OP171
Transcript of OP171

OP169
A retrospecti ve analysis of locally advanc ed tongue cancer trea- ted with surgery at tertiary care centre in India Anuja D. Deshmuk h, Rakesh Katna, Pawan Rane,Devendr a A. Chaukar, Anil K. D’Cruz
Head & Neck Oncology Department, Tata Memorial Centre, Parel,Mumbai, India
Background: Locally advanced oral cancer is mainly treated bymultimoda lity i.e. surgery follow ed by adjuvant therapy. Tongue cancer holds a poor prognosis despite of the advances in various treatment modalities. In the era of organ preservation, surgery for locally advanced tongue cancer is too morbid. Manageme nt ofLocally advanced tongue cancer (LADTCA) surgery revolves around poor prognosis due to early recurre nces and morbid surgery which require extensive reconstruct ion.
Material and methods: Retrospective study of patients with his-tologically proven squamous cell carcinoma of LADTCA whounderwent surgery at our centre during 2008–2011 were ana-lyzed for different histopathological parameters and recurrencepatterns.
Results: We reviewed the charts of 874 patien ts. Wide excision was done in 671 patients and major glossectomy done for 203 patients. Out of these, 57 patients were included in the study after fulfilling the inclusion criteria. All underwent major glossec tomy with neck dissection and reconstructi on. The mean age was 47.5 yrs with majority males. Thirty percent patients were young (<40 yrs). Majority had pedicled flap reconstru ction (74%) and 23%underwent free microvasc ular flaps.
Sixty percent had thickness more than 2 cm.Sixty percent age ofpatients had perineural invasion. Nodal positivity rate was 64% with unilateral nodal positivity in 39% and bilateral positivity in 28%patients. Perinodal extension was seen in 53% of patients. Ninety- four percent had free margins and 6% had involved margins.
Median Disease free survival was 7 month. Sixty-thr ee percent ofpatients had recurrence i.e. local recurrence and/or regional recur- rence in 65% and distant metastasis and/or local disease in 35%patients. Perine ural invasion (p = 0.011), nodal metastasis (p = 0.006), perinodal extension (P = 0.031), bilateral node positivity (p = 0.012) were significantly correlat ed with recurre nce.
Conclusion: Major glossecto my achieves good palliation of symp- toms and offers potential chance of cure in selected cases.
doi:10.1016/j.oraloncolo gy.2013.03.177
OP170
Predictiv e factors of morbidity after salvage surgery in head and neck cancers Rahul Buggaveet i, Shawn T. Joseph, Krishnakum ar Thankappa n,Subrama nia Iyer
Dept. of Head and Neck Surgery, Amrita Institute of Medical sciences,Kochi, India
Purpose: To determ ine predictor s of morbidity after salvage sur- gery of recurre nt head and neck cancer and to evaluate Survival out- comes of salvage surgery.
Materials and methods: Retrospe ctive analysis of 154 pts who underwent salvage surgery after chemo radiation and surgery between August 2004 and May 2011 are included. Patient, tumor and treatment factors, complicatio ns, tube depende nce and recur- rence patterns are analyzed. Wound complicat ions included analysis
of bleeding, local infectio n, pharyngo cutaneou s fistula and oro cuta- neous fistula.Partial and total flap loss, re exploration data recorded .Feeding tube and tracheostomy tube depende nce isanalyzed .
Results: Most of pts in this series has oral cancer (70) and laryn- geal cancer (31). 112 pts received previous RT,47 received CTRT and 38 are treated with surgery alone. 44 pts are treated with sal- vage of both primary and neck, 73 with salvage of primary and 33with salvage of neck alone. Recurren t T stage T4a-47(31%), T3–17(11%). Recurrent N stage N2b 21(14%), N2a 9(6%). Free flap recon- struction is done in 54 (36%) pts.
Wound complications are seen in 28% of pts, flap complications in 12%and tube dependence in 44 %of pts. Mean duration of hospital stay is13 days and ICU is 3.4 days. Previous RT (p = 0.018), previous CT (0.021)and type of salvage surgery (p = 0.002) are significant in univariate analy-sis for wound complications.In multivariate analysis type of salvage sur-gery is significant (p = 0.011, ORR-2.751, CI 1.264 �5.981).Type ofsalvage surgery is significant in univariate analysis for flap complications(p = 0.040) and tube dependence (p = 0.006). 2 year post salvage overallsurvival is 48.7% and 2 year disease free survival is 45%.
Conclusion: Salvage surgery has resulted in good survival out- comes. Previou s RT, previous chemothera py and type of salvage sur- gery are significant predictor s for wound complicat ions. In salvage cases, combining primary surgery with neck surgery will result insignificant increase in morbidity.
doi:10.1016/j.oraloncology.2013.03.178
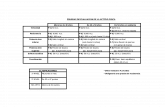
OP171
Salvag e surgery for local recurrence in head and neck squamous cell carcinom a: Oncologic results and predic tive factors for suc- cessful salvage surgery Dong Jin Lee, Kee Hwan Kwon, Eun Jae Chung, Jin Hwan Kim, Il-Seok Park, Young Soo Rho
Departme nt of Otorhino laryngolog y-Head and Neck Surgery, Hallym Univers ity School of Medicine, Seoul, Republic of Korea
Background and objectives: The purpose of this study was to eval- uate the oncolo gic outcome and predictive factors for successfu l sal- vage surgery after local recurrence in head and neck squamous cell carcinoma (HNSCC).
Materials and methods : A retrospec tive study was conduc ted with total 171 patients who developed a recurren ce after primary curative treatmen t for head and neck squamous cell carcinoma and received salvage surgery for their recurre nce. Among them, local recurrence withou t regional or distant metastasis develop ed in 89 (52%)patien ts. Salvage surgery with or without adjouvant therapy was offered to all 89 patients.
Results: The 5-year locoregiona l control rate was 62% and 5-year disease specific surviva l rate was 74%. Univariate analysis showed that previous radiotherap y only as initial treatment (p = 0.013), skin or glottic cancer (p = 0.05), disease free interval more than 6 months (p = 0.01), and initial early T stage (T1 or T2) (p < 0.001) showed favorabl e salvage results. On the other hand, early T stage (T1 orT2) at recur state (p = 0.07), age (p = 0.22), sex (p = 0.76), initial early N stage (N0 or N1) (p = 0.86), and the modality of salvage treatmen t(p = 0.66) were not significant factors regarding successful salvage surgery . In multivaria te analysis, only initial early T stage was inde- penden t predictor of successful salvage for local recurren ce (p = 0.02,Odds ratio 3.398).
Conclusion: In locally recurred HNSCC, skin or glottic cancer had favorabl e salvage result than that of hypopharynx cancer. Disease
S68 Abstracts / Oral Oncology 49 (2013) S4–S79

free interval more than 6 months, and radiotherap y only as an initial therapy had favorable salvage results. Initial early T stage was anindepend ent prognostic factor of salvage treatment in locally recurred group.
doi:10.1016/j.oraloncolo gy.2013.03.179
OP172
The effect of hyperbaric oxygen therapy on treatment of wound complicati ons after oral and (pharyngo) laryngeal salvage surgery Didier Dequant er, Youri Van Hemelri jck, Mohammad Shahla,Pascal Paulus, Christine Aubert, Philippe Lothaire
CHU Vésale, Montigny le Tilleul, Belgium
Purpose : (Chemo) radiotherap y which is often used for cancer inthe head and neck leads to damage of tissue cells and vasculat ure.Surgery in such compromi sed tissues increased complicat ions rate,because wound healing with angiogen esis and fibroplasias, requires normal cell growth conditions. Hyperbaric oxygen therapy raises oxygen levels in hypoxic tissue, stimula tes angiogenes is and fibro-plasia. In this study, we have reviewed the possible clinical value of hyperbari c oxygen therapy for major wounds that show no signs of healing or fistulas after salvage surgery in patients treated with (chemo) radiation of the head and neck regions.
Method s: In this retrospective study, 16 patien ts with soft-tissue wounds without signs of healing after salvage surgery in (chemo)irradiate d head and neck regions were treated with hyperbaric oxy- gen therapy. The patients were treated by HBO, 2.5 bars 90 min daily, usually 20 treatments .
Results : The healing processes seemed to be initiat ed and acceler- ated by HBO. 14 of the 16 the patients healed completel y. There nolife-threat ening complicat ions.
Conclusi on: (Chemo) radioth erapy leads to damage of tissue cells and vasculature. Salvage surgery in such tissues has an increased complicatio ns rate, because wound healing requires angiogen esis and fibroplasias, all of which are jeopardize d. Hyperbaric oxygen therapy raises oxygen levels in hypoxic tissue, stimulate s angiogen -esis and fibroplasias and is an effective and powerful treatment for postoper ative wounds in oral and (pharyngo) laryngeal carcinoma surgery.
doi:10.1016/j.oraloncolo gy.2013.03.180
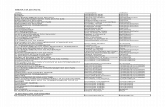
OP173
Predictiv e factors of morbidit y and survival outcomes after sal- vage surgery in head and neck cancers Krishnak umar Thankappa n, Rahul Buggaveeti, Subramania Iyer
Departme nt of Head and Neck Surgery and Oncology , Amrita Institute ofMedical Sciences, Amrita University, Kochi, Kerala, India
Purpose : Treatment of loco-regi onal recurren ces in head and neck is associated with increas ed complicat ions. Purpose of study is toevaluate outcome of salvage surgery and to identify the predictor sof morbidity after such surgery.
Materia ls and method: Retrospe ctive analysis of 150 consecuti vecases of salvage surgery.The study period was between 2004 and 2011.Oper ative and clinical records were analyzed. Morbidit y interms of immediate and long term compli cations such as local
wound complicatio ns, systemi c complicat ions, flap related compli- cations, post operative death, feeding tube and tracheosto my tube depende nce were studied . Oncological outcome in terms of subse- quent recurrence, patterns of recurre nce and survival were analyzed.Univariat e and Multi variate Analysis and Kaplan Meir survival stud- ies were performed.
Results: 70 patients had oral cavity tumors and 37 patients had laryngop haryngeal tumors . 117 patients received previous radio- therapy, 47 receives previous chemoradiot herapy and 38 patien tshad prior surgery alone.44 patients had salvage surgery of the neck and the primary areas, 73 had primary salvage alone and 33 had neck salvage. Recurren ce T stage T4a-47(31%), T3–17(11%). Recur- rence N stage N2b 21(14%), N2a 9(6%). Wound complicatio ns are seen in 28% of pts, flap complicatio ns – 12% of patients. Study has 44% pts with tube depende nce. Free flap reconstru ction is done in54(36%) patients, regional/loc al flap is used in 36(24%) patients.Mean duration of hospital stay is 13 days and ICU stay is 3.4 days.Previou s RT (p = 0.018), previous Chemother apy (0.021) and type of salvage surgery (Combined primary and neck vs either)(p = 0.002) was significant for wound complicatio ns in univariate analysis. On multivariate analysis The type of surgery remained sig- nificant for wound complicatio ns (p = 0.011, Odds Ratio �2.751,95%CI 1.26–5.98). 2 year post salvage overall surviva l is 48.7%. 2 year post salvage disease free survival is 45%. The mean follow up period was 20 months.
Conclusion: Salvage surgery has resulted in Good surviva l out- comes.Pre vious RT, previous chemothera py and type of salvage sur- gery are significant predictor s for wound complicatio ns. In salvage cases, combining primary surgery with neck surgery will result insignificant increase in morbidity.
doi:10.1016/j.oraloncology.20 13.03.181
OP174
The use of oral brush biopsy – Guidelines and practice inGermany Harald Ebhardt a, Luisa Daniel a, Andrea-M aria Schmidt- Westhau sen b
a Center of Oral Pathology, Potsda m, German yb Center of Oral Surgery, Charité-University Medicine, Berlin, Germany
Purpose: The German Society of Dentistry introduc ed guideli nes for diagnostic workup of oral leukoplak ia in 2010. The use of brush biopsy was recommend ed to general dental practitioners to investi- gate homogeneo us leukoplak ia. Patients with inhomoge neous leuko- plakia i.e. suspicious for carcinoma should be referred tomaxillofac ial surgery department s accordin g to this guideli nes.
Material and methods: This study includes 1,449 cytology reports from patients investigat ed by brush biopsy in dental practices inGermany in the years 2009–2012. The indication of brush biopsy of the given lesion was assessed and correlated to the guidelines as well as to the cytopat hological diagnosis.
Results: In the years 2009–2012 out of 1449 patients 699 pre- sented clinically with homogeneo us leukoplak ia, 236 patients with signs of oral lichen planus, 193 patients with candidiasi s, and 352 cases with other lesions (i.e. fibrous polyps, gingivitis, burning mouth disease, and others). In 229 cases no clinical informatio nabout the indication for brush biopsy were given. Cytologicall y,hyperort ho- and parakera tosis was found in 1067 cases, 283 patients had candidias is, and 97 lesions contained atypical/dys plastic kerati- nocytes. The guidelines were followed in 895 out of 1499 cases (59.7%).
Abstracts / Oral Oncology 49 (2013) S4–S79 S69