CMO_11
Transcript of CMO_11
-
8/8/2019 CMO_11
1/7
Clinical Manual of Otolaryngology
CHAPTER 11AIDS/HIV, Hepatitis and Otolaryngology
Otolaryngologists are involved with patients with communicable diseases both in the clinic
and in the operating room. The otolaryngologist is not only involved in diagnosing and
caring for these patients, but is also involved and concerned to reduce the risk of infection
to themselves, their OR assistants and their clinic staff. Two key references are (1)
Exposure to Blood: what health care workers need to know and (2) Guidelines for
prophylaxis of occupational exposure to HIV.
As physicians, we are involved with infectious diseases, many of which are transferable.
The most commonly transmitted diseases are viral respiratory tract and intestinal tract
disease. These are carried by fomites, sputum or other body fluids and these are spread by
direct contact, not by aerosolized spray. The physician has obvious risk, for if they touch a
patient, and then place their hands in their eye or mouth, they may transmit disease.
Frequent hand washing reduces this risk. Keep in mind, however, that patients hands are
also contaminated and they touch virtually everything they come in contact with, from the
front door through the entire clinic visit. Patients may therefore wipe their nose with their
hand or fail to wash after the toilet and contaminate every doorknob in the clinic. Anyone
who touches these doorknobs and then rubs their eye or places their hand in their mouth,
directly or via a snack in the back room, is at risk for infection.
It is alleged that we often contract respiratory tract infections on airplanes. I do not believe
this comes from a poor air system, but rather if the patient in the 1st or 2nd row has a cold
and smears their hands with infected secretion and then decides to travel to the back to
use the rest room, get a magazine or just take a walk, they typically touch each and every
seat as they travel down the aisle. Every body else who travels the aisle, also touches
these seats for balance. Snacks are served, flights are long and people invariably
contaminate themselves by itching their eyes, placing food in their mouth and picking their
teeth. This is all complicated by the stewardesses who serves the food and beverages, and
touching everybody and everything on their serving trip down the aisle.
Most of us recover from a cold without significant sequelae. This is not true for tuberculosis,
HIV illness or hepatitis. Tuberculosis is not covered here, but suffice it to say, it is a major
health risk. Otolaryngologists are involved with patients with TB for they present with cough
-
8/8/2019 CMO_11
2/7
and neck mass.
Hepatitis is the disease which the physician should fear the most. The hepatites are
transmitted differently. Hepatitis A is transmitted through ingestion and Hepatitis B and C
are more commonly transmitted by blood, but with direct contact, other transmission
infection can result. Whether this is through the alimentary track or whether it is through a
small, forgotten cut in the skin, is irrelevant. The bottom line is that these diseases are
readily transmittable, both in the clinic and in the operating room. The risk of transmission
of Hepatitis B and C after needle stick is Hepatitis B 6-30% and Hepatitis C 3.5% (0-7%).
Hepatitis infection requires as few as 100 viral particles, and with salivary and blood
products carrying up to 12 trillion viral particles per cc, very small volumes are required for
successful transmission.
In contrast, HIV illness requires a million viral particles and this commonly requires up to a
cc of blood for successful transmission.
Hepatitis does not particularly have head and neck manifestations and so it is not a disease
that otolaryngologists are called upon to diagnose and treat. However, patients with
hepatitis certainly have other head and neck illnesses and as the otolaryngologist treats
these, are at risk for infection.
HIV illness does have head and neck manifestation and as such, is an important illness.
While the primary care physicians caring for HIV patients are slowly but surely increasing
their abilities to diagnose and treat head and neck illness in the HIV patient, the
otolaryngologist is still called upon to participate in both diagnosis and treatment.
It is difficult to keep track of the magnitude of this illness. The CDC maintains the most
current data. You should refer to the CDC website. Having spent sometime on this website
you will have to browse and determine which sources of information are the most useful.
The numbers which are most impressive to myself are the number of patient currently
infected in the United States, the staggering costs of medical care, the cost of research for
this illness and the magnitude of the illness in 3rd world countries, particularly Africa. In
some countries up to 50% of the sexually active adults are infected with HIV illness.
A summary of current statistics garnered from multiple sources shows that worldwide there
are 36 million people with HIV illness, 35 million adults, 1.5 million children. 70% live in
Africa and 16% live in Asia.
80% of adult HIV infections result from heterosexual relations. 90% of pediatric infections
result from mother to fetus transmission.
In the U.S. the CDC estimates 800,000 to 900,000 people with HIV illness, one third are
http://www.cdc.gov/http://www.cdc.gov/ -
8/8/2019 CMO_11
3/7
unaware of their infection. 40,000 new cases occurred in 1998, 70% men, 30% women,
and 50% were younger than age 25.
60% of males are homosexual, 25% of HIV adults are infected via injection drugs and 15%
are infected via heterosexual sex.
New pediatric HIV infections are decreasing.
As of December 1999, 430,441 deaths from AIDS in the U.S. were reported to the CDC.
This is now the 5th leading cause of adult mortality second only to injuries, cancer, heart
disease and suicide.
Millions of Americans have hepatitis C, most unaware of their infection. 8000 to 10,000
people die annually from hepatitis, primarily B and C.
The HIV retrovirus infects T lymphocytes. These are called CD4 lymphocytes. A normal,
healthy person has approximately 1000 CD4 lymphocytes per cubic milliliter of blood.When the CD4 count drops below about 200 cells/mL, the body's immunity is significantly
compromised, cellular immunity is affected predominately and, hence, organisms such as
protozoans (Pneumocystis), fungi (Candida), and viruses (cytomegalovirus, herpes, and
Epstein-Barr) that are normally cytotoxically killed by CD4 1ymphocytes, can and do
produce disease.
Tumors that are also under the surveillance of the CD4 lymphocytes may begin to appear.
Humoral antibody is also adversely affected, but not to the same degree as the cytotoxic
immune system.
As the immune system is impaired, infections and tumors manifest. The opportunistic
pathogens and the tumors are most notable for two reasons. First, these require cellular
immunity that is now compromised. Second, current medicines against these opportunistic
diseases have not been well developed, because prior to AIDS these were infrequently
troublesome diseases.
The more common bacterial infections are still more frequent. They are of less concern for
two reasons. First, humoral immunologic protection is not as severely affected and, second,current antibiotic availability provides excellent coverage to control and eradicate the
bacterial disease.
Mycobacteria, particularly M. tuberculosis is a relatively common infection. It can present as
a cervical adenopathy that may or may not have a pulmonary component. Extrapulmonary
tuberculosis is particularly increased. The adenopathy is multiple. Normally, it is
successfully eradicated with aggressive medical therapy, but if the nodes are large and
develop necrotic foci, excision of the involved nodes is required. Atypical mycobacterial
-
8/8/2019 CMO_11
4/7
infection, especially M.avium complex, are more common problems than M. tuberculosisin
AIDS.
Fungi present frequently as a pathogen. Candida is the most common and oral candidiasis
is prevalent. Different presentations are seen. The patient will complain of a sensitive,
painful mouth. On examination, the mucosa can be red and sensitive or there may be a
build-up of white exudate. The candida can spread to the pharynx and esophagus and
present as odynophagia. Treatment is topical clotrimazole. A 10-mg troche is prescribed
five times a day, and success is dependent on the patient sucking the troche and keeping
the clotrimazole in contact with the fungi as long as possible. The dissolved clotrimazole is
swallowed, killing the candida in the pharynx and esophagus. Ketoconazole or fluconazole
are alternatives for cases refractory to topical treatment. Histoplasmosis may present with
ulcerative granulomatous lesions in the pharynx. Cases of disseminated histoplasmosis
and coccidiomycosis are increasingly recognized.
Protozoans are uncommon pathogens in healthy humans. Pneumocystis carinii is an
opportunistic protozoan and is common in AIDS. The vast majority of P carinii infections are
pulmonary, but the protozoan has been reported in the external auditory canal, middle ear,
thyroid, and in widely disseminated forms.
Viral infection is also common, and most of the viruses have head and neck manifestations.
The most commonly recognized viruses include cytomegalovirus, Herpes simplex, Herpes
zoster, Epstein-Barr, and human papilloma virus. These can be quite troublesome but are
treated the same as in the general population. Ganciclovir, Foscarnet & Cidofovir are
important new antivirals licensed for treatment of cytomegalovirus infection.
Lymphoproliferative head and neck disorders are also common and can be the initial AIDS
presentation. Patients come to the head and neck surgeon for biopsy with a differential
diagnosis including lymphoma, tuberculosis, and metastatic malignancy. Although a good
history should identify important risk factors, the patient may not always provide the
necessary information. HIV serology should be included in the initial work-up. Operating
room and laboratory personnel must be warned that HIV is a consideration. Even in the HIV
illness patients, different lymphoproliferative disorders are seen. These include reactive
lymph adenopathy, lymphoma, and metastatic malignancy.
Kaposi's sarcoma is also common in HIV illness. Although it normally presents initially with
mucocutaneous lesions, it can manifest in the cervical lymph nodes and it must be
differentiated from epidermoid carcinoma. In a patient with known HIV illness, cervical
lymph node biopsy is frequently requested to differentiate between the myriad of the
aforementioned diseases. Special precautions are necessary for these surgeries and will
be discussed later in this chapter.
-
8/8/2019 CMO_11
5/7
There has been a tendency to subcategorize HIV illness in the head and neck. For the
most part, the diseases such as otitis media, tonsillitis, and sinusitis present the same and
are treated the same as in patients who are immunologically normal. Opportunistic
infections are similar to those seen in other immunocompromised patients. Perhaps these
infections are more difficult to treat and, as with oral candidiasis, may require a longer
medical regimen.
For the most part, the otolaryngologist's primary role is to diagnose. The infections and
tumors are often difficult for the primary care physician to diagnose, and biopsies of
mucosal and lymphoid tissues can be helpful in keeping individual patients well. Because
the otolaryngologist will see HIV illness patients -- some with a known diagnosis, some
without knowledge of the transmission risks is important. Precautions to protect the entire
health team are important.
Since the early 1980s, health care providers have feared (at times irrationally) contracting
AIDS in part because of the social stigma and in part because of the prolonged, miserable
death. As of June 1997, 114 health care workers were considered possible occupational
transmissions. 52 cases are documented; some were by needle stick with contaminated
blood, fewer by spillage of blood into an open wound. Three cases involved spilling
contaminated blood onto mucous membranes.
Current data indicate the risk of contracting AIDS from a percutaneous inoculation of
infected blood to be 0.36%, or a little less than 1 in 300. The risk from mucous membrane
contamination is so low that reliable statistics do not exist. The risk in the dental profession
is estimated at 0.08% (1 in 1300) and occurs from spillage of blood-contaminated saliva
into an open wound. Although other body fluids-tears, saliva, peritoneal fluid, contain HIV,
disease transmission has not been documented. The bottom line is that there may be a
risk, but it is small.
Hepatitis, on the other hand, is highly contagious. The CDC estimates that of 12,000 health
care providers infected annually with hepatitis, 500 to 600 require hospitalization and up to
1200 will become carriers; up to 250 will die annually as a direct result of hepatitis infection.
It therefore behooves all health care providers to take appropriate precautions. The
following are the guidelines recommended by the Operating Room Committee at the VA
San Diego Healthcare System.
Prevention of Transmission of AIDS and Hepatitis for the OR Personnel
The OR Committee recommends that the Medical Center assume an active role in the
prevention of transmission of AIDS and hepatitis for the OR personnel.
1. The OR Committee strongly supports HIV testing for all patients cared for at the
-
8/8/2019 CMO_11
6/7
Medical Center.
2. The OR Committee strongly supports the availability of combination antiretroviral
therapy in the OR suite for immediate administration to consenting OR personnel
accidentally incurring percutaneous or mucous membrane exposure to blood or
body fluids.
3. All OR personnel should be tested and immunized for HBV.
4. The OR Committee strongly supports HIV transmission precautions for all ORpersonnel.
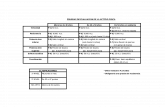
a. The following patient categories are recognized:
High risk = known HIV or HBV positive or at high risk for HIV or HBV
infection;
Low risk = known HIV and HBV negative or at low risk for HIV and HBV
infection.
b. The patient category will be determined by the most senior surgeon in the
OR.
c. The following operational policies are recommended:
AttireHigh-Risked
Patients
Low-Risked
Patients
Eye protection Required Required
Double gloves Required Optional
Impermeable gown Required Optional
Boots Optional Optional
Air filter system Optional Optional
Techniques
Intra-Op self gowning Required Required
Post-Op hand
washingRequired Required
Sharps isolation Required Required
Student/intern
exclusionRequired Required
1.
d. The following clarifications are noteworthy:
i. Eye protection or a face shield is required for the entire operating team
at all times. The only exceptions are individuals performing surgery
through a microscope or endoscope where such gear compromises
visual acuity .Where high-pressure irrigation is used the operating
team will be required to wear full face shields during the irrigation.
ii. Heavy orthopedic gloves may substitute for double gloves. Double
gloves or heavy gloves are recommended for all operating team
-
8/8/2019 CMO_11
7/7
members at all times. Exceptions are those procedures requiring the
delicate touch offered by single gloves.
iii. Impermeable gowns are recommended for all cases where excessive
blood loss, high volume irrigation, or extensive splattering is
anticipated.
iv. Impermeable boots are recommended for cases involving blood or fluid
spillage beyond the operative field.v. Air-filter systems are expensive and should not be used routinely.
However, high risk cases involving extensive splashing, plumes, or
aerosolization make air-filter systems a serious consideration.
vi. Following the initial incision, surgeons scrubbing into a case must
gown and glove themselves if the scrub nurse has contacted tissue,
blood, or body fluids directly or by handling instruments.
vii. All OR personnel are required to wash their hands immediately after
degloving.
viii. Special techniques for passing sharp instruments, pins, and wires willbe required in all high-risk cases.
ix. Inexperienced personnel such as interns and medical students are not
permitted to scrub on high risk cases. Although it is acceptable for
medical students to work with and examine AIDS patients, the
inexperienced should not:
(1) Draw blood on HIV and hepatitis-positive patients.
(2) Assist at surgery on HIV-positive patients.
(3) Perform surgery on HIV and hepatitis-positive patients.
Until venepuncture and surgical skills are developed to a high level of proficiency, the risk is
simply unnecessary .
Every health care provider should be vaccinated against hepatitis infection. Last, should an
inadvertent blood inoculation occur, particularly from a known HIV-infected patient,
everyone should have made the decision to take or not to take combination antiretroviral
therapy (ART) treatment. If one has opted to take ART, it should be readily available and
should be taken within minutes of the inoculation.