Quick review in hematology for resident
-
Upload
kaipol-takpradit -
Category
Health & Medicine
-
view
136 -
download
3
Transcript of Quick review in hematology for resident

Catch up in hematology
May the force be with you

Topic• Anemia
• Cytopenia
• VTE
• Bleeding disorder
• Hematologic malignancy

Anemia

Anemia by WHO
• Male Hb < 13 g/dL
• Female Hb < 12 g/dL (event in menopause)
• Pregnancy Hb < 11 g/dL

Clinical approach• Acute anemia
• Symptomatic
• Sudden onset
• Usually bleeding or hemolysis
• Precipitate by infection/drugs/trauma

Clinical approach
• Chronic anemia
• Usually asymptomatic/mild symptom (considering very low Hb)
• Usually decrease production (marrow/nutrition)

Iron def• Low MCV High RDW
• Reproductive age female
• Low T sat, Low SI, High TIBC, low ferritin
• Ferrous sulfate 1x3 at maximum (< 200mg/day)
• Further iron supplement 6-9 months

Thalassemia• Genetic disease
• Alpha gene chromosome 16
• Beta gene chromosome 11
• Transfusion dependent vs NTDT
• CBC show low MCV high RDW
• Enlarged spleen

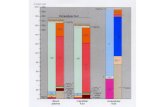
Hb typing• ↓Hct ↓Hb ↓MCV ↑RDW
• A2 > 3.5% Beta trait
• A2 25-35% = E trait
• E > 85% = HomoE (very mild or no anemia)
• H = H disease
• CS 5-6% = Homo CS disease

Hb tying
• A2 10-25% = E trait with alpha-thal or IDA
• E ≅F = E/beta-thal
• A E Bart = AE Bart’s disease (HbH with E trait)
• E F Bart = EF Bart’s disease (HbH with Homo E)

Complication• Hemochromatosis
• NTDT ferritin > 800 ng/mL start chelation
• TD ferritin > 1,000 ng/mL start chelation
• Assessment
• Cardiac and liver MRI T2*
• Liver Bx

Chelation• Deferoxamine SC continuous injection
• Ototoxicity, visual disturb bancla
• Deferasirox Oral Once a day
• Deferiprone Oral 3-4 times a day
• Malaise, N/V, joint pain

Complication
• Extramedullary hematopoiesis
• Ix MRI
• Tx RT, transfusion, hydroxyurea

Complication
• Megaloblastic crisis
• Hemolytic crisis

G-6-PD def.• Male predominant (X-link gene)/Lionization in
female
• WHO type 3 (10-60% with stress induced lysis)
• Precipitated by oxidative stress (sulfa, etc.)
• Normal or mildly increased MCV(∵polychromatia)
• Resolve in 7-10 days

Hereditary Spherocytosis
• AD inherit
• Mild splenomegaly
• May complicated by gall stone
• normal MCV with High MCHC
• Definite treatment is splenectomy

Megaloblastic anemia• Folate or B12 def
• Folate
• Increase homocysteine
• B12
• Increase MMA (methylmalonic acid)
• Increase homocysteine

Megaloblastic anemia• MCV 110-120 High RDW (>130 =auto-agglutination)
• In B12 def
• Hair greying, beefy tongue, impair proprioceptive, dementia
• Mild jaundice, mild fever, mild pancytopenia
• Hypersegmented neutrophil (5-lobe 5%, 6-lobe 1%)

Pernicious anemia
• B12 def from impaired absorption
• Ab to parietal cells or intrinsic factor
• Associated with CA stomach
• Associated with autoimmune including thyroiditis, vitiligo, etc

Pernicious anemia• Treatment
• Cyanocobalamine 100 mcg SC
• OD x 1 wk
• weekly x 1 month
• Then monthly life-long
• Always replace B12 before folate

AIHA• Direct Coomb test positive
• IgG (warm), C3d (cold)
• Gradual onset of anemia and jaundice
• Look for other autoimmune disease, lymphoma
• Tx Prednisone 1 mkd, IVIg, rituximab
• splenectomy is work for warm type

Cytopenia

Thrombocytopenia• Drug induced
• Immune onset 7-10 days (ATB)
• Myelosuppression onset several weeks (rifam, depakene)
• ITP
• TTP/HUS
• DIC

ITP• Plt < 100,000/mcL without cause
• Acute < 3 months
• Persistent 3-12 months
• Chronic > 12 months (Keep Plt > 30,000)
• Look for associated autoimmune
• Treatment Pred 1 mkd, Dexa 40 mgx4days, IVIg, Anti-D, rituximab, splenectomy

TTP/HUS• Pentad (fluctuate neuro, fever, MAHA, low Plt, AKI)
• Rarely bleed
• Low ADAMTS13 (<10%)
• Platelet transfusion is contraindication if no bleed
• Plasma exchange, prednisone, plasma infusion
• Look for HIV, drug (Ticlopidine)

DIC• MAHA + low platelet + coagulopathy + D-dimer > 500
ng/mL
• Acute form severe tissue injury (severe sepsis, large trauma, abruptio placenta, etc.)
• Chronic form (Kassabach-Merit, Trousseau syndrome)
• Treat cause, transfusion only if bleeding
• Heparin in presence of thrombosis

Neutropenia• Febrile neutropenia
• Fever 38.3 or 38 x 1 hr
• Neutropenia ANC < 500 or < 1,000 and decreasing
• If relatively lymphocyte predominate indicate marrow cause
• Drug induced onset several weeks (antipsychotic)

Aplastic anemia• Pancytopenia with hypocellular marrow <25%
• Severe AA: marrow cellularity (2 of 3)
• Reticulocyte count < 60,000
• Platelet < 25,000
• ANC < 500
• Vert severy < 250

Aplastic anemia• Look for drugs, flowcytometry for PNH (CD55,59)
• Severe and very severe
• AlloSCT
• Antithymocyte immunoglobulin + CSA
• Non-severe
• Androgen

VTE

VTE• Provoked VTE
• Hormone, surgery, inflammation, CA, APS
• Non-provoked VTE
• Genetic predisposing -> family Hx
• Protein C,S deficiency, factor V Leiden, protrombin 20210

VTE Treatment• Heparin overlap(5 days at least) with warfarin keep
INR 2-3
• NOAC
• Rivaroxaban
• Apixaban
• LMWH overlap with dabigatran

VTE Treatment• Duration
• Provoked: 3 months
• Unprovoked: 3 months then consider risk of bleeding (~1%/y) vs recurrent (10,20,30,40% at 1,3,5,10 years)
• APS: life long
• Recurrent: life long

Diagnosis of APS

Diagnosis of APS• Objective confirm vascular thrombosis
• Pregnancy-related morbidity
• 3 abort in <10 wk or
• 1 abort after 10 wk or
• Preterm < 34 wk ∵eclampsia/severe preeclampsia of placental insufficiency

Diagnosis of APS• One of these LAB +ve 2 or more at least 12 wk
apart
• Lupus anticoagulant
• Anticardiolipin IgG/IgM* in moderate or high titre
• Anti-β-2GP1 IgG/IgM*
• >40 GPL or MPL or > 99th percentile

Bleeding disorder

Bleeding disorder• Congenital
• Hemophilia A,B
• vWD
• Acquired
• Warfarin overdose
• Acquired hemophilia (autoimmune)

Hemophilia A• X-link recessive
• Factor VIII level
• Mild 6-40%
• Moderate 1-5%
• Severe <1%

Hemophilia A• Treatment
• Give factor VIII/Cryoprecipitate/FFP as soon as trauma
• Dose = Desired level(%) x Wight(kg)
• 1 unit raise FVIII 2%
• Screening for FVIII Ab if frequent treatment

Hemophilia A• Example
• Male 70 kg with knee injury -> Desired level 60%
• Dose = 60% x 70 kg = 4200 ->
• FVIII 2100 units
• Cryoprecipitate 21 units
• FFP 2100 ml

FVIII Ab in hemophilia A• If < 5 Bethesda Unit -> give factor
• If > 5 Bethesda Unit -> give by passing agent
• FEIBA (aPCC)
• Prothrombinase complex concentrate
• rFVII cencentrate

Hemophilia B
• X-link recessive
• Approach similar to hemophilia A
• FIX 1 unit raise FIX 1%
• Cryoprecipitate does not contain FIX

von Willebrand Deficiency
• AD except type3
• Primary hemostatic
• Hemophilia-like in type3
• Late onset -> prolonged menstruation, tooth extraction, etc

vWD• vWF:Ag, vWF:Rco
• Type 1 decrease level
• Type 2 abnormal function
• Type 3 severe deficiency

vWD
• Treatment
• DDAVP for type1 0.3mcg/kg (max 20-24mcg)
• Cryoprecipitate 1 U/10 kg
• FVIII conc. that contain vWF (Rco unit) 40-60 U/kg

Hematologic Malignancy

Hematologic malignancy
• Acute leukemia
• Myeloproliferative neoplasm
• Lymphoproliferative disease
• Plasma cell dyscrasia

AML• Acute -> onset ~1 months
• Pancytopenia -> early disease “aleukemic leukemia
• Blast > 50,000 -> risk of leukostasis
• Monoblast > 30,000 -> of leukostasis
• Extramedullary disease=myeloid sarcoma/chloroma

AML• PBS show myeloblast with Auer’s rod
• Blast > 20% in marrow of peripheral blood
• Extramedullary disease=myeloid sarcoma/chloroma
• Prognosis depend on chromosome
• Good t(8;21), t(16;16)/inv(16)
• Intermediate t(9;11), normal
• Bad -5 -7 +8 complex, t(3;)/inv(3), t(6;9), t(v,11), -5, -7, abnl(17p)

Treatment• Hyperleukocytosis
• Leukapheresis + chemo (Hydrea or Ara-C)
• Induction (7+3) then consolidation of AlloSCT
• Supportive
• leukocyte reduced blood component
• TLS prevention

Tumor lysis syndrome• Hyper K+
• Hyper PO42-
• Hypo Ca2+
• Hyperuricemia
• Renal failure
• Anuria

Tumor lysis syndrome• Hydration
• ± alkalinized urine
• Allopurinol
• Rasburicase
• Dialysis

ALL/lymphoblastic leukemia
• Similar to AML
• Younger age group
• May have lymphadenopathy and hepatosplenomegaly
• Prognosis depend on chromosome, age, T or B cell
• Induction/consolidation/maintenance or AlloSCT

MDS• Anemia or bi- or pancytopenia
• Dysplastic change
• Pseudo Pelger-Huët anomaly
• Megaloblastoid change in marrow
• Prognosis depend on chromosome/blast/cytopenia

MPN• Philadelphia chromosome +ve MPN
• CML
• Philadelphia chromosome -ve MPN
• PV
• ET
• PMF

CML• Philadelphia chromosome -> t(9;22)
• Usually asymptomatic
• High WBC with all stage of myeloid cell
• mild or no anemia and high platelet
• Panmyelosis marrow with dwarf megakaryocyte

CML• Chronic phase
• Treat with TKI (imatinib,nilotinib,dasatinib)
• Accelerated phase
• Blastic phase -> blast > 20% in blood or marrow or cluster of blast in marrow or myeloid sarcoma
• AlloSCT in blastic phase or TKI failure

Polycythemia vera• Hb > 18.5 g/dL in male, 16.5 in female
• Usually have high WBC and Plt
• JAK2V617F mutation in 95% (exon 12 mutation in the rest)
• Rule out secondary cause
• Can progress to myelofibrosis or AML

Polycythemia vera• Tefferi criteria
• Age ≥ 67 (5) 57-66 (2)
• WBC ≥ 15,000 (1)
• Hx of vascular event (1)
• 4:high, 3:int-2, 1-2:int-1, 0:low
• ASA for all, cytoreductive of high risk, phlebolectomy for Hct > 45%

Essential thrombocythemia
• Plt > 450,000 for 6 months
• JAK2V617F in 50% of case
• Increased large hyperlobated bizarre shape megakaryocyte
• Small chance of MF or AML

Essential thrombocythemia• IPSET-thrombosis
• Age ≥ 60 (1)
• Hx of vascular event (2)
• CVD risk (1) (DM, HT, smoking)
• JAK2V617F (2)
• 3:high, 2:int, 1:low
• Low: ± ASA, Int or more: ASA + cytoreductive

Primary myelofibrosis• Pancytopenia with enlarged spleen
• Leukoerythroblastic blood picture
• Progress into AML
• Treatment
• supportive in low risk
• AlloSCT in high risk and fit
• Ruxolitinib can reduce spleen size and improve survival

Lymphoproliferative disease
• Aggressive
• DLBCL, Hodgkin, mantle cell lymphoma, Burkitt lymphoma, TCL
• Indolent lymphoma
• Follicular lymphoma, CLL/SLL, MALT lymphoma

Lymphoproliferative disease• Aggressive
• Progress in several weeks or months
• Need systemic chemotherapy
• Indolent
• Progress over many years
• Local treatment
• In advance stage need treatment only if symptomatic

Hodgkin lymphoma
• Bimodal age distribution (20 and 60 year)
• Alcohol precipitates pain in the node
• Very good prognosis
• In HIV usually occurs in higher CD4 (150-250)

DLBCL• Large cell with CD20+
• IPSS score
• Age > 60
• ECOG > 2
• Stage III-IV
• Extranodal involvement (spleen is nodal)
• Elevated LDH

Plasma cell dyscrasia• MGUS
• M-protein < 3 g, marrow plasma cell < 10%
• Smoldering MM
• M-potein > 3 g, marrow plasma cell > 10%
• MM
• With CRAB

Plasma cell dyscrasia• CRAB
• Calcium > 11 g/dL
• Renal insuff (creatinine > 2 mg/dL)
• Anemia (Hb < 10 g/dL)
• Bone lytic lesion

Plasma cell dyscrasia
• Age ≤ 65 year -> transplant eligible
• Novel agent + chemo + steroid (avoid alkylating angent)
• Age > 65 year -> transplant ineligible
• Melphalan + novel agent + steroid

Amyloidosis
• Amyloid light chain
• Apple green in Congo Red
• Renal involvement cause proteinuria
• Cardiac involvement cause increased Trop-T

Good luck!