Rehab.anak
Transcript of Rehab.anak

REHABILITASI MEDIK ANAK

REHABILITASI MEDIKIS A PHYISICAL MEDICINE AND REHABILITATION SCIENCE
ILMU KEDOKTERAN FISIK DAN REHABILITASI ( IKF&R)
SEJARAH REHABILITASI MEDIK DIMULAI SAAT PENGGUNAAN BAHAN FISIK UNTUK PENGOBATAN PADA MASA LALU.
HYDROTHERAPY TELAH DIKEMBANGKAN SEJAK KAKISRAN ROMAWI
PADA ABAD IX DAN X MASA PENGGUNAAN GALVANIC AND PARADIC
1890 : PENGGUNAAN GELOMBANG ELEKTROMAGNETIK FREKUENSI TINGGI ( DIATHERMIA ) OLEH d’ ARSONVAL DI FRANCIS UNTUK TUJUAN PENGOBATAN

REHABILITASI ANAK Secara khusus dalam penilaian dan
penanganan bayi, anak dan dewasa muda dengan berbagai jenis
“ developmental disabilities”
The disabilities may include cerebral palsy, muscular dystrophy, or spina bifida.

Disability / disabilitas ???
interaksi yang komplek antara individu terhadap lingkungannya
word health organisation (WHO )

Impairment disfungsi fisiologis
Disabilitas
perawatan diri dan mobilitas fungsional dalam suatu lingkungan
Handikap
Pilihan peran sosial, bekerja, sekolah, berkeluarga,gaya hidup, rekreasi
Impairment disfungsi fisiologis
Aktivitas
perawatan diri dan mobilitas fungsional dalam suatu lingkungan
Partisipasi
Pilihan peran sosial, bekerja, sekolah, berkeluarga,gaya hidup, rekreasi

Definisi WHO
Impairmen suatu kondisi abnormal dari struktur atau fungsi
“ disfungsi fisiologis “
Aktivitas adalah melaksanakan tugas atau aksi oleh seorang individu cerminan dari sudut pandang individu tsb. Contoh kemampuan untuk melakukan pemenuhan perawatan diri
“ keterbatasan beraktivitas = disabilitas
Partisipasi tergantung pada keterlibatan sorang individu dalam situasi kehidupan dan cerminan dari sudut pandang sosialnya
Keterbatasan partisipasi = handikap atau ketidak mampuan untuk dalam menggunakan peran sosial normal

KEDOKTERAN FISIK DAN REHABILITASI MEDIK
KEDOKTERAN FISIK : CARA INTERVENSI UNTUK MEMPERBAIKI FISIOLOGI MENTAL DAN FUNGSIONAL
REHABILITASI MEDIK : MEMUNGKINKAN MASYARAKAT UNTUK BERPARTISIPASI AKTIF DALAM LINGKUNGAN SOSIAL

“ Khusus terhadap anak – anak di titik beratkan pada
1. Mengerti terhadap proses komplek perkembangan bayi, anak, adolesen, dewasa muda dan keluarganya dalam pengertian komunitas .
2. Mengerti peran biologis, psikologis dan sosial dalam perkembangan emosi, sosial, motoris, bahasa dan kognitif
3. Mekanisme dari pencegahan primer dan sekunder terhadap kelainan dalam prilaku dan perkembangan
4. Mengindentifikasi dan menangani terhadap gangguan dari lingkungan dan perkembangan sepanjang anak- anak dan dewasa “
Source: Accreditation Council for Graduate Medical Education(ACGME)

Understanding the complex
developmental processesIn the first few months of life some children need help
learning to roll, sit, crawl and walk. The earlier a developmental delay is detected, the better the outcome
will be with therapy .
Some major milestones: Rolling: 4-6 months Sitting: 6-8 months Crawling: 7-10 months Walking: 12-15 months Running: 24-28 months Jumping: 26-30 months

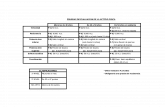
CATEGORY REFLEX APPEARS INTEGRATED BY
NEONATAL
POSTURAL
RIGHTING AND
PROTECTIVE
MORO
GALANT
CROSSED EXTENSOR
FLEXOR WITHDRAWAL
EXTENSOR THRUST
REFLEX WALKING
PALMAR GRASP
PLANTAR GRASP
TONIC LABYRINTHINE
ATNR
STNR
POSITIVE SUPPORTING
NECK
LABYRINTHINE
OPTICAL
BODY ON BODY
BODY ON HEAD
PROTECTIVE EXTENSION - FORWARD
- SIDEWAYS
-BACKWARD
LANDAU
EQUILIBRIUM - PRONE
- SUPINE AND SITTING
- ALL – FOUR
- STANDING
BIRTH
BIRTH
BIRTH
BIRTH
BIRTH
BIRTH
BIRTH
BIRTH
BIRTH
2 MONTTH
4 – 6 MONTH
BIRTH
BIRTH
2 MONTH
7 – 12 MONTH
6 – 9 MONTH
8 MONTH
10 MONTH
3 – 6 MONTH
6 MONTH
7 – 8 MONTH
9 – 12 MONTH
12 – 21 MONTH
6 MONTH
2 MONTH
1 – 2 MONTH
1 – 2 MONTH
1 – 2 MONTH
6 MONTH
6 MONTH
9 MONTH
6 MONTH
4 MONTH
10 MONTH
2 MONTH
4 – 6 MONT
LIFE LONG
LIFE LONG
LIFE LONG
5 YEARS
LIFE LONG
LIFE LONG
LIFE LONG
1 – 2 YEARS
LIFE LONG
LIFE LONG
LIFE LONG
LIFE LONG
REFLEX DEVELOPMENT 0 - 5 YEARS



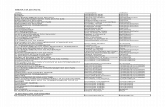
AGE SKILL
2 MONTH
4 MONTH
5 MONTH
6 MONTH
7 MONTH
LIFTS HEAD IN PRONE
LIFTS HEAD IN PRONE , WEIGHT ON FOREARMS
BRINGS HANDS TO MIDLINE
HEAD KEPT IN LINE WITH TRUNK WHEN PULLED TO DITTING
LIFT HEAD IN SUPINE
LIFT BOTTOM IN SUPINE –” BRIGES ‘
ROLL TO SIDE
TAKE BOTH FEET TO MOUTH
HELPS PULL SELF TO SITTING
SITS WITH HANDS IN FRONT FOR SUPPORT
ROLLS SUPINE TO PRONE
TAKES BOTH FEET TO MOUTH
HELPS PULL SELF TO SITTING
PIVOTS AND PUSHES SELF BACKWARDS IN PRONE
DEVELOPMENT 0 - 12 MONTH

SUMBER : PHYSICAL THERAPY FOR CHILDREN ( PAMELA ARGARET )
AGE SKILL
8 MONTH
8 – 10 MONTH
10 – 12 MONTH
12 MONTH
CREEPS FORWARDS ON FOREARMS
SITS UNSUPPORTED WITH STRAIGHT BACK
CAN REACH IN SITTING
CAN GET INTO LYING
CRAWLS ON ALL FOURS
PULLS TO STANDING
GETS DOWN FROM S TANDING
WALKS WITH BOTH OR ONE HAND HELD
SOME CHILDREN WALK INDEPENDENTLY

Specific Examples: Development
Developmental Delay Cognitive Disabilities Motor Disabilities
Examples: cerebral palsy, spina bifida
Chromosomal/Genetic Disorders Examples: Down Syndrome, Fragile X
Autism Spectrum Disorders Neonatal Intensive Care Unit follow-up

COGNITIVE
DEVELOPMENT
Physical
Development
Cultural
influence
Social emotional
DevelopmentPerson

PEDIATRIC REHABILITATION
HABILITATIONCongenital
Cerebral palsy
Chilhood aphasia Developmental delay
REHABILITATION Acquired Disorder
Brain injury Spinalcord injury
THE APROACHMENT Comprenhensive evaluation Identification of specific area of deficit development of threatment plan based on development level, age of child and outcome expectation Implementation of a threatment plan as appropriate discharge planing

Assesment The functional balance
Score : • + : can without helped• + : can with helped• - : cannot
The examination point: From lying to sit down From sit down to stand up Standing with support Standing Standing with right foot Standing with left foot squat

The Examination Musculosceletal condition
MMT ROM Antopometri Scoliosis Test Club Foot Test Trandelenburg Test Gait test

Double support
(10%)
Loading response
10%
Stance (60%)
30%
Double support
(10%)
Midstance Terminal stance
Preswing
50% Toe off
Initial swing
70%
Midswing Terminal swing
85%
Swing (40%
One complete gait cycle

GAIT COMPONENT
Initial contact Loading response Midstance Terminal stance Preswing Initial swing mid swing Terminal swing

FUNCTIONAL EXAMINIATION / GROWTH & DEVELOPMENT
DENVER DEVELOPMENTAL TEST ( DDST )
- SOCIAL PERSONAL
- FINE MOTOR ADAPTIVE
- LANGUAGE
- GROSS MOTOR
INTELLIGENCE EXAMINATION
The good IQ grade is ease the EXERCISE

MEDICAL REHABILITATION DIAGNOSTIC
( IMPAIRMENT, DISABILITY HANDICAPS )
functional disorder
APROACH PROBLEM ORIENTED
R1. MOBILISATION
R2. ADL
R3.COMUNICATION
R4.PSYCHOLOGY
R5.SOCIAL
R6.VOCATIONAL
R7.ETC

ICF ( WHO 2002)( International Clasification of Function )
Structure of body fanction
Physiological dysfunction ( Erb’s Palsy : parese Flexus brachialis )
Activity ( Graps disorder )
Particifation ( can’t plays )

MEDICAL REHABILITATION PROGRAM
“ REALISTIC GOAL “
A. PHYSIOTHERAPY / Physical Therapy
- With Modality
- Exercise
B. Ocupational therapy
C. Orthotic - Prostetic
D. SPEECH THERAPY

Physical Therapy
Physical Therapy (PT) specializes in the assessment and management of infants, children and adults with a variety of developmental disabilities. The disabilities may include
cerebral palsy, muscular dystrophy, or spina bifida.What Is Occupational Therapy?...
Technically, it is defined by the American Occupational Therapy Association executive board
(1976) as: "The therapeutic use of work, self-care, and play activities to increase development and prevent disability. It may include adaptation of task or
environment to achieve maximum independence and to enhance the quality of life."

The Goal Of Occupational Therapy (OT )Occupational Therapy has the same goal in mind
(increasing function and independence) in regards to physical disabilities and limitations, and we may use
repetitive exercises, but most often we use them in the context of a "functional activity". This refers to
performing meaningful activities while simultaneously working on increasing function and mobility.
For example, suppose we have a patient with limitations in upper extremity strength and range of motion. A
Physical Therapist may have a patient doing an arm exercise bike or repetitively lifting weights over their head (using heavier weights as the patient tolerates). This HAS
it's place and definite purpose in rehab!

PHYSIOTHERAPY
THERAPY EXERCISE TRADITIONAL MODE- Strengthening- ROM ( Range Of
Movement ) - Endurance - Compensation- Game


THE PRINCPLE Doing activity that funny but the purposes is to doing therapy
For Example With game activity direct the fine motor movement ( skil hand movement , Coordination hand movement , Coordination eye
movement , centrum attention )
Many kind of puzzle dll

Activities that promote the development of gross motor skill
Playground equipment •Endurance activities •Swimming •Ball Toss •Kick Ball •Jump Rope, Skipping, galloping, hopping •Playing outside •Imitating animals •Wheelbarrow walking •"Simon Says" •Log Rolling •Riding bicycles •General exercises •Walking a line, curb, railroad ties

SPEECH PATOLOGY( SPEECH THERAPY )
COMUNICATION PROBLEM Language disorder Voice production disorder because neurogenic disorder and organ
disorder had role in Voice production Sensory disorder ( Auditory )

Orthotic – Prosthetic Orthotic
The porpuse is to support , function , adaptation
Prosthetic - ( protese )




8. PROGNOSIS - MEDICAL ( ACCORDING WITH MEDICAL DIAGNOSTIC ) - FUNCTIONAL ( MOBILITATION, PERSONAL ADL, INSTRUMENT ADL, EDUCATION )
9. FOLLOW UP / EVALUATION / DISEASE RECOVERY, NEUROLOGICAL RECOVERY ,
FUNCTIONAL RECOVERY
DISEASE – IMPAIRMENT – DISABILITY - HANDICAP




CNS PROBLEM / CEREBRAL PALSY
BRACHIAL PALSY MUSCULAR DISTROPY SCOLIOSIS TORTICOLIS CTEV FLAT FEET DEFISIENSI EXTREMITY AUTISM SPECTRUM SPINAL MUSCULAR
ATROPI FRAKTUR EKSTREMITAS DOWN SYNDROME
JUVENIL RA POLIOMYELITIS, SINDROMA
GUILLAINBARE,MIELITIS TRANSVERSA SPINALCORD INJURY
NEURITIS TRAUMATIC PARALISIS PERIODIK
POT DISEASE
DEVELOPMENTAL
DELAYED
SPEECH DELAYED
MOTOR DELAYED

CEREBRAL PALSY




REHABILITATION OF C.P
Principles of proper rehabilitation :1. Proper evaluation ( individual treatment ) - to plan a therapy program.to assess progress. - to add observation to the diagnostic picture.2. Early treatment( increasing functional deficits w/ age
as secondary effects of spasticity &other primary problems
3. Team work ( global dysfunction )

(A) Clinical evaluation
1. Functional : Postural control Mobility
Primitive reflexes Motor exam
2. Swallowing & dysphagia
3. Communication: Speech/ language Visual
Auditory Mentality
4. Chest 5. Urinary bladder 6. Bowel
7. Self -care activities (ADL) 8. psychosocial
EVALUATION OF CP CHILD

SCOPE OF CP REHAB. 1. Neurodevelopmental training. 2. Motor facilitation approach. 3. Treatment of spasticity. 4. Rehab. of swallowing problems. 5. Rehab. of speech problems. 6. Rehab. of auditory problems. 7. Rehab. of visual problems. 8. Rehab. of chest problems. 9. Rehab. of urinary bladder & bowel problems.10.Rehab. Of ADL & 11.Psychosocial rehab.

ASSESSMENT OF MILESTONES & POSTURAL CONTROL
Understanding normal development allows to adaptive equipment to assist child in gaining increase the interaction with the environment.
Sitting balance at age 2 yrs. is an indicator of future walking. Observe how much parental support given to child.
child own ability in postural stabilization.
collapse on one side of his body, twist to one side, tilt & turn to one side.

EVALUATION OF PRIMITIVE REFLEXES
Can be used as indicator of ambulation Abnormal response for two of the following seven reflexes by age 12
month has a poor prognosis for walking this are Should be absent Should be present ATNR parachute reaction STNR foot placement Moro response Neck righting reflex Extensory thrust Presence of Moro or ATNR, seizures, ability to sit at 12 month
indicate ambulation by age of 6 yrs.

MOTOR EXAMINATIONGAIT
Hemiplegia Toe walk
Diplegia Bilateral equinovaras,
Knee flexed & in valgus
Scissoring
Cerebellar Ataxic
DEFORMITIES
Hemiplegia : adducted arm, flexed
elbow, wrist & fingers equinus foot.Diplegia: adducted hip, flexed knee
in valgus, bilateral EV knee height
discrepancy indicates hip dislocation.Quadriplegia: combination scoliosis &
hyperlordosis in spastic CP
kyphoscoliosis in hypotonic CP

MOTOR EXAMINATIONR.O.M.
Degree by goniometry: Limited (= fixed deformity =
ms. Contracture) Not limited (+ deformity =
threatening deformity
= muscles imbalance)
ABNORMAL MOVEMENT Dystonia, ( cervical =
spasmodic torticollis ) Chorea & Athetosis Tremors
MUSCLE TONESpasticity ( = clasp knife ): - generalized or focal - grade 0 (non) - 4 (severe) [Ashworth scale]Rigidity ( = lead pipe ) Hypotonia ( cerebellar )Combination : the predominant symptoms will contribute to diagnostic type referred for treatment

MOTOR EXAMINATIONMUSCLE STRENGTH
Grade 0 = No contraction detected1 = Flicker of contraction w/ no
movement.2 = Joint movement possible only with gravity eliminated.3 = Muscle contraction possible against
gravity without resistance.4= Muscle contraction against gravity & less than normal amount of
resistance.5 = Normal power against gravity and
resistance.
MUSCLE STRENGTHValues of muscles grading: - To determine ambulation with or without brace ( grade 3 antigravity muscles can ambulate without brace - Topographic classification for treatment plan ( strengthening exercise for weak muscles ) - Ex. must be low grade and non-fatiguing in ms.<3/5 -N.B (I) grade drops form muscle power following tendon lengthening.

SWALLOWING STUDY Values: - To facilitate appropriate position for safe, effective feeding - To increase ability to self feed. Methods: 1. Video fluoroscopic swallowing study - Requires speech - pathologist & radiologist - Patient is given liquid & various consistency of solid food impregnated w/ baruim & folowed by X-ray until be sure safe effective swallowing 2.Fiberoptic evaluation of swallowing ( FEES ) Transnasal endoscopy of hypopharynx to observe foodway & airway before & after( but not during ) the moment of swallowing. 3. EMG, manometry, scintigraphy & U.S: less commonly use.

Assessment of speechSpeech problems : Dysarthria (oral motor control problems ) :
Spastic
Hypokinetic (ataxic )
Hyperkinetic (dystonia,chorea) Aphasia Language delay (brain pathology, MR, hearing
impairment )

VISUAL ASSESSMENT
Problems: Strabismus ( imbalance in eye ms. )
Hemianopsia(in dense hemiplegi w/ MCA occlusion)
Blindness ( anoxic cortical vision loss ) Effects: 1. More motor delay 2. Language delay
3. Abnormal movements ( blindism )
4. More delayed postural mechanism
especially hypotonic CP

AUDIOLOGICAL EVALUATION Must be early so that important speech development period not
lost.
In infant (1-2 d. of birth): Brain stem auditory evoked response (BAER): Electrodes placed on the child & presenting a stimulus picked up from a computerized system.
A specific wave form response is recorded from the brain stem if stimulus is heard.
Otoacoustic emission testing (OAE): Echo from hair cell of normally functioning cochlea picked by a microphone placed in the middle ear & connected to micro computer.(middle ear pathology is ruled out)

NEURODEVELOPMENTAL TRAININGEQUIPMENT TRAINING
Criteria for selection: 1. to carry out tasks otherwise
impossible with his ability.2. appropriate support to participate
in social & educational activities .
3. good alignment & correction of abnormal postures
4. adjust for child” growth, removal of support with increasing ability.
5. modification for different children in schools & clinics
6. provide additional motor experience in different posture
7. Comfort and protect joints & skin.
Equipments varieties: 1. Wedges: Abductor W : prevent adduction deformities 2. Trumble form wedges & trumbles. 3. Large inflatable ball set 4.Crawlers: -platforms on wheels or wedges on wheels -A canavas sling under child” abdomen & supports on casters, straps to hold thighs in flexion. 5. Sitters

NEURODEVELOPMENTAL TRAINING
6. Apparatus for supporting standinga) Prone or supine standers to encourage
weight bearing & standingb) Standing frames adjusting correct
alignment: -checked for height so that child does not
grasp them w/ abnormal shoulder hunching , excessive elbow flexion &
radial deviation of wrist. -supplied w/ strapping to correct flexed hip
& knees -feet held at right angles by a board &/or
foot place.c) Parallel bars
d) Mirrorse) Stairs with bannisters: very in height. f) Rumps, uneven ground, various floor
services for gait training.
7.Walking aids Walkers Crutches Braces & Calipers: Knee gaiters (polyethylene knee moulds) to keep knee straight abduction parts to keep legs apart. Elbow gaiters which keep elbow straight for correct arm push & grasp of walkers.

MOTOR FACILITATION APPROACH
1. Bobath Method: inhibition of abnormal tone & posture of released postural reflex while facilitating specific automatic motor response (by special technique of handling) resulting in performance of skilled voluntary movements.
2. Rood Method: Use of peripheral input of cutaneous sensory stimuli (brushing, tapping, icing, heating, pressure, ms. stretch, muscle contraction, joint approximation. or retraction)
Various nerves & sensory receptors are described & classified into types ,location, effect, response, indication.

MOTOR FACILITATION APPROACH
3. Propioceptive Neuromuscular facilitation (Kabat & Knott)
Use of such mechanisms as maximum resistance , quick stretch & spiral diagonal (mass) movements, sensory afferent stimuli (touch, pressure, traction,compression & visual) to facilitate normal mov .
[special techniques: irradiation. stim. of reflexes,reversal(successive induction), relaxation.].
4. Brunstrom Method ( hemiplegia): Produces motion by provoking primitive movement pattern or synergitic pattern as follows :
-Reflex response used initially & later voluntary control
-Control of head & trunk by stim. of TNR, tonic labrinythine R
-Associated reaction : hyperextension of the thumb produces relaxation of finger flexors.

MOTOR FACILITATION APPROACH
5. Motor relearning program of Carr & Shepherd: functional training, practice, repitition, in the performance of tasks &
carry over those motor skills into functional activities.
6. Forced use paradigm (= constraint - induced movements therapy CIMT):
Non hemiplegic limb is restrained in a sling during 90% of waking hrs. to force the patient to use the hemiplegic limb.
The minimum amount of motion in the paretic limb before being enrolled into CIMT protocol is 20 of wrist extension and 10 of extension of 2 fingers at MCP or IPJ.

TREATMENT OF SPASTICITY
Positioning Avoid prolong sitting (less hip & hamstring flexion ) Prone lying at night (less hip flexion ) Abduction wedge at night & in wheelchair (less hip
adduction) AFO splint Standing frame Molded thoracolumbar orthosis for early scoliosis or
kyphosis Total contact support incorporated into a contoured
seating system

Drugs Indication : generalised spacticity to aid in mobility
Types :1. Dantrolene Sodium (Dantrium):
Inhibits Ca release in excitation-contraction coupling
Used in cerebral form of spacticity Dose: 25- 200mg
2. Baclofen (Lioresal ) [ presynaptic inhibition ]
Used in spinal form of spasticity Dose :5-40mg
3. Diazepam (Valium) [postsynaptic inhibition]
Used in spinal form of spasticity Dose :2-30mg
TREATMENT OF SPASTICITY

TREATMENT OF SPASTICITYPHYSIOTHERAPY
PHYSICAL AGENTS
Aim: a. Analgesia b. Ms. Relaxation c. Collagen extensibility
Modalities: 1) Ice 20mins.
2) Heat: Superficial : Dry: I.R. Moist: hot packs
Deep : S.W. U.S
ELECTRIC CURRENTS Aim: Ms. strengthening (galvanic & faradic) .
Analgesia ( TENS, IF)
EXERCISES For spasticity : Passive ROM Stretch (short ms.)
Strengthening (weak ms., antagonist),
resistive > 3/5
For hypotonia : Strengthening ( weak ms) Balance
For athetosis : Training to control simple joint motion

TREATMENT OF SPASTICITY
Nerve/ Motor Point Block
Indications Localized spasticity poorly responsive to drugs or PT, interfering w/ mobility, bracing, hygiene & causing pain Contraindication: - Absolute: Allergy Infection Pregnancy - Relative: Coagulopathy Problems: -Loss of motor function of injected ms. -Return of spasticity ( axon sprouting )

TREATMENT OF SPASTICITY
SERIAL CASTINGIndications: focal contracture (especially elbows,
knees, ankles ). Method: Limb is stretched then casted in a lengthened position ( can be combined with blocks ) Changed every few days or weeks to gradually stretch contracted structures.

TREATMENT OF SPASTICITYBRACES ( = CALIPERS = ORTHOSIS )
Aim: To correct deformity To control athetosis To obtain upright position
Types: AFO: For ankle instability w adequate Q > 3/5 Types: solid ( in ankle clonus ) Klenzak ankle joint w/spring(A,P) w/ stop (A,P) Accessories: varus strap valgus strap KAFO: For correction of knee deform. & instab. HKAFO: For ambulation w/ hip instability . Shoe modification

REHAB OF SWALLOWING PROBLEMS
Team: speech language specialist, OT, Dietary specialist. Items: Changes in posture & head position during feeding. Oral motor exercise for the tongue & lips to increase
strength, ROM, velocity, percision. Use of thickened fluid & soft food in small boluse Use of alternative feeding routes e.g. nasogastric tube,
gastrotomy or jejunostomy tubes with severe aspiration or caloric need.

REHAB OF SPEECH PROBLEMS
Team : speech -language pathologist & nurse Items : 1- oral option : electrolarynx
2 - non oral options :
- simple hand writing
- gestures
- augmentative communication
device (simple alphabet & picture board
to sophosticated computer systems
3- treatment of hearing & visual problems

REHAB OF ADL
Team : occupational therapist Items :
- provision of self help devices
- training in activities of ADL
- provision of creative interest
- training in suitable work

PSYCHOSOCIAL REHAB
Team : psychiatrist + social specialist Items : - provision of recreational activities
e.g.- special olympics, athletic competition
- horse back riding programs
(recreational & therapeutic )
- computers ( for schools & recreation

Muscular Dystrophy

DefinitionRefers to a group of hereditary progressive diseases. Muscular Dystrophy affects muscular strength and action, some of which first become obvious in infancy, and others which develop in adolescence or young adulthood. The syndromes are marked by either generalized or localized muscle weakness, difficulties with walking or maintaining posture, muscle spasms, and in some instances, neurological, behavioral, cardiac, or other functional limitations.

Nursing Diagnosis
Impaired mobility, activity intolerance, risk for injury, risk for aspiration, risk for impaired skin integrity, self-care deficit, knowledge deficit, caregiver role strain, low self-esteem, social isolation, disturbed body image, and hopeless to name a few.

Nursing Implications and interventions:
Multidisciplinary. Care for these patients involves arranging for consultations with physical therapy, occupational therapy, respiratory therapy, speech therapy, psychosocial therapy, and dieticians.
Reinforce techniques learned in all of the above therapies. Educate client and family members thoroughly about expected
outcomes and possible problems. Encourage exercise while teaching s/s of exercise overload: feeling
weaker rather than stronger after exercise, excessive muscle soreness, severe muscle cramping, heaviness of extremities, and prolonged shortness of breath.
Ensure braces are a good fit to prevent pressure ulcers and promote stability.
Have equipment (braces, wheelchairs) evaluated by PT, OT to ensure proper fit.
Be sensitive to psychosocial needs and make appropriate referrals. Refer to support groups and clinics.



(*) Gowers' sign






Devices. Rehabilitation
Polypropylene orthosis

Devices. Rehabilitation
Orthopedic shoes

An overhead arm suspension attaches to the back of the wheelchair. The device eliminates gravity and may make it possible for some patients to have functional use of a weak upper extremity.
Devices. Rehabilitation

Death Most common between 15 - 25 years Due to respiratory or cardiac failure Life prolonged by ~ 6 years to 25 years with
respiratory support Life shortened by 2 years with cardiomyopathy
Effects of treatment Walking: Prolonged by 2 to 5 years Strength: Increased Falling: Reduced
While patient still ambulatory ? When started at early age (3 to 5 years) ? May prolong walking long enough to reduce
likelihood of serious scoliosis

Traumatic obstetric brahial plexopathy usually result from traction on the brachial plexus 80 % ( ERB”S – DUCHENE PALSY ( C5 – C6 ) other ( KLUMKE’S PALSY ) C8 – TH 1 or totaly


























Exercise Therapy
Goals = Improve ROM•Especially in direction of convexity•Reduce contractural change of soft tissues on concave side
Done through:•Improve strength, endurance, & postural control of muscles on convex side•Identify & correct vestibular and/or proprioceptive imbalance/deficiency•Improve balance & coordination•Normalize weight bearing in lower extremities & spine

Exercise Therapy
Specific Exercises:•Stretch concave side = balance ball, hanging from bar, leaning against wall•Strengthen convex side = active exercise•Strengthen trunk muscles •Rotary torso exercises to left (right thoracic curve)•Proprioceptive training •Heel lift (up to 5 mm) – goal is to balance weight bearing for CNS re-education, re-evaluate every 6 weeks

Exercise Therapy - continued
•Exercises to restore cervical lordosis•Work with Exercise Ball – proprioceptive control•Sleep posture – lying on side with pillow under ribs•To correct pelvic unleveling (ex. elevated Rt. Ilium)•Strengthen: Lt. QL, Lt. hip adductors, Rt. G Med•Stretch: Rt. QL, Rt. hip adductors, Lt. G Med•Breathing exercises – maximize & normalize chest expansion

Masa depan yang lebih baik