Tacroz
Transcript of Tacroz
-
8/14/2019 Tacroz
1/46
Management
of
Atopic Dermatitis:
Role of
Immunomodulators
-
8/14/2019 Tacroz
2/46
Atopic Dermatitis
Atopic dermatitis (AD) is a chronic, relapsing, inflammatoryskin condition associated with immunological dysfunction thatis characterized by an itchy red rashes.
Majority of the patients having a personal or family history ofatopic diathesis.
The most common skin disorder seen in infants and children.60% present in first year of life
It is a chronic skin disease with frequent episodes of remissionsand flare ups.
Atopic March: atopic dermatitisfood allergiesasthmaallegic rhinitis
-
8/14/2019 Tacroz
3/46
Epidemiology
Atopic eczema is common and the prevalence is increasing.
Arising trend in AD has been observed in India also in last fourdecades*.
AD was the commonest dermatoses in children constituting28.46% of pediatric patients.
* Kanwar AJ, De D. Epidemiology and clinical features of atopic dermatitis in India.Indian J Dermatol 2011;56:471-5
-
8/14/2019 Tacroz
4/46
Trigger factors Environmental irritants and allergens
Irritants, e.g. soaps and detergents (including shampoos, bubble baths,shower gels and washing-up liquids).
Skin infections: Staphylococcus aureus.
Contact allergens
Extremes of temperature and humidity. Most patients improve in summer
and are worse in winter. Sweating.
Abrasive fabrics, e.g. wool.
Dietary factors
Inhaled allergens, e.g. house dust mites, pollens, pet dander and moulds.
Endogenous factors
Stress
Hormonal changes in women - e.g. premenstrual flare-ups, deterioration inpregnancy.
-
8/14/2019 Tacroz
5/46
-
8/14/2019 Tacroz
6/46
Pathophysiology
Immune Dysfunction
-
8/14/2019 Tacroz
7/46
Pathophysiology
Defective epidermal barrier
Entry of allergens
in the skin
Normal Skin Skin of individual
predisposed to AD
Increased
desquamationof cells
In an individual genetically predisposed to AD, premature breakdown of
the corneodesmosomes leads to enhanced desquamation, analogous to
having rusty iron rods all the way down through the brick wall.
The brick wall starts falling apart and allows the penetration ofallergens thereby causing lesions ofAD.
-
8/14/2019 Tacroz
8/46
Reported Immunological Features ofAtopic Dermatitis
Increased IgE production
Specific IgE to multiple antigens
Increased basophil spontaneous histamine release
Decreased CD8 suppressor/cytotoxic number andfunction
Increased expression of CD 23 on mononuclear cells
Chronic macrophage activation with increased secretionof GM-CSF, PGE2 and IL-10
Expansion of IL-4 and IL-5 secreting Th 2-like cells
Decreased numbers of IFN-gamma-secreting Th 1-likecells
-
8/14/2019 Tacroz
9/46
Clinical Manifestations
Seen in early infancy, in 50 - 75% of cases,
age of onset is 6 months or younger
Clearance rate of 60% expected by age 16, relapses occurin adulthood
Worse prognosis
severe childhood disease
early onset
concomitant or family history of asthma/allergic rhinitis,biparental history of atopy
-
8/14/2019 Tacroz
10/46
Child with severe skin lesionsChild with mild eczema
Flexural involvement
-
8/14/2019 Tacroz
11/46
Infected eczema in an atopic child
Child with severe Pruritus andskin lesions
-
8/14/2019 Tacroz
12/46
Clinical Features
Three main age-related stages.
Infantile phase
Childhood phase
Adult phase
Dry skin and pruritus associated with all stages.
Skin barrier function decreased, may lead to increased
absorption of topically applied treatments.
Usually improves with adequate treatment
-
8/14/2019 Tacroz
13/46
Clinical Phases
Infantile Phase ( 0-2 years )
Onset around 3 months of age.
Under 6 months, the face and scalp commonly involved,
at an older age, limb folds and hands involved
Red, scaly, crusted weeping patches withexcoriations seen on both cheeks and extensorsurfaces of extremities
Course chronically relapsing and remitting
-
8/14/2019 Tacroz
14/46
Clinical Phases (contd)
2 Childhood Phase ( 2-12 years ) Papular areas in flexural regions common.
Persistent rubbing and scratching leads tolichenified plaques and excoriations
3 Adult Phase (puberty onwards) Flexural lichenified eczema with facial
involvement in periorbital regions seen.Upper trunk, shoulders, scalp affected with
chronic remissions and exacerbations
-
8/14/2019 Tacroz
15/46
Diagnosis of Atopic Dermatitis
This requires the presence of three or more majorand three or more minor criteria as defined byHanifin and Rajka
Major criteria 1.pruritus
2.typical morhology and distribution
3.chronicity
4.family history of atopy
-
8/14/2019 Tacroz
16/46
-
8/14/2019 Tacroz
17/46
Morbidity
Impact on quality of life occurs at all ages.
Psychological problems from visible skin
lesions due to stigmatization Itch-scratch cycle
Sleeplessness, lack of concentration at schoolor work
Repeated treatments, time involved,financial costs
-
8/14/2019 Tacroz
18/46
Management
Hydrate with tub soaks and moisturizers
Control inflammation with topical corticosteroids
Reduce flare and control disease withimmunomodulators
Treat secondary bacterial infections with topical andsystemic antibiotics
Manage pruritis with antihistamines
UVA and UVB phototherapy
-
8/14/2019 Tacroz
19/46
Management of Atopic Dermatitis
No single, ideal treatment available
Each patient should have a flexible plan tailored fortheir need
Dietary history important, dietary manipulationcontroversial
Family education important
Reduce exposure to allergens
-
8/14/2019 Tacroz
20/46
General Treatment Guidelines
Moisturizers are the
cornerstone of therapy in AD
Frequent use important because AD is oftenaccompanied by dry skin.
Creams, ointments or lotions can be used dependingon individual needs
Avoidance of drying bathing products
Itch control Distressing symptom, use oralantihistamines, try to break the itch-scratch cycle
-
8/14/2019 Tacroz
21/46
General Treatment Guidelines(contd.)
Control of infection
Patients with extensive AD are often colonized withStaph. aureus.
A course of oral antibiotics topical antibioticsneeded for lichenified, excoriated lesions notresponding to treatment.
Viral infections, eg. warts, eczema herpeticum areseen in these patients.
-
8/14/2019 Tacroz
22/46
Selection of treatment
This depends on -
Disease severity
Age Compliance
Efficacy
Safety data
Treatment costs
-
8/14/2019 Tacroz
23/46
Rx Treatment Options
1. Topical corticosteroids
2. Topical immunosuppressants
3. Systemic corticosteroids
Off-Label and other treatment options
1. Photochemotherapy
2. Cyclosporin
3. Azathioprine
4. Thymopentin
5. Interferon-therapy6. Traditional Chinese medicine
7. -linoleic acid
-
8/14/2019 Tacroz
24/46
Topical corticosteroids (TCS)
First introduced in the 1950s and are currentlythe mainstay of prescription therapy for atopicdermatitis
Safe and effective when used as recommended
Weakest steroid that will keep the eczema undercontrol should be used
Potent steroids should be used in short pulses,generally 2-3 weeks
-
8/14/2019 Tacroz
25/46
Factors to consider when prescribingtopical corticosteroids
1. Type of preparation (base and potency)
Base can be ointment, cream, emulsion, gel or lotion
Potency classified from group I (most potent) to VII(least potent)
2. Acute or chronic eczema
3. Age of child
4. Site to be treated
5. Extent of eczema
6. Method of application
-
8/14/2019 Tacroz
26/46
Mechanism of action of TCS
1. Antiinflammatory effects
TCS affect inflammatory cells, chemical mediators and tissueresponses which are all responsible for cutaneous inflammation
2. Antiproliferative effects
TCS may reduce mitotic activity in the epidermis, leading toflattening of the basal cell layer and thinning of the stratumcorneum and stratum granulosum
3. Atrophogenic Effects
TCS can promote atrophy of the dermis through inhibition offibroblast proliferation, migration, chemotaxis and proteinsynthesis
-
8/14/2019 Tacroz
27/46
Cutaneousor local adverse effects
may include:
Atrophic changes
Easy bruisability
Increased fragility
Purpura
Stellate pseudoscarsSteroid atrophy
Striae
Telangiectasis
Ulceration
Topical corticosteroids may increase
therisk for infections, including:
Aggravation of cutaneous infection
Granuloma gluteale infantum
Masked infection (tinea incognito)
Secondary infections
Adverse Effect of Topical Corticosteroid
Note: It is difficult to quantify the incidence of
side effects caused by topical corticosteroids
as a whole, given their differences in potency
-
8/14/2019 Tacroz
28/46
Contact dermatitis
Delayed wound healing
Hyperpigmentation
Hypertrichosis (hirsutism)
Hypopigmentation
Perioral dermatitis
Photosensitization
Miscellaneous adverse effects of topical corticosteroids
Hypothalamic-pituitary-adrenal suppression
Glaucoma
Septic necrosis of the femoral head
Hyperglycemia
Hypertension
Topically applied high and ultra-high potency corticosteroids can be
absorbed well enough to cause systemic side effects such as:
-
8/14/2019 Tacroz
29/46
Risk factors for systemic adverseeffects
Young age (infants and children)
Liver and renal disease
Amount of TCS applied
Extent of skin disease treated Frequency of application
Length of treatment
Potency of drug
Use of occlusionIt is not established whether catch up growth in children will
occur when TCS are discontinued.
-
8/14/2019 Tacroz
30/46
Topical Immunosuppressants
Newest pharmacological class for AD
Introduced in this decade
Direct immunosuppressive action in diseases withimmunologic basis
2 FDA approved products
Tacrolimus (FK506)
Pimecrolimus (SDZ ASM 981)
-
8/14/2019 Tacroz
31/46
Background
Tacrolimus ointment approved on 12/08/2000,0.03% ointment approved for children 2 to 15 years,0.1% ointment approved for adults.
Indication in both age groups is short andintermittent long term therapy of patients withmoderate to severe AD.
Systemic tacrolimus first introduced for preventionof allograft rejection, now used in kidney, liver andheart transplantation
-
8/14/2019 Tacroz
32/46
Pimecrolimus cream 1% approved on 12/13/2001
Indicated for patients 2 years of age and older forshort and intermittent long term therapy in thetreatment of mild to moderate atopic dermatitis
Both drugs not approved for use in children lessthan 2 years of age
Background (contd)
-
8/14/2019 Tacroz
33/46
-
8/14/2019 Tacroz
34/46
Mechanism of Action
Calcineurin = Enzyme with phosphotase activity causes dephosphoralation
Calmodulin = Intracellular protein that combines with calcium & activates variety of cellularprocesses
-
8/14/2019 Tacroz
35/46
IMMUNOMODULATORS INATOPIC TREATMENT
Decrease atopic flare by:
Decrease pruritus
Decrease use of topical steroids
Low systemic absorption
Burning and warmth most frequent adverseevent
-
8/14/2019 Tacroz
36/46
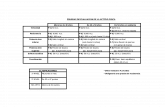
MINIMAL SYSTEMIC ABSORPTION
%
12 week randomized double-blind multicenter trials
-
8/14/2019 Tacroz
37/46
Indication
Short-term & intermittent long-term therapy in
moderate to severe AD
Dosage
0.03% in children aged 2-15 years twice daily
0.03% and 0.1% in adults twice daily
-
8/14/2019 Tacroz
38/46
Adverse Events
Most common were sensation of skin burning & pruritus at
application sites, prevalence decreased after first 4 days.
Flu-like symptoms, Allergic reactions, Skin erythema, Headache,Skin infection, Folliculitis, Rash, Skin tingling, Acne &
hyperaesthesia may occur rarely.
-
8/14/2019 Tacroz
39/46
Proven Safety Profile in 3 years ofPediatric Clinical Trials
Gentle for children, even on head neck, intertriginous areas& large body surface areas.
Studied in >6000 pediatric patients.
No immunosuppression or effect on immune parameters.
No skin atropy or growth retardation.
-
8/14/2019 Tacroz
40/46
Precautions
In treatment of infected AD. Before commencing treatmentwith tacrolimus ointment, clinical infections at treatmentsites should be cleared
Treatment may be associated with an increased risk of viralinfections.
In presence of these infections, balance of risks & benefits
associated should be evaluated.
-
8/14/2019 Tacroz
41/46
* MF Rehaman et al.2008
-
8/14/2019 Tacroz
42/46
* Breuer K et al. 2005
-
8/14/2019 Tacroz
43/46
* Hanifin et al. 2005
-
8/14/2019 Tacroz
44/46
Salient Features
Rapid onset of action
Minimal systemic absorption
Safe & efficacious application to head/neck region
Few adverse effects
Safety & efficacy of tacrolimus ointmentmonotherapy has been demonstrated for periodsof upto 2 year in adults & children.
-
8/14/2019 Tacroz
45/46
Salient Features contd
Does not interfere with (or decrease) collagensynthesis or cause skin atrophy.
Associated with a reduction in staphylococcal skincolonization in AD lesions.
Demonstrated antifungal activity against strains ofMalessezia furfur, a possible allergen.
-
8/14/2019 Tacroz
46/46