV�AS) [83]. It was shown that subretinaladministration of rAAV�AS to rats with streptozocin(STZ)�induced DM significantly reduced the degreeof permeability of the capillaries and the developmentof choroidal neovascularization induced by laser pho�tocoagulation. Application of this gene delivery systemopens wide perspectives for therapy of ocular diseases,as rAAV�AS has a high stability and prolonged expres�sion, which ensures a significant therapeutic effecteven after a single injection.
Sima et al. [24] studied the effect of K1�4 on theexpression of VEGF and a number of physiologicalparameters of the retina of diabetic animals. As aresult, a single injection of 7.5 μg K1�4 in the vitreousbody significantly decreased retinal vascular perme�ability in rats with oxygen�induced and diabetic retin�opathy. At the cellular level the described effects of AScorrelated with the decrease of abnormally highVEGF level in the retinal tissue of diabetic animals. Atthe same time, AS had no effect on the VEGF leveland retinal vessels condition of healthy rats. Based onthese data, it was suggested that AS inhibit the devel�opment of proliferative retinopathy by direct inhibi�tory effect on vascular endotheliocytes, mainly due tothe suppression of VEGF synthesis under conditionsof retinal hypoxia induced by chronic hyperglycemia.A proposed molecular mechanism, by which AS mayinhibit the synthesis of VEGF, includes the followingevents. It is known that hypoxia induces phosphoryla�tion of p42/p44 MAP kinase, which in turn leads to anincrease in the level of VEGF due to stimulation of itstranscription by the activator protein AR�2/Sp1. ASinhibits p42/p44 MAP kinase phosphorylation andthus inhibits VEGF expression in hypoxic conditions.It was shown that intravitreal administration of therAAV�AS construct to diabetic rats caused a paralleldecline in the phosphorylation level of p42/p44 MAP�kinase and the retinal content of VEGF observed onthe next day after the construct administration to ratswith STZ�induced diabetes [24].
Despite the fact that most of the studies on the DRmodels were carried out using Pg fragments consistingof the first three or four kringle domains, there isincreasing evidence that K5 can play a special role inthe regulation of retinal neovascularization. The firststudies of the biological activity of K5 showed that thisPg fragment is one of the most potent inhibitors ofproliferation and migration of endotheliocytes, as wellas an inducer of the apoptosis of these cells [85, 86].

100
BIOCHEMISTRY (MOSCOW) SUPPLEMENT SERIES B: BIOMEDICAL CHEMISTRY Vol. 8 No. 2 2014
TYKHOMYROV et al.
Transfection of ovarian tumor cells and the tumor cellline NV with the adenoviral vector comprising a DNAsequence encoding K5 resulted in inhibition of cancercell growth [87].
The effects of K5 on retinal neovascularization inDR attract much interest. K5 appears to be a promis�ing therapeutic agent for the treatment of the diabeticcomplication [88]. Introduction of a genetic constructencoding K5 sequence in retinal cells reduced thedegree of capillary permeability, inhibited VEGF over�expression and retinal neovascularization underischemic conditions [89]. The same study also demon�strated that K5 reduced VEGF expression by Mullercells in vitro. It is known that Muller cells are themajor retinal glial cells, they provide support, trophicand protective functions for retinal neurons and arethe major source of pro�inflammatory and pro�angio�genic factors in the retina (including VEGF) [90]. Thisexplains why Muller cells play an important role in ret�inal neovascularization in hyperglycemic conditions.Studies on identification of a K5 binding site/receptoron the surface of these cells are in progress now. Thereis evidence that the K5 binding site on the surface ofMuller cells do not interact with other AS, includingK1�4, thus indicating specific nature of K5 interactionwith cells. It is suggested that the physiological effectsof this Pg fragment are realized due to the specific andhigh affinity binding to a voltage�gated anion channelas is the case of endotheliocytes. The decreased level ofK5 receptor (K5R) expression was observed both inthe culture of Muller cells during hypoxia or hypergly�cemia (damaging factors that mimic some stages ofproliferative diabetic retinopathy), and in rat retina inexperimental models of oxygen� and STZ�inducedretinopathies. Incubation of Muller cells in patholog�ical conditions with K5 maintained the levels of K5Rand this was considered as the main reason for sup�pression of VEGF expression [89]. Despite theseencouraging results, further studies are clearly neededto elucidate the mechanisms of the AS angiostaticeffect of K5, as well as the nature and features of itsreceptor.
The suggestion that AS are important regulators ofmetabolism of pro�angiogenic and anti�angiogenicfactors is supported by the AS effect on the level ofPEDF, the other suppressor of angiogenesis. Adecrease of the retinal PEDF is one of factors, whichare closely associated with the ischemia�induced reti�nal neovascularization and proliferative diabetic retin�opathy [91]. However, results of studies on the ASeffect on the PEDF expression are rather contradic�tory. For example, it was shown that administration ofK5 in a dose�dependent manner increased the PEDFlevel in the vascular endothelial cells and retina [60],whereas retinal transfection of a gene engineered con�struct encoding K1�4 had an insignificant effect on thePEDF content in the retina and HUVEC�2C cells[27]. It is possible that the differences in the effective�ness of certain types of AS are associated with struc�
tural features of the kringle domain acceptor bindingsites and/or the presence of unique receptor bindingsites on the surface of retinal cells.
To date there are no non�invasive methods fortreatments of such ophthalmic diseases as DR and dia�betic uveitis induced by impairments of microvascularpermeability and macular edema (the main causes ofvision deterioration and vision loss in diabeticpatients). Results of experimental studies using bothAS and the engineered constructs expressing AS arerather promising in terms of the development of newhighly effective and minimally invasive therapies ofsuch pathologies.
Pathological changes in the cornea, which often donot manifest clinically, may also occur in diabeticpatients. Nevertheless, DM often leads to the develop�ment of inflammatory processes in the cornea andkeratoses, accompanied by accumulation of cellularelements in the tissue, neovascularization and conse�quently, attenuation of light transmission. In this con�text, the control of corneal neovascularization is aprincipal precondition for maintaining its transpar�ency. As in the retinal tissue, components of thePg/Pm system, including AS, and also PEDF, TSR,ES and maspin, normally prevent neovascularizationof the cornea, and their profiles reflect its functionalstate [92, 93]. The human corneal level of Pg (1.1 μgper the retina, which corresponds to 122 nM) is suffi�cient for the formation of physiologically significantquantities of AS [81]. Studies performed using cul�tured corneal sections showed that corneal epithelialcells and fibroblasts can produce Pg and convert it intovarious fragments, including AS [94]. In the case of Pgproteolytic fragments the IC50 value (concentrationcausing 50% inhibition) for proliferation of vascularendothelial cells was about 40 nM. It should benoted that Pg synthesis in corneal cells was stimulatedby IL�1β, thus suggesting a possible control of thisprocess by paracrine factors [81].
A role of AS in regulation of corneal neovascular�ization in vivo was originally demonstrated by Kaoet al. [95] and Drew et al. [96] in experiments with Pggene�knockout mice.
The corneal tissue of Pg�deficient mice containedfibrin deposition, accompanied by inflammatory reac�tions and blood vessel invasion. AS prevented bFGF�and VEGF�induced corneal neovascularization andpromoted regression of newly formed vessels [97].Gabison et al. [98] demonstrated that administrationof antibodies to AS K1�3 and K1�5 into the of laser�treated mouse cornea resulted in an intensive prolifer�ation of capillaries due to AS inactivation and a shift ofthe angiogenic balance towards neovascularization. Atthe same time, administration of antibodies to the Pgproteinase domain was not accompanied by the above�described effect. Daily systemic administration of2 mg/kg K1�5 to mice with FGF�induced cornealneovascularization facilitated blockade of the growth

BIOCHEMISTRY (MOSCOW) SUPPLEMENT SERIES B: BIOMEDICAL CHEMISTRY Vol. 8 No. 2 2014
ANGIOSTATINS IN DIABETES 101
of new blood vessels. In this context, administration ofK1�4 at the same dose was not accompanied by inhi�bition of the induced neovascularization.
Epithelial cells and corneal fibroblasts can secretevarious proteases, including MMPs and Pg activators,which play an important role in cell migration, angio�genesis regulation and wound healing [99]. In con�trast, myofibroblasts characterized by a lower mobilitythan fibroblasts, lack the ability to hydrolyze Pg to AS.TGFβ induced transformation of fibroblasts intomyofibroblasts; however, it is also known that this fac�tor inhibits the secretion of two MMPs (gelatinase andstromelysin), which are responsible for AS generation[100]. The use of AS as endogenous (and thereforelacking side effects) angiostatics may be a promisingtreatment for pathological corneal neovascularization.
Thus, the AS�dependent regulation of angiogenesisin the cornea and retina shares numerous commonfeatures. However, one should take into considerationan important feature of the corneal physiology: this isthe ability to function under hypoxic conditions of aclosed eye. It is well known that lack of oxygen supplyinduces production of factors, which trigger a cascadeof compensatory processes leading to the formation ofnew blood vessels and increased blood supply. In thiscontext the study [101] is especially interesting; itdemonstrated that human corneal neovascularizationwas not activated even when the eye was closed for anextended time interval sufficient for the increase oflevels of pro�angiogenic factors. The authors attrib�uted this fact to the AS formation from Pg in the tearfluid of the closed eye. Indeed, tears collected after anovernight sleep, had higher levels of Pg, and also K1�3,K1�4, and intact K5 exhibiting a potent anti�angio�genic activity. Based on these data it was concludedthat Pg fragments protect the cornea under conditionsof forced hypoxia; this protective role consists in pre�vention of neovascularization and inflammation.
3. ANGIOSTATINS IN DIABETIC NEPHROPATHY
Diabetic nephropathy (DN) is the main cause ofchronic renal failure, which is the gradual kidneydamage up to complete renal dysfunction. Nephropa�thy develops in 20–40 and 10–20% of patients withtype I and type II diabetes, respectively. Histologically,this pathology is characterized by mesangial matrixproliferation, sclerosis, glomerular basement mem�brane thickening, hyaline deposition in the glomerulararterioles. It is believed that podocytes and mesangialcells play a key role in the DN development; however,structural anomalies of the renal microvasculature,leading to its increased permeability and microalbu�minuria also contribute to pathogenesis of this disease.As in the case of retinopathy, the increase in densityand length of the glomerular capillaries is the result ofpathological neovascularization in hyperglycemic
conditions and a key factor in the development ofglomerular hypertrophy [10, 102].
Comparing DN with the development of prolifera�tive DR, it should be noted that increased expressionof VEGF, especially its two isoforms, VEGF�A164 andVEGF�A188, is one of the reasons for the abnormallyhigh level of angiogenesis in renal glomeruli in theearly stages of DN development [103]. Inflammatoryprocesses are also an important etiologic factor of DN.Increased levels of pro�inflammatory cytokines suchas TNF�α, MCP�1, ICAM�1, and IL�18 do correlatewith the development of diabetic renal failure. It isbelieved that among all most significant angiopoietins,TGF�β is most important inductor of DN. Theincrease in the renal glomerular level of TGF�β in dia�betes leads to accumulation of extracellular matrix byactivating the synthesis of fibronectin and inhibition ofcollagen degradation [104].
Despite limited information on a crucial role of ASin the development of DN there is unquestionable evi�dence for their involvement in the pathogenesis of thisdisorder. Using Western blot, the presence of Pg and itsproteolytic fragments with Mm of 50 and 38 kDa wasdemonstrated in renal tissues of animals with nor�moglycemia [105]. Six weeks after the induction ofSTZ�diabetes, rats had polyuria, microalbuminuria,inflammation, and a significant decrease the levels ofrenal AS as compared with control. In the same sam�ples the content of intact Pg exceeded the controlvalue, while the renal level of mRNA MMP�2 and theenzyme activity were significantly reduced in diabeticrats as compared with healthy animals [27]. Theseresults indicate that inhibition of proteases involved inthe generation of AS, rather than changes in Pg geneexpression, is the main cause determining the rate ofAS formation in tissues.
Changes in the balance of regulatory factors andthe activity of key proteases observed in the kidneyduring DN progression lead to a significant (approxi�mately 2�fold) increase of the vascular wall AS level indiabetic as compared with patients with renal insuffi�ciency of another origin [105]. It is known that NO isinvolved in the development of the angiogenic signalinduced by VEGF. Under conditions of end�stagerenal disease the vascular tissues are characterized byboth low levels of VEGF, and decreased activity ofeNOS. The observed decrease of VEGF expressionmay be due to impaired insulin�mediated activation ofthe PI3K/Akt signaling pathway [27, 106]. Thisincrease in the AS levels may be one of the causes ofthe decreased density of renal microvessel, inhibitionof eNOS and impairments in the acetylcholine�induced vasodilation, which is considered to be a pos�itive regulator of neovascularization [107]. Activationof MMP, particularly MMP�2 and MMP�9, which arealso responsible for the degradation of elastin fibers ofarterial stiffness and calcification, is considered as thereason for high levels of AS [27]. The role of other pro�

102
BIOCHEMISTRY (MOSCOW) SUPPLEMENT SERIES B: BIOMEDICAL CHEMISTRY Vol. 8 No. 2 2014
TYKHOMYROV et al.
teases involved in limited hydrolysis of Pg (in particu�lar MMP�3, �7, and �12) remains to be clarified.Interestingly, the age�related changes in the tissues ofthe kidneys affecting the balance of angiogenesis regu�lators, share common features with the changesobserved in the development of DN. Authors of [22]found that aging of rats is accompanied by theincreased renal AS levels. This effect is attributed tothe activation of cathepsin D, which occurs due toreduction of the physiological level of tissue inhibitorsduring aging. This example seems to support the exist�ing paradigm of DM as one of the factors of acceler�ated aging.
Chronic inflammation is yet another importantlink in the development of DN. The early stages of thisdisease are characterized by a sharp increase in the lev�els of such pro�inflammatory factors as MCP�1,TNF�α, ICAM�1, and IL�18 [108]. In this contextMCP�1 attracts special attention; this chemokineinduces monocyte migration and differentiation ofmacrophages and also enhances synthesis of extracel�lular matrix components that provokes interstitialfibrosis in diabetic kidneys [109]. The authors of [26]confirmed previous data on the anti�inflammatoryeffect of AS: they found that AS inhibited TGF�β�induced secretion of MCP�1 in mesangial cells underhyperglycemic conditions. In addition, the sameresearchers found that ATP�synthase is a potentialreceptor for AS on the surface of mesangial cells. It isknown that high levels of renal tissue PEDF have aprotective effect under DN conditions. Administra�tion of a gene engineered construct encoding the ASsequence K1�4 to the kidney, but not to the retina pre�vented TGF�β� and angiotensin II�induced reductionof the PEDF level. The suggestion that the protectiveeffect of AS in kidneys is realized due to its anti�inflammatory activity is supported by results of Mu etal. [110]. Using the model of chronic renal failure ofnon�diabetic origin these authors demonstrated thatexpression of the gene encoding AS promoted reduc�tion of interstitial fibrosis during inhibition of mac�rophages and T�lymphocytes infiltration.
During the development of therapeutic approachesto the regulation of neovascularization in conditions ofdiabetes�associated renal failure one should take intoconsideration the stage of this pathology. By analogywith tumor growth, it is reasonable to suggest thatunder conditions of the deficit of angiogenesis sup�pressors (on early stages of DN) a strategy for inhibi�tion of growth factors, including VEGF, and/or theirreceptors (FLK�1, FLT�1 and Tie2) would be effectiveas the anti�angiogenic therapy [111, 112]. Indeed, theuse of specific VEGF�neutralizing antibodies effec�tively reduced the degree of hyperfiltration, albumin�uria and renal glomerular hypertrophy in rodents withexperimental diabetes [113]. However, it is unlikelythat these antibodies can be used for the treatment ofnephropathy in diabetic patients due to the risk of sideeffects (hypertension, various hemostatic disorders,
proteinuria), which have been observed in patientswith rectal cancer during trials [114]. The use of vari�ous angiostatics (including AS) is currently consideredas a promising alternative approach to the prophylaxisand treatment of DN. However, it should be kept inmind that mesangial cells but not endotheliocytes arethe main renal targets of AS. Delivery of a gene engi�neered construct encoding the AS sequence to kidneyof diabetic rats by means of an adenoviral vectorreduced microglobulinuria almost to the normal level[26]. In the early stages of DN development microal�buminuria is closely associated with glomerular hyper�trophy. It was shown that it is possible to reduce abnor�mally high levels of VEGF and TGF�β and thereby toattenuate the degree of the renal glomerular damageby means of compensation of the renal level of ASdue to expression of the gene�engineered constructcarrying its sequence. Moreover, further in vitro exper�iments using renal glomerular mesangial cells showedthat AS effectively inhibited mechanisms controllingthe TGF�β signaling pathway: they effectively inhib�ited expression of MCP�1 and fibronectin. It wasfound that the same concentration of AS had no effecton the growth of mesangial cells; consequently, reduc�tion of the fibronectin production was not associatedwith a decrease in the number of cells synthesizingfibronectin. It is suggested that this effect may be (atleast partially) explained by inhibition of expression ofthe transcription factors Smad, which are the majortransducers of the TGF�β signaling pathway [26].
In summary, we can conclude that the protectiveeffects of AS during DN development are realized viainhibition of synthesis and activity of pro�angiogenic(VEGF and TGF�β) and proinflammatory (MCP�1)factors and activation of endogenous synergistic fac�tors such as PEDF. Comparison of the data concern�ing the effects of different types of AS in DR and DNsuggests the existence of some specific features of theiractions in different tissues.
4. ANGIOSTATIN AND CARDIOVASCULAR DISEASES IN DIABETES
Cardiovascular diseases (CVD) caused by the dam�age of both myocardial and coronary vessels are thecause of high mortality among diabetic patients. His�tologically, myocardial diabetic microangiopathy ischaracterized by thickening of the basement mem�brane of small vessels, endothelial cell proliferation,appearance of aneurysms. Besides microangiopathy,DM often provokes the development of myocardialdystrophy, coronary atherosclerosis, and diabetic car�diac autonomic neuropathy. It was found that thedevelopment of diabetic vascular dysfunctionsinduced changes in the functioning of endothelial andsmooth muscle cells and platelets. Insulin resistanceand dyslipidemia cause the development of coronaryatherosclerosis almost in every diabetic patient.Development of collateral vessels due to the activation

BIOCHEMISTRY (MOSCOW) SUPPLEMENT SERIES B: BIOMEDICAL CHEMISTRY Vol. 8 No. 2 2014
ANGIOSTATINS IN DIABETES 103
of angiogenesis can be regarded as an important adap�tive response in the body, compensating problems ofblood flow (up to cardiac arrest), particularly associ�ated with deposition of atherosclerotic plaques. Col�lateral circulation provides blood flow through the sideanastomoses, possibly, due to the high plasticity of theblood vessels, controlled by angiopoietin and anti�angiogenic factors. However, in diabetic patients cor�onary collateral formation is suppressed and thisresults in tissue ischemia and increases the risk ofmyocardial infarction [115, 116].
Molecular mechanisms underlying the develop�ment of diabetes�associated CVD are now underdetailed study. Certain evidence exists that hypergly�cemia inhibits NO production by vascular endothelialand smooth muscle cells by blocking eNOS andby activating generation of ROS, particularly superox�ide anion radical. Increased glucose levels and associ�ated decrease of eNOS activity lead to inhibition ofHIF�1α activity; this transcription factor regulatesexpression of the VEGF gene [75]. In non�diabeticpatients increased levels of VEGF in CVD (includingmyocardial infarction) are among triggering mecha�nisms for formation of new vascular collaterals. How�ever, diabetes is characterized by a sharp decrease inthe levels of VEGF, as well as VEGF receptors(VEGFR) in the aortal wall and the myocardium.Reduced capillary density in patients with diabeticcardiomyopathy correlated with decreased levels ofVEGF165 and VEGFR, and in the ventricles of dia�betic patients the levels of transcription of VEGF andits receptor was 2�fold lower than the normal values[117].
Some researchers suggest that these are the key fac�tors associated with the development of CVD compli�cations in diabetic conditions. Nevertheless, it shouldbe noted that in addition to aberrations of mitogenmetabolism, impaired regulation of activity of someproteases responsible for the formation of angiogene�sis inhibitors (especially AS) also represents an impor�tant pathogenic element [118]. In hyperglycemic con�ditions a low vascular level of NO is a signal provokingactivation of MMPs, especially MMP�2 and MMP�9.It is known that MMP activity is regulated at the tran�scriptional level, activation of corresponding proen�zymes, and endogenous tissue inhibitors (TIMP). Thestudy [119] revealed a tight correlation betweendecreased levels of TIMP�2, activation of MMP�2 andMMP�9 and increased generation of proteolytic Pgfragments with Mm of 40–45 kDa in the vascular wallsof diabetic patients. Impairments in the activation�inhibition balance of some proteases taking place inDM are important factor influencing the developmentof vascular pathologies. Characterization of the func�tioning of AS�generating enzymes in diabetes, as wellas search for possible ways of their regulation, may bea promising approach to the treatment of coronaryheart disease and prophylaxis of acute heart failure indiabetic patients. Promising results have been reported
in [120] showing that normalization of blood glucosewith insulin resulted in a significant inhibition of ASgeneration in the diabetic animals. The decrease in theAS content correlated with improvement of perfusionof ischemic areas of the myocardium. However, theeffect of insulin on the activity of enzymes responsiblefor limited proteolysis of Pg, in particular, MMP,remains poorly investigated. It is known that tissueROS levels sharply elevated during the development ofdiabetes, induce the conversion of inactive MMP pre�cursors (zymogens) into mature active forms [120]. Itwas also shown that the use of antioxidants reducedMMP�9 activity in the aorta of animals at experimen�tal hyperglycemia.
The data described above are supported by a num�ber of other studies. An experiment modeling diabetesby alloxan administration to mini�swines revealedendothelial dysfunction associated with decreaseddensity of endothelial cells. This was accompanied byan increase in the levels of endogenous angiogenic fac�tors (AS and ES) in myocardial tissue of the diabeticanimals [121]. An imbalance of regulators of angio�genesis deteriorated via VEGF�mediated signalingpathways can be considered as one of the main causesof impaired coronary microcirculation. Using a myo�cardial biopsy material from patients with type II dia�betes it was found [122] that although VEGF levelsexceeded the normal range, this was accompanied bydecreased activity of its receptor and signaling path�ways aberration. In contrast to these results, anotherstudy revealed a decrease of the VEGF levels in mini�swines with experimental diabetes in response tochronic ischemia [123]. These differences may beattributed to interspecies peculiarities of the diabeticprocess; it is also possible that antidiabetic agents usedfor therapy of diabetic patients could also contribute tothese differences. In model experiments, occlusion ofthe coronary arteries in dogs with normoglycemia wasfound to trigger intensive formation of vascular collat�erals, while in animals with increased glucose levels(>19 mmol/L) such occlusion was not accompaniedby the increased levels of myocardial perfusion [124].The authors obtained experimental evidence thatproducts of Pg processing, formed in the myocardialtissue fluid inhibited proliferation of endotheliocytes;this resulted in inhibition of formation of new coro�nary collaterals. It has been shown that ischemic myo�cardial interstitial fluid of hyperglycemic animals wasnot able to stimulate proliferation of endotheliocytesand vascular tube formation in vitro in contrast to theinterstitial fluid, taken from normoglycemic animals.However, the addition of anti�AS antibodies to themyocardial fluid of hyperglycemic dogs to endothelio�cyte cell cultures restored the mitotic activity of thecells and their ability to form the vascular wall. Later,a number of adequate experimental models gave simi�lar results. Chronic diabetes�associated ischemia wasaccompanied by almost a 4�fold increase in the myo�cardial content of AS [123]. Thus, the development of

104
BIOCHEMISTRY (MOSCOW) SUPPLEMENT SERIES B: BIOMEDICAL CHEMISTRY Vol. 8 No. 2 2014
TYKHOMYROV et al.
approaches to the regulation of the local AS level willopen wide prospects for highly effective therapy ofsuch fatal diabetic complications as CVD. In the con�text of diagnosis of CVD, determination of the levelsof pro� and anti�angiogenic factors can be used forassessment of the functional status of coronary micro�circulation.
CONCLUSIONS
Despite certain progress in our understanding ofthe role of AS in the processes leading to the develop�ment of vascular disorders in DM, there are unsolvedissues that require further investigation.
AS are biologically active polypeptides exhibiting awide range of physiological activities, which obviouslyneed subsequent investigation in the context of theirpossible role in the pathogenesis, as well as diabeticcomplications, which were not discussed in thisreview, and also diabetes�related pathologies, such asneuropathy, encephalopathy, peptic ulcer disease, andatherosclerosis. Despite similar manifestations of thedisease in the case of type I and II diabetes (chronichyperglycemia, endothelial dysfunction, oxidativestress and inflammation, the risk of atherosclerosis),the mechanisms of AS�dependent regulation of angio�genesis and insulin resistance are still far from com�plete understanding. At the same time, elucidation ofthe AS role in the metabolism of other angiogenesisregulators also requires more detailed investigation.Most of the studies on the determination of tissue lev�els of AS were performed in model experiments onanimals with relatively short periods of the DM dura�tion. There are no data on the dynamics of changes inthe levels of angiogenesis regulators (including AS)during the development of chronic hyperglycemia inhumans. The studies of the isoform spectrum of AS,their tissue distribution and functional properties atdifferent stages of development of DM are also of greatscientific and practical importance.
ACKNOWLEDGMENTS
This work was supported by the Russian Founda�tion for Basic Research (project nos. 11�04�02066 and12�04�90444).
REFERENCES
1. Folkman, J., N. Engl. J. Med., 1971, vol. 285, no. 21,pp. 1182–1186.
2. Polverini, P.J., J. Dent. Educ., 2002, vol. 66, no. 8,pp. 962–975.
3. Poveshchenko, A.F. and Kononenkov, V.I., Usp. Fiziol.Nauk, 2010, vol. 41, no. 2, pp. 68–89.
4. Folkman, J., Eur. J. Cancer., 1996, vol. 32A, no. 14,pp. 2534−2539.
5. Carmeliet, P. and Rakesh, K.J., Nature, 2000, vol. 407,pp. 249−257.
6. Sluimer, J.C. and Daemen, M.J., J. Pathol., 2009,vol. 218, no. 1, pp. 7–29.
7. Hudson, N., Balsitis, M., Everitt, S., and Hawkey, C.J.,Gut, 1995, vol. 37, no. 2, pp. 191−194.
8. Heidenreich, R., Röcken, M., and Ghoreschi, K., Int.J. Exp. Pathol., 2009. vol. 90, no. 3, pp. 232–248.
9. Szekanecz, Z., Besenyei, T., Szentpétery, A., andKoch, A.E., Curr. Opin. Rheumatol., 2010, vol. 22,no. 3, pp. 299–306.
10. Watkins, P.G., Sakharnyi diabet (Diabetes Mellitus),Moscow: BINOM, 2006.
11. Xu, L., Kanasaki, K., Kitada, M., and Koya, D., Fib�rogenesis Tissue Repair, 2012, vol. 5, no. 1, p. 13.
12. Severina, A.S. and Shestakova, M.V., Sakharnyi dia�bet, 2004, vol. 4, pp. 38–42.
13. O’Reilly, M.S., Holmgren, L., Shing, Y., Chen, C.,Rosenthal, R.A., Moses, M., Lane, W.S., Cao, Y.,Sage, E.H., and Folkman, J., Cell, 1994, vol. 79, no. 2,pp. 315–328.
14. Sakurai, T. and Kudo, M., Oncology, 2011, vol. 81,no. 1, pp. 24–29.
15. Wahl, M.L., Kenan, D.J., Gonzalez�Gronow, M., andPizzo, S.V., J. Cell. Biochem., 2005, vol. 96, no. 2,pp. 242–261.
16. Lee,T.Y., Muschal, S., Pravda, E.A., Folkman, J.,Abdollahi, A., and Javaherian, K., Blood, 2009,vol. 114, no. 9, pp. 1987–1998.
17. Takahashi, S., Shinya, T., and Sugiyama, A., J. Pharmacol.Sci., 2010, vol. 112, no. 4, pp. 432–437.
18. Perri, S.R., Annabi, B., and Galipeau, J., FASEB J.,2007, vol. 21, no. 14, pp. 3928–3936.
19. Aisina, R.B., Mukhametova, L.I., Gulin, D.A.,Levashov, M.Yu., Gershkovich, K.B., and Varfolo�meev, S.D., Biochemistry (Moscow), 2009, vol. 74,no. 10, pp. 1104–1113.
20. Scapini, P., Nesi, L., Morini, M., Tanghetti, E., Bel�leri, M., Noonan, D., Presta, M., Albini, A., and Cas�satella, M.A., J. Immunol., 2002, vol. 168, no. 11,pp. 5798–5804.
21. Jurasz, P., Santos�Martinez, M.J., Radomska, A., andRadomski, M.W., J. Thromb. Haemost., 2006, vol. 4,no. 5, pp. 1095–1106.
22. Satoh, M., Kidokoro, K., Ozeki, M., Nagasu, H.,Nishi, Y., Ihoriya, C., Fujimoto, S., Sasaki, T., andKashihara, N., Lab. Invest., 2013, vol. 93, no. 3,pp. 334–343.
23. Klys’, Yu.G., Zaitseva, N.V., Kizim, A.I., and Verev�ka, S.V., Onkologiya, 2010, vol. 12, no. 1, pp. 17–21.
24. Shyong, M.P., Lee, F.L., Kuo, P.C., Wu, A.C.,Cheng, H.C., Chen, S.L., Tung, T.H., and Tsao, Y.P.,Mol. Vis., 2007, vol. 13, pp. 133–141.
25. Sodha, N.R., Clements, R.T., Boodhwani, M.,Xu, S.H., Laham, R.J., Bianchi, C., and Sellke, F.W.,Am. J. Physiol. Heart Circ. Physiol., 2009, vol. 296,no. 2, pp. 428–434.
26. Zhang, S.X., Wang, J.J., Lu, K., Mott, R., Longeras, R.,and Ma, J.X., J. Am. Soc. Nephrol., 2006, vol. 17,no. 2, pp. 475–486.
27. Chung, A.W., Yang, H.H., Sigrist, M.K., Brin, G.,Chum, E., Gourlay, W.A., and Levin, A., Cardiovasc.Res., 2009, vol. 84, no. 3, pp. 494–504.

BIOCHEMISTRY (MOSCOW) SUPPLEMENT SERIES B: BIOMEDICAL CHEMISTRY Vol. 8 No. 2 2014
ANGIOSTATINS IN DIABETES 105
28. Syrovets, T. and Simmet, T., Cell. Mol. Life Sci., 2004,vol. 61, nos. 7–8, pp. 873–885.
29. Zhernosekov, D.D., Yusova, E.I., and Grinenko, T.V.,Ukr. Biokhim. Zhurn., 2012, vol. 84, no. 4, pp. 5–19.
30. Godier, A. and Hunt, B.J., J. Thromb. Haemost., 2013,vol. 11, no. 1, pp. 24–34.
31. Lijnen, H.R., Ann. N.Y. Acad. Sci., 2001, vol. 936,pp. 226–236.
32. Zhang, L., Seiffert, D., Fowler, B.J., Jenkins, G.R.,Thinnes, T.C., Loskutoff, D.J., Parmer, R.J., andMiles, L.A., Thromb. Haemost., 2002, vol. 87, no. 3,pp. 493–501.
33. Ponting, C.P., Marshall, J.M., and Cederholm�Will�iams, S.A., Blood Coagul. Fibrinolysis, 1992, vol. 3,no. 5, pp. 605–614.
34. Xue, Y., Bodin, C., and Olsson, K., J. Thromb.Haemost., 2012, vol. 10, no. 7, pp. 1385–1396.
35. Collen, D. and Lijnen, H.R.J., J. Thromb. Haemost.,2004, vol. 2, no. 4, pp. 541–546.
36. Parry, M.A., Zhang, X.C., and Bode, I., TrendsBiochem. Sci., 2000, vol. 25, no. 2, pp. 53–59.
37. Cockell, C.S., Marshall, J.M., Dawson, K.M, Ceder�holm�Williams, S.A, and Ponting, C.P., Biochem. J.,1998, vol. 333, pp. 99–105.
38. Markus, G., Fibrinolysis, 1996, vol. 10, pp. 75–85.39. Lerch, P.G., Rickli, E.E., Lergier, W., and
Gillessen, D., Eur. J. Biochem., 1980, vol. 107, no. 1,pp. 7–13.
40. Geiger, J.H. and Cnudde, S.E., J. Thromb. Haemost.,2004, vol. 2, no. 1, pp. 23–34.
41. Lijnen, H., Hoylaerts, M., and Collen, D., J. Biol.Chem., 1980, vol. 255, no. 21, pp. 10214–10222.
42. Grinenko, T.V. and Kudinov, S.A., Biokhimiya zhivot�nykh i cheloveka (Animal and Human Biochemistry),Kiev: Naukova Dumka, 1991, vol. 15, pp. 66–76.
43. Grinenko, T.V., Yusova, E.I., Zadorozhnaya, M.B.,and Makogonenko, E.M., Ukr. Biokhim. Zhurn., 2002,vol. 74, no. 6, pp. 83–90.
44. Herren, T., Swaisgood, C., and Plow, E.F., Front.Biosci., 2003, vol. 8, pp. 1–8.
45. Andrianov, S.I., Makogonenko, E.M., and Kudi�nov, S.A., Ukr. Biokhim. Zhurn., 1992, vol. 64, no. 3,pp. 14–20.
46. Sottrup�Jensen, L., Zaidel, M., Claeys, H., Petersen, T.E.,and Magnusson, S., in Progress in Chemical Fibrinoly�sis and Thrombolysis, Davidson, V.F., Rowan, R.H.,Samama, M.M., and Desnoyers, D.C., Eds., NewYork: Raven Press, 1978, pp. 191–209.
47. Thewes, T., Ramesh, V., Simplaceanu, E.L., andLlinás, M., Biochim. Biophys. Acta, 1987, vol. 912,no. 2, pp. 254–269.
48. Lerch, P.G., Rickli, E.E., Lergier, W., and Gillessen, D.,Eur. J. Biochem., 1980, vol. 107, no. 1, pp. 7–13.
49. Ho, P.L., Serrano, S.M., Chudzinski�Tavassi, A.M.,Moura da Silva, A.M., Mentele, R., Caldas, C.,Oliva, M.L., Batista, I.F., and Oliveira, M.L.,Biochem. Biophys. Res. Commun., 2002, vol. 294,no. 4, pp. 879–885.
50. Shi, G.Y. and Wu, H.L., J. Biol. Chem., 1988, vol. 263,no. 32, pp. 17071–17075.
51. Cao, Y., Ji, R.W., Davidson, D., Schaller, J., Marti, D.,Söhndel, S., McCance, S.G., O’Reilly, M.S., Llinás, M.,and Folkman, J., J. Biol. Chem., 1996, vol. 271, no. 46,pp. 29461–29467.
52. Cao, R., Wu, H.L., Veitonmäki, N., Linden, P.,Farnebo, J., Shi, G.Y., and Cao, Y., Proc. Natl. Acad.Sci. USA, 1999, vol. 96, no. 10, pp. 5728–5733.
53. Cao, Y., Cao, R., and Veitonmäki, N., Curr. Med.Chem. Anticancer Agents, 2002, vol. 2, no. 6, pp. 667–681.
54. Ji, W.R., Barrientos, L.G., Llinás, M., Gray, H., Vil�larreal, X., DeFord, M.E., Castellino, F.J.,Kramer, R.A., and Trail, P.A., Biochem. Biophys. Res.Commun., 1998, vol. 247, no. 2, pp. 414–419.
55. Ji, W.R., Castellino, F.J., Chang, Y., Deford, M.E.,Gray, H., Villarreal, X., Kondri, M.E., Marti, D.N.,Llinás M., Schaller, J., Kramer, R.A., and Trail, P.A.,FASEB J., 1998, vol. 12, no. 15, pp. 1731–1738.
56. Zhou, Q.W., Xie, J.L., Xin, L., Ye, Q., Li, Z.P., andGan, R.B., Acta Biochim. Biophys. Sin., 2003, vol. 35,no. 8, pp. 761–767.
57. Dudani, A.K., Ben�Tchavtchavadze, M., Porter, S.,and Tackaberry, E., Biochem. Cell Biol., 2005, vol. 83,no. 1, pp. 28–35.
58. Chen, Y.H., Wu, H.L., Chen, C.K., Huang, Y.H.,Yang, B.C., and Wu, L.W., Biochem. Biophys. Res.Commun., 2003, vol. 310, no. 3, pp. 804–810.
59. Redlitz, A., Daum, G., and Sage, E.H., J. Vasc. Res.,1999, vol. 36, no. 1, pp. 28–34.
60. Gao, G., Li, Y., Gee, S., Dudley, A., Fant, J.,Crosson, C., and Ma, J.X., J. Biol. Chem., 2002,vol. 277, no. 11, pp. 9492–9497.
61. Doll, J.A. and Soff, G.A., in Cytokines and Cancer,Platanias, L.C., Ed., Springer Science + BusinessMedia, Inc., 2005, pp. 175–204.
62. Cao, Y. and Xue, L., Semin. Thromb. Hemost., 2004,vol. 30, no. 1, pp. 83–93.
63. Stathakis, P., Lay, A.J., Fitzgerald, M., Schlieker, C.,Matthias, L.J., and Hogg, P.J., J. Biol. Chem., 1999,vol. 274, no. 13, pp. 8910–8916.
64. Wang, H., Doll, J.A., Jiang, K., Cundiff, D.L., Czar�necki, J.S., Wilson, M., Ridge, K.M., and Soff, G.A.,Cancer Res., 2006, vol. 66, no. 14, pp. 7211–7215.
65. Tykhomyrov, A.A., Biopolymers Cell, 2012, vol. 28,no. 6, p. 413–423.
66. Cao, Y., Veitonmaki, N., Keough, K., Cheng, H.,Lee, L.S., and Zurakowski, D., Int. J. Mol. Med.,2000, vol. 5, no. 5, pp. 547–551.
67. Walter, J.J. and Sane, D.C., Arterioscler. Thromb. Vasc.Biol., 1999, vol. 19, no. 9, pp. 2041–2048.
68. Benelli, R., Morini, M., Brigati, C., Noonan, D.M.,and Albini, A., Int. J. Oncol., 2003, vol. 22, no. 1,pp. 87–91.
69. Peyruchaud, O., Serre, C.M., NicAmhlaoibh, R.,Fournier, P., and Clezardin, P., J. Biol. Chem., 2003,vol. 278, no. 46, pp. 45826–45832.
70. Weihrauch, D., Lohr, N.L., Mraovic, B.,Ludwig, L.M., Chilian, W.M., Pagel, P.S., Warltier, D.C.,and Kersten, J.R., Circulation, 2004, vol. 109, no. 19,pp. 2343–2348.

106
BIOCHEMISTRY (MOSCOW) SUPPLEMENT SERIES B: BIOMEDICAL CHEMISTRY Vol. 8 No. 2 2014
TYKHOMYROV et al.
71. Chang, P.C., Wu, H.L., Lin, H.C., Wang, K.C., andShi, G.Y., J. Thromb. Haemost., 2010, vol. 8, no. 1,pp. 194–201.
72. Chavakis, T., Athanasopoulos, A., Rhee, J.S.,Orlova, V., Schmidt�Wöll, T., Bierhaus, A., May, A.E.,Celik, I., Nawroth, P.P., and Preissner, K.T., Blood,2005, vol. 105, no. 3, pp. 1036–1043.
73. Bhadada, S.V., Goyal, B.R., and Patel, M.M., Fundam.Clin. Pharmacol. 2011, vol. 25, no. 1, pp. 29–47.
74. Danis, R.P., Ciulla, T.A., Criswell, M., and Pratt, L.,Expert. Opin. Pharmacother., 2001, vol. 2, no. 3,pp. 395–407.
75. Tahergorabi, Z. and Khazaei, M., Int. J. Prev. Med.,2012, vol. 3, no. 12, pp. 827–838.
76. Costa, P.Z. and Soares, R., Life Sci., 2013, vol. 92,no. 22, pp. 1037–1045.
77. Keck, P.J., Hauser, S.D., Krivi, G., Sanzo, K., War�ren, T., Feder, J., and Connolly, D.T., Science, 1989,vol. 246, no. 4935, pp. 1309–1312.
78. Miller, J.W., Adamis, A.P., and Aiello, L.P., DiabetesMetab. Rev., 1997, vol. 13, no. 1, pp. 37–50.
79. Murakami, T., Felinski, E.A., and Antonetti, D.A.,J. Biol. Chem., 2009, vol. 284, no. 13, pp. 21036–21046.
80. Kowluru, R.A. and Odenbach, S., Br. J. Ophthalmol.,2004, vol. 88, no. 10, pp. 1343–1347.
81. Twining, S.S., Wilson, P.M., and Ngamkitidechakul, C.,Biochem. J., 1999, vol. 339, no. 3, pp. 705–712.
82. Spranger, J., Hammes, H.P., Preissner, K.T.,Schatz, H., and Pfeiffer, A.F., Diabetologia, 2000,vol. 43, no. 11, pp. 1404–1407.
83. Lai, C.C., Wu, W.C., Chen, S.L., Xiao, X., Tsai, T.C.,Huan, S.J., Chen, T.L., Tsai, R.J., and Tsao, Y.P.,Invest. Ophthalmol. Vis. Sci., 2001, vol. 42, no. 1,pp. 2401–2407.
84. Sima, J., Zhang, S.X., Shao, C., Fant, J., and Ma, J.,FEBS Lett., 2004, vol. 564, nos. 1–2, pp. 19–23.
85. Cao, Y., Chen, A., An, S.S., Ji, R.W., Davidson, D.,and Llinás, M., J. Biol. Chem., 1997, vol. 272, no. 36,pp. 22924–22928.
86. Nguyen, T.M., Subramanian, I.V., Kelekar, A., andRamakrishnan, S., Blood, 2007, vol. 109, no. 11,pp. 4793–4802.
87. Bui Nguyen, T.M., Subramanian, I.V., Xiao, X.,Nguyen, P., and Ramakrishnan, S., Gene Ther., 2010,vol. 17, no. 5, pp. 606–615.
88. Zhang, S.X., Sima, J, Shao, C., Fant, J., Chen, Y.,Rohrer, B., Gao, G., and Ma, J.X., Diabetologia, 2004,vol. 47, no. 1, pp. 124–131.
89. Ma, J., Li, C., Shao, C., Gao, G., and Yang, X., Mol.Vis., 2012, vol. 18, pp. 330–336.
90. Izumi, Y., Kirby, C.O., Benz, A.M., Olney, J.W., andZorumski, C.F., Glia, 1999, vol. 25, no. 4, pp. 379–389.
91. Liu, X., Chen, H.H., and Zhang, L.W., Int. J. Ophthalmol.,2013, vol. 6, no. 2, pp. 221–227.
92. Bikbova, G., Oshitari, T., Tawada, A., and Yamamoto, S.,Curr. Diabetes Rev., 2012, vol. 8, no. 4, pp. 294–302.
93. Chang, J.H., Gabison, E.E., Kato, T., and Azar, D.T.,Curr. Opin. Ophthalmol., 2001, vol. 12, no. 4, pp. 242–249.
94. Warejcka, D.J., Vaughan, K.A., Bernstein, A.M., andTwining, S.S., Mol. Vis., 2005, vol. 11, pp. 859–868.
95. Kao, W.W., Kao, C.W., Kaufman, A.H., Kom�brinck, K.W., Converse, R.L., Good, W.V.,Bugge, T.H., and Degen, J.L., Invest. Ophthalmol. Vis.Sci., 1998, vol. 39, no. 3, pp. 502–508.
96. Drew, A.F., Schiman, H.L., Kombrinck, K.W.,Bugge, T.H., Degen, J.L., Kaufman, A.H., Invest.Ophthalmol. Vis. Sci., 2000, vol. 41, no. 1, pp. 67–72.
97. Kim, J.H., Kim, J.C., Shin, S.H., Chang, S.I.,Lee, H.S., and Chung, S.I., Exp. Mol. Med., 1999,vol. 31, no. 4, pp. 203–209.
98. Gabison, E., Chang, J.H., Hernández�Quintela, E.,Javier, J., Lu, P.C., Ye, H., Kure, T., Kato, T., andAzar, D.T., Exp. Eye Res., 2004, vol. 78, no. 3,pp. 579–589.
99. Fini, M.E., Cook, J.R., and Mohan, R., Arch. Dermatol.Res., 1998, vol. 290, pp. 12–23.
100. Fini, M.E., Girard, M.T., Matsubara, M., and Bar�tlett, J.D., Invest. Ophthalmol. Vis. Sci., 1995, vol. 36,no. 3, pp. 622–633.
101. Sack, R.A., Beaton, A.R., and Sathe, S., Curr. Eye.Res., 1999, vol. 18, no. 3, pp. 186–193.
102. Shumway, J.T. and Gambert, S.R., Int. Urol. Nephrol.,2002, vol. 34, no. 2, pp. 257–264.
103. Hohenstein, B., Hausknecht, B., Boehmer, K.,Riess, R., Brekken, R.A., and Hugo, C.P., Kidney Int.,2006, vol. 69, no. 9, pp. 1654–1661.
104. Chen, S., Jim, B., and Ziyadeh, F.N., Semin. Nephrol.,2003, vol. 23, no. 6, pp. 532–543.
105. Basile, D.P., Fredrich, K., Weihrauch, D., Hattan, N.,and Chilian, W.M., Am. J. Physiol. Renal. Physiol.,2004, vol. 286, no. 5, pp. 893–902.
106. Jiang, Z.Y., He, Z., King, B.L., Kuroki, T.,Opland, D.M., Suzuma, K., Suzuma, I., Ueki, K.,Kulkarni, R.N., Kahn, C.R., and King, G.L., J. Biol.Chem., 2003, vol. 278, no. 34, pp. 31964–31971.
107. Koshida, R., Ou, J., Matsunaga, T., Chilian, W.M.,Oldham, K.T., Ackerman, A.W., and Pritchard, K.A.,Circulation, 2003, vol. 107, no. 6, pp. 803–806.
108. Wada, J. and Makino, H., Clin. Sci., 2013, vol. 124,no. 3, pp. 139−152.
109. Kim, M.J. and Tam, F.W., Clin. Chim. Acta., 2011,vol. 412, nos. 23–24, pp. 2022–2030.
110. Mu, W., Long, D.A., Ouyang, X., Agarwal, A.,Cruz, P.E., Roncal, C.A., Nakagawa, T., Yu, X.,Hauswirth, W.W., and Johnson, R.J., Am. J. Physiol.Renal. Physiol., 2009, vol. 296, no. 1, pp. 145–152.
111. Asano, M., Yukita, A., Matsumoto, T., Kondo, S., andSuzuki, H., Cancer Res., 1995, vol. 55, no. 22,pp. 5296–5301.
112. Mima, A., Qi, W., and King, G.L., Semin. Nephrol.,2012, vol. 32, no. 5, pp. 471–478.
113. de Vriese, A.S., Tilton, R.G., Elger, M., Stephan, C.C.,Kriz, W., and Lameire, N.H., J. Am. Soc. Nephrol.,2001, vol. 12, no. 5, pp. 993–1000.
114. Gupta, K. and Zhang, J., Postgrad. Med. J., 2005,vol. 81, no. 954, pp. 236–242.
115. Abaci, A., O uzhan, A., Kahraman, S., Eryol, N.K.,Unal, S., Arinc,, H., and Ergin, A., Circulation, 1999,vol. 99, no. 17, pp. 2239–2242.
g
)

BIOCHEMISTRY (MOSCOW) SUPPLEMENT SERIES B: BIOMEDICAL CHEMISTRY Vol. 8 No. 2 2014
ANGIOSTATINS IN DIABETES 107
116. Starostin, I.V., Talitskii, K.A., Bulkina, O.S., and Kar�pov, Yu.A., Sakharnyi Diabet, 2013, vol. 1, pp. 19–26.
117. Abraham, D., Hofbauer, R., Schäfer, R., Blumer, R.,Paulus, P., Miksovsky, A., Traxler, H., Kocher, A., andAharinejad, S., Circ. Res., 2000, vol. 87, no. 8,pp. 644–647.
118. Chung, A.W., Hsiang, Y.N., Matzke, L.A.,McManus, B.M., van Breemen, C., and Okon, E.B.,Circ. Res., 2006, vol. 99, no. 2, pp. 140–148.
119. Boodhwani, M., Sodha, N.R., Mieno, S., Ramlawi, B.,Xu, S.H., Feng, J., Clements, R.T., Ruel, M., andSellke, F.W., J. Thorac. Cardiovasc. Surg., 2007,vol. 134, no. 6, pp. 1453–1460.
120. Uemura, S., Matsushita, H., Li, W., Glassford, A.J.,Asagami, T., Lee, K.H., Harrison, D.G., andTsao, P.S., Circ. Res., 2001, vol. 88, no. 12, pp. 1291–1298.
121. Sodha, N.R., Boodhwani, M., Clements, R.T.,Xu, S.H., Khabbaz, K.R., and Sellke, F.W., Arch.Surg., 2008, vol. 143, no. 5, pp. 463–470.
122. Sasso, F.C., Torella, D., Carbonara, O.,Ellison, G.M., Torella, M., Scardone, M., Marra, C.,Nasti, R., Marfella, R., Cozzolino, D., Indolfi, C.,Cotrufo, M., Torella, R., and Salvatore, T., J. Am. Coll.Cardiol., 2005, vol. 46, no. 5, pp. 827–834.
123. Boodhwani, M., Sodha, N.R., Mieno, S., Xu, S.H.,Feng, J., Ramlawi, B., Clements, R.T., andSellke, F.W., Circulation, 2007, vol. 116, no. 11,pp. 31–37.
124. Weihrauch, D., Lohr, N.L., Mraovic, B.,Ludwig, L.M., Chilian, W.M., Pagel, P.S.,Warltier, D.C., and Kersten, J.R., Circulation, 2004,vol. 109, no. 19, pp. 2343–2348.





![Review Article The Role of Transforming Growth Factor-Beta ...downloads.hindawi.com/archive/2014/180270.pdf · diabetic nephropathy [ ]. Cross-sectional studies in TD haveshownthatin](https://static.fdocument.pub/doc/165x107/5f819792314d424b39476304/review-article-the-role-of-transforming-growth-factor-beta-diabetic-nephropathy.jpg)