Updated EDF guideline on the use of topical steroids in ...€¦ · Women with these dermatoses may...
Transcript of Updated EDF guideline on the use of topical steroids in ...€¦ · Women with these dermatoses may...

Updated evidence-based (S3) European Dermatology Forum guideline on the use of topical corticosteroids in pregnancy
Developed by the Guideline Subcommittee “Topical Corticosteriods” of the
European Dermatology Forum
Subcommittee Members: Prof. Dr. Ching Chi-Chi, Taoyuan (Taiwan) Dr. Gudula Kirtschig, Tübingen (Germany Prof. Dr. Werner Aberer, Graz (Austria) Prof. Dr. Jean-Paul Gabbud, Bern (Switzerland) Prof. Dr. Jasna Lipozenčić, Zagreb (Croatia) Prof. Dr. Sarolta Kápáti, Budapest (Hungary) Prof. Dr. Uwe-Frithjof Haustein, Leipzig (Germany) Prof. Dr. Fenella Wojnarowska, Oxford (United Kingdom) Prof. Dr. Dr. Torsten Zuberbier, Berlin (Germany) Members of EDF Guideline Committee: Prof. Dr. Werner Aberer, Graz (Austria) Prof. Dr. Dieter Metze, Muenster (Germany) Prof. Dr. Martine Bagot, Paris (France) Prof. Dr. Gillian Murphy, Dublin (Ireland) Prof. Dr. Nicole Basset-Seguin, Paris (France) PD Dr. Alexander Nast, Berlin (Germany) Prof. Dr. Ulrike Blume-Peytavi, Berlin (Germany) Prof. Dr. Martino Neumann, Rotterdam (Netherlands) Prof. Dr. Lasse Braathen, Bern (Switzerland) Prof. Dr. Tony Ormerod, Aberdeen (United Kingdom) Prof. Dr. Sergio Chimenti, Rome (Italy) Prof. Dr. Mauro Picardo, Rome (Italy) Prof. Dr. Alexander Enk, Heidelberg (Germany) Prof. Dr. Annamari Ranki, Helsinki (Finland) Prof. Dr. Claudio Feliciani, Rome (Italy) Prof. Dr. Johannes Ring, Munich (Germany) Prof. Dr. Claus Garbe, Tübingen (Germany) Prof. Dr. Berthold Rzany, Berlin (Germany) Prof. Dr. Harald Gollnick, Magdeburg (Germany) Prof. Dr. Rudolf Stadler, Minden (Germany) Prof. Dr. Gerd Gross, Rostock (Germany) Prof. Dr. Sonja Ständer, Münster (Germany) Prof. Dr. Michael Hertl, Marburg (Germany) Prof. Dr. Wolfram Sterry, Berlin (Germany) Prof. Dr. Dimitrios Ioannides, Thessaloniki (Greece) Prof. Dr. Eggert Stockfleth, Bochum (Germany) Prof. Dr. Gregor Jemec, Roskilde (Denmark) Prof. Dr. Alain Taieb, Bordeaux (France) Prof. Dr. Lajos Kemény, Szeged (Hungary) Prof. Dr. George-Sorin Tiplica, Bucharest (Romania) Dr. Gudula Kirtschig, Tübingen (Germany) Prof. Dr. Elke Weisshaar, Heidelberg (Germany) Prof. Dr. Robert Knobler, Vienna (Austria) Prof. Dr. Sean Whittaker, London (United Kingdom) Prof. Dr. Annegret Kuhn, Muenster (Germany) Prof. Dr. Fenella Wojnarowska, Oxford (United Kingdom) Prof. Dr. Marcus Maurer, Berlin (Germany) Prof. Dr. Christos Zouboulis, Dessau (Germany) Prof. Dr. Kai Munte, Rotterdam (Netherlands) Prof. Dr. Dr. Torsten Zuberbier, Berlin (Germany)
Chairman of EDF Guideline Committee: PD Dr. Alexander Nast, Berlin (Germany)
Expiry date: 06/2019
EDF Guidelines Secretariat to PD Dr. Nast: Bettina Schulze, Klinik für Dermatologie, Venerologie und Allergologie, Campus Charité Mitte, Charité – Universitätsmedizin Berlin, Charitéplatz 1, 10117 Berlin, Germany phone: ++49 30 450 518 062, fax: ++49 30 450 518 911, e-mail: [email protected]

1
Croatian Academy of Medical Sciences, Zagreb, Croatia
Updated evidence-based (S3) European Dermatology Forum guideline on
the use of topical corticosteroids in pregnancy
Running head: Updated guideline on topical steroids in pregnancy
C-C. Chi,*† G. Kirtschig,‡ W. Aberer,§ J.-P. Gabbud,¶ J. Lipozenčić, S.**
Kárpáti,†† U-F. Haustein,‡‡ F. Wojnarowska,§§ and T. Zuberbier¶¶
*Department of Dermatology and Centre for Evidence-Based Medicine, Chang Gung
Memorial Hospital, Chiayi, Chiayi, Taiwan
†College of Medicine, Chang Gung University, Taoyuan, Taiwan
‡Department of General Medicine and Interdisciplinary Care, University of Tübingen,
Tübingen, Germany
§Department of Dermatology, University of Graz, Graz, Austria
¶Dermatology and Venereology, Bern, Switzerland
** Croatian Academy of Medical Sciences, Zagreb, Croatia
††Department of Dermatology, Venereology and Dermato-oncology, Semmelweis
University, Budapest, Hungary
‡‡Department of Clinical and Experimental Dermatology, University of Leipzig, Leipzig,
Germany
§§Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK

2
¶¶Allergy-Centre-Charité, Department of Dermatology and Allergy, Charité-
Universitätsmedizin Berlin, Berlin, Germany
Corresponding author
Prof Dr med Dr h c Torsten Zuberbier
Department of Dermatology and Allergy
Charité - Universitätsmedizin Berlin
Charitéplatz 1
D-10117 Berlin
Tel. +49 30 450 518 135
Fax +49 30 450 518 919
E-mail: [email protected]
Funding source: none
Conflict of interest: TZ, institutional funding for research and/or honoria for lectures
and/or consulting from Allergopharma, Ansell, Bayer Schering, DST, Faes Pharma,
Fujisawa, HAL, Henkel, Kryolan, Leti Pharma, Menarini, Merck, MSD, Novartis, Procter
& Gamble, Ranbaxy, Sanofi-Aventis, Schering Plough, Stallergenes, Takeda, and UCB;
the others, none.

3
What’s already known about this topic?
Only limited data on the fetal effects of topical corticosteroids are available.
What does this study add?
Mild/moderate topical corticosteroids are preferred to potent/very potent ones for use
in pregnant women. Use of potent/very potent topical corticosteroids, especially when
the applied amounts are large, is associated with an increased risk of low birth weight.
The current evidence does not support associations of maternal use of topical
corticosteroids with birth defect, preterm birth, and fetal death.
In the choice of the topical corticosteroids, also the risk benefit needs to be assessed
regarding cutaneous side effects for the mother with a higher risk of older topical
corticosteroids in comparison to more modern ones with a better therapeutic index.

4
Summary
Topical corticosteroids may be needed for treating skin conditions in pregnancy.
Nevertheless, only limited data on the fetal effects of topical corticosteroids are available.
A guideline subcommittee of the European Dermatology Forum was organised to update
an evidence-based guideline on the safe use of topical corticosteroids in pregnancy. The
current best evidence is from an updated Cochrane Review which included 14
observational studies with 1,601,515 study subjects and found no significant associations
between maternal use of topical corticosteroids of any potency and some adverse
pregnancy outcomes including mode of delivery, birth defect, preterm delivery, and fetal
death. However, maternal use of potent/very potent topical corticosteroids, especially in
large amounts, is associated with an increased risk of low birth weight. We conclude that
mild/moderate topical corticosteroids should be preferred to potent/very potent ones in
pregnancy and that the well-known topical side effects of corticosteroids on the mother’s
side need to be in the focus of the choice.

5
Introduction
Topical corticosteroids are frequently prescribed for treating various dermatoses
including eczema,1 psoriasis,2 discoid lupus erythematosus,3 and bullous pemphigoid.4
Women with these dermatoses may need topical corticosteroid treatment during
pregnancy. Pregnant women with specific dermatoses of pregnancy, for example atopic
eruption of pregnancy, need topical corticosteroid treatment as well.5 Nevertheless, the
effects of topical corticosteroids on the fetus are largely unclear. Drug references for
example the British National Formulary do not provide explicit instructions on
prescribing topical corticosteroids in pregnancy.6 A typical labelling for use of topical
corticosteroids in pregnancy is: “should be used during pregnancy only if the potential
benefit justifies the potential risk to the fetus.”7
Clinical decisions are usually a trade-off between conceivable benefit and harm.
The lack of knowledge on the safety of topical corticosteroids in pregnancy may result in
physicians’ hesitancy and non- or under-prescribing. Pregnant women’s over-concern of
fetal risk may lead to underuse of topical corticosteroids and decreased therapeutic
effects.8 A previous survey of 250 directors of departments of dermatology across Europe
found 30% were concerned about prescribing topical corticosteroids to pregnancy women
and 91% restrained their prescribing.9
For making an informed clinical decision on the use of topical corticosteroids in
pregnancy, an evidence-based guideline is warranted. We organised a guideline
subcommittee of the European Dermatology Forum and have developed an evidence-
based (S3) guideline on the use of topical corticosteroids in pregnancy in 2011.10 Herein
we present an updated guideline in which we added and appraised new evidence

6
Disclaimer
This guideline was developed by the European Dermatology Forum (available at
http://www.euroderm.org/edf/index.php/edf-guidelines/category/5-guidelines-
miscellaneous). The recommendations reflect the best data available at the time when this
guideline was prepared. Caution should be exercised in interpreting the data; the results
of future studies may require alteration of the conclusions or recommendations in this
report. It may be necessary or even desirable to depart from these recommendations in
special circumstances. Just as adherence to guidelines may not constitute defence against
a claim of negligence, so deviation from them should not be necessarily deemed
negligent.
Levels of evidence and grades of recommendation
Much has been written in recent years on the need for clinical guidelines and the criteria
they should meet for development and application, as well as evidence and
recommendations to be used in their support. We used the levels of evidence defined by
the Oxford Centre for Evidence-Based Medicine (Table 1)11 and the Grading of
Recommendations Assessment, Development and Evaluation (GRADE) Working
Group’s approach to rate the quality of evidence (Table 2).12 The quality of evidence
from randomised trials is initially rated as high and observational studies as low. Further
evaluation may upgrade the quality of evidence for large magnitude effect, dose response,
and confounders likely minimise the effect, and may downgrade due to study limitations,
imprecision, inconsistency of results, indirectness of evidence and publication bias.12

7
Evidence for harm from animal studies
Animal experiments showed corticosteroids have fetotoxic effects and are teratogenic.
Administration of systemic corticosteroids resulted in cleft palate in rabbits, mice, rats,
and hamsters.13-16 The occurrence of genital organ anomalies in mice correlated with the
amounts of corticosteroids applied to the eyes.17 Administration of dexamethasone in
juvenile rhesus monkeys resulted in permanent loss of hippocampal neurons, elevated
plasma cortisol levels at the circadian baseline and post-stress concentrations.18 The birth
weight of fetal lambs reduced after prenatal administration of betamethasone in a dose-
response relationship.19
One animal experiment illustrated that after application on the mothers’ skin,
appreciable levels of betamethasone 17, 21-dipropionate were detected in the fetal blood
of mice and rabbits.20 Animal studies have found topical corticosteroids are also
teratogenic. Diflorasone diacetate cream caused cleft palate after applied to pregnant rats’
skin at a dose of 0.001 mg/kg/day, which was just one-third of the equivalent human
topical dose. The treated rats had a higher rate of fetal death than untreated controls when
the dose was increased to 0.5 mg/kg/day.21 After topical application of diflorasone
diacetate 0.016 mg/kg/day to pregnant rabbits, depressed fetal growth, external anomalies
(31.9%), cleft palate (22.2%), and visceral defects (45.5%) were found.22
To sum up, animal experiments demonstrated that topical application of topical
corticosteroids to pregnant rodents resulted in teratogenic effects, low birth weight, and
increased fetal death, but these experiments cannot be extrapolated to humans as the

8
stratum corneum of the animals is much thinner and the percutaneous absorption is much
higher than in humans.
Pharmacology and pharmacokinetics in the mother
The systemic effects of topical corticosteroids rely on the degree of percutaneous
absorption and the pharmacokinetic pathways for systemically absorbed corticosteroids.
Corticosteroids are bound to plasma proteins, metabolised mainly in the liver, excreted in
the kidney, and cross the placenta in pregnant women.
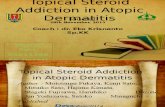
Skin absorption and bioavailability of topical corticosteroids in pregnancy
The systemic effects of topical corticosteroids largely depend on the extent of
percutaneous absorption, which varies from < 0.5 to 7% when applied to intact skin23,24
and also on systemic bioavailability (see Figure 1). The degree of percutaneous
absorption, and hence the potential for systemic exposure, depends upon the following
factors:25
the nature of the corticosteroid chemical compound;
the nature of the vehicle;
the integrity of the skin barrier;
the use of occlusion;
the surface area and regional anatomic variation of the treated skin;
the frequency and duration of application ;
the metabolism of corticosteroids;
inflammation and/or other diseases in the skin;

9
pregnancy (there may be variation in different trimesters).
Hydrocortisone and other corticosteroids have various systemic bioavailability
following topical application due to different lipophilicity, degradability, and other
pharmacokinetic properties. Hydrocortisone, the least potent corticosteroid, is able to
suppress the adrenals following long-term use in children with dermatitis.26 Clobetasol
propionate ointment, the most potent topical corticosteroid, may cause adrenal
insufficiency at a very low dose of 2 g per day for 1 week.23 Adrenal suppression after
application of newer topical lipophilic corticosteroids (i.e. mometasone furoate,
fluticasone propionate, and methylprednisolone aceponate) under extreme conditions
have been documented,27,28 but was not found for mometasone furoate under more
moderate conditions (10 g/day)29 or in psoriatic patients (15 g/day).30
Previous studies found no significant differences in treatment response with once
or twice daily application of very potent corticosteroids. Likewise, there was no
difference or only a slight difference with once or twice daily application of potent or
moderately potent corticosteroids.31
The vehicle may enhance penetration and promote systemic absorption.25 The use
of occlusive dressings, hydration of skin, application over large surface areas, and
prolonged use can enhance systemic absorption.25 Percutaneous penetration is increased
over thin skin including the face, intertriginous areas, and genital area.25
Inflammation and other conditions of the skin may enhance percutaneous
absorption of topical corticosteroids. The percutaneous absorption of 1% hydrocortisone
cream during flares of eczema increased to 11 to 31 times that in remission.32 While only

10
< 0.5% of applied methylprednisolone aceponate was absorbed through intact skin,
removal of the skin barrier by stripping increased the absorption to 15.4 ± 7.7%.24
The change in the hydration and blood flow of the skin in pregnancy may alter the
systemic bioavailability of topical corticosteroids.33 Nevertheless, there have been no
studies on the systemic bioavailability of topical corticosteroids in pregnant women for
ethical concerns.
The data from nasal and inhaled corticosteroids may not be directly applicable to
the skin. The systemic bioavailability of fluticasone propionate and mometasone furoate
through these routes is very low;34-36 however, the data could not be directly extrapolated
to cutaneous application. The newer lipophilic corticosteroids including fluticasone
propionate, mometasone furoate, and methylprednisolone aceponate, should perhaps be
preferred based on fewer local and systemic side effects,37,38 but direct evidence from
pregnant women is lacking. However, these newer corticosteroids do have a better risk-
benefit profile regarding cutaneous side effects (Figure 1)39 and are maybe preferable due
to this benefit. In addition, they have been marketed for over 20 years and used
worldwide in a very high number of patients, giving further indirect evidence for safety
by the lack of reported side effects.
Metabolism of corticosteroids
Over 90% of absorbed corticosteroids in the plasma reversibly combine with two plasma
proteins: corticosteroid-binding globulin (CBG) and albumin. Only unbound
corticosteroids can enter cells to exert actions. Most of circulating corticosteroids are
bound at normal or low plasma levels. At higher plasma levels of corticosteroids, the

11
binding capacity of proteins is overwhelmed, and a greater proportion of the
corticosteroids are in the free form.40 A specific circumstance of physiological
hypercorticism happens in pregnancy. The high circulating oestrogen levels promote the
production of CBG, resulting in elevated total plasma cortisone levels. The physiological
significance of these changes during pregnancy on exogenous corticosteroids is unclear.41
Corticosteroids are metabolised in the liver to water-soluble compounds which are
excreted by the kidneys.40
Placental metabolism
The fetal effects of corticosteroids reply on their extent of transplacental passage (Table
3). The key metabolising enzyme of corticosteroids in the placenta is 11β-hydroxysteroid
dehydrogenase (11βHSD) that transforms biologically active cortisol (hydrocortisone)
into biologically inactive cortisone. Therefore, 11βHSD is the gatekeeper in limiting the
quantities of maternal cortisol that pass through the placenta to enter the fetus and in
protecting the fetus from unwanted harm.42 Hydrocortisone is assumed safe for use in
pregnancy because of the weak potency and high metabolism in the placenta. However,
one study using the fetal-placental unit before abortion found 15% of 3H-cortisol passed
through the placenta without being metabolised43 and another study illustrated a linear
relationship between maternal and fetal serum cortisol levels.44,45 Only 10-12% of
prednisolone passed through the placenta.46 In the meanwhile, dexamethasone,
methylprednisolone, and betamethasone are less metabolised by the placenta, and 67%,
45%, and 30% reached the fetus, respectively.47 Fluticasone propionate and budesonide
are unmetabolised,48 and thus high amounts of them pass through the placenta. To the

12
best of our knowledge, there is a lack of relevant studies on other corticosteroids.
However, the newer corticosteroids like mometasone, which shows a first-pass effect in
the liver, are most unlikely to pass the placenta in significant levels, if - like in other
corticosteroids - a linear relationship between the maternal and the fetal serum may be
assumed. In addition, mometasone is strongly bound to plasma proteins and the free
fraction is approximately 10-20 times lower compared to other corticosteroids49 which
should lead to lower transition into the placenta.
Evidence from human studies
The data available as to possible fetal harm from the use of topical corticosteroids in
pregnancy were limited. The current best evidence is from a recently updated Cochrane
review published in 2015.50 The review authors systematically searched 10 databases
including the Cochrane Skin Group Specialised Register, the Cochrane Pregnancy and
Childbirth Group Specialised Register, the Cochrane Central Register of Controlled
Trials, MEDLINE, EMBASE, LILACS, and five trial registers. They identified 14
relevant studies, including 5 cohort and 9 case-control studies which covered a total of
1,601,515 subjects (Table 4).51-63 A pregnant woman coauthor has been invovled in
preparing this review.
Most of the available data were related to orofacial cleft (level of evidence: 3).
The majority of the included studies found no significant associations between maternal
use of topical corticosteroids and adverse pregnancy outcomes including mode of
delivery, birth defect, preterm delivery, and fetal death, although these studies all had
certain limitations.51-60,62 A significant association between topical corticosteroids and

13
orofacial cleft was found in one small case-control study,61 while none of other included
studies showed a similar effect. Two cohort studies showed a significant association
between maternal use of potent/very potent topical corticosteroids and low birth
weight.59,63 One further study identified an increased risk of low birth weight when the
dispensed amounts of potent/very potent topical corticosteroids were more than 300 g
during pregnancy.60
Conclusions
The available data on the safety of topical corticosteroids in pregnancy suggest a lack of
associations of their use by the mother with birth defect, preterm birth, fetal death, and
mode of delivery. Limited evidence does suggest a significant association of maternal use
of potent/very potent topical corticosteroids, especially in large amounts, with low birth
weight.59,60,63 However, the finding was from only two research groups. Further studies
are warranted for reproducing this finding.
Recommendations
1. Mild/moderate topical corticosteroids should be used in preference to more potent
corticosteroids in pregnancy (low-quality evidence).
2. Potent/very potent topical corticosteroids should be used as second-line therapy for
as short a time as possible. Once daily application of potent/very potent topical
corticosteroids is recommended. Appropriate obstetric care should be provided as
they increase the risk of low birth weight (low-quality evidence).

14
3. The association between maternal exposure to potent/very potent topical
corticosteroids and fetal growth restriction needs to be considered when applying
them during pregnancy. However, systemic corticosteroids have a greater
bioavailability than that of topical corticosteroids, and thus have a greater potential
for fetotoxicity than topical corticosteroids (systemic corticosteroids are associated
with a reduction in fetal birth weight and an increase in preterm delivery64,65), and
should not be used in preference (low-quality evidence).
4. On theoretical grounds the danger of adverse events is increased when areas with
high absorption (e.g. genitals, eyelids, flexures) are treated (very low-quality
evidence).
5. There are no data available to determine if newer lipophilic topical corticosteroids
(mometasone furoate, fluticasone propionate, and methylprednisolone aceponate,)
with a good therapeutic index (Figure 1) are associated with a smaller risk of low
birth weight. On theoretical grounds a favourable side effect profile for the use in
pregnancy is suggested, furthermore they have the practical advantage of once daily
application compared to older preparations (very low-quality evidence).
Advice to women about using topical corticosteroids in pregnancy
1. Women can be reassured that there is no significantly increased risk of birth defect,
preterm delivery, and fetal death while using topical corticosteroids for medical
indications in pregnancy. There is also no increased risk of low birth weight when
using mild/moderate topical corticosteroids in pregnancy.
2. Women should be informed that there is a small risk for low birth weight when

15
using large amounts of potent/very potent topical corticosteroids in pregnancy, but
this risk is less than that of systemic corticosteroids, for an additional risk for
miscarriage and preterm delivery associated with use of systemic corticosteroids.65
3. Depending on the severity of their skin conditions, pregnant women should use
topical corticosteroids of the least potency required and limit the use amounts,
preferably once daily. Pregnant women should be cautious on sites of high
percutaneous absorption for example the skin folds, armpits, and vulva.
References
1 Berth-Jones J. Topical therapy. In: Rook's Textbook of Dermatology (Burns T,
Breathnach SM, Cox N et al., eds), 7th edn. Oxford: Blackwell Publishing. 2004;
75.1-.52.
2 Mason AR, Mason J, Cork M et al. Topical treatments for chronic plaque
psoriasis. Cochrane Database Syst Rev 2013; 3: CD005028.
3 Jessop S, Whitelaw DA, Delamere FM. Drugs for discoid lupus erythematosus.
Cochrane Database Syst Rev 2009: CD002954.
4 Kirtschig G, Middleton P, Bennett C et al. Interventions for bullous pemphigoid.
Cochrane Database Syst Rev 2010: CD002292.
5 Al-Fares SI, Vaughan Jones S, Black MM. The specific dermatoses of pregnancy:
a re-appraisal. Journal of the European Academy of Dermatology and
Venereology : JEADV 2001; 15: 197-206.

16
6 Joint Formulary Committee. British National Formulary (online). In, Vol. 2016.
London: BMJ Group and Pharmaceutical Press. 2016.
7 GlaxoSmithKline. Cutivate cream prescribing information. In. Pittsburgh:
GlaxoSmithKline. 2002.
8 Zuberbier T, Maurer M, Augustin M. Use of topical steroids is largely restricted
by irrational emotional concerns in both patients and physicians. Allergy 2008;
63: 1560-1.
9 Chi CC. Evidence-based assessment of the safety of topical corticosteroids in
pregnancy. In: Nuffield Department of Clinical Medicine, Vol. DPhil thesis.
Oxford: University of Oxford. 2009.
10 Chi CC, Kirtschig G, Aberer W et al. Evidence-based (S3) guideline on topical
corticosteroids in pregnancy. Br J Dermatol 2011; 165: 943-52.
11 OCEBM Levels of Evidence Working Group. The Oxford 2011 Levels of
Evidence. In: Oxford Centre for Evidence-Based Medicine. 2011.
12 Guyatt G, Oxman AD, Akl EA et al. GRADE guidelines: 1. Introduction-GRADE
evidence profiles and summary of findings tables. J Clin Epidemiol 2011; 64:
383-94.
13 Nanda R, van der Linden FP, Jansen HW. Production of cleft palate with
dexamethasone and hypervitaminosis A in rat embryos. Experientia 1970; 26:
1111-2.
14 Nasjleti CE, Avery JK, Spencer HH et al. Tritiated cortisone distribution and
induced cleft palate in mice. Journal of Oral Therapeutics and Pharmacology
1967; 4: 71-82.

17
15 Shah RM, Kilistoff A. Cleft palate induction in hamster fetuses by glucocorticoid
hormones and their synthetic analogues. Journal of Embryology and Experimental
Morphology 1976; 36: 101-8.
16 Walker BE. Induction of cleft palate in rabbits by several glucocorticoids.
Proceedings of the Society for Experimental Biology and Medicine 1967; 125:
1281-4.
17 Ballard PD, Hearney EF, Smith MB. Comparative teratogenicity of selected
glucocorticoids applied ocularly in mice. Teratology 1977; 16: 175-80.
18 Uno H, Eisele S, Sakai A et al. Neurotoxicity of glucocorticoids in the primate
brain. Horm Behav 1994; 28: 336-48.
19 Ikegami M, Jobe AH, Newnham J et al. Repetitive prenatal glucocorticoids
improve lung function and decrease growth in preterm lambs. American Journal
of Respiratory and Critical Care Medicine 1997; 156: 178-84.
20 Yamada H, Nakano M, Ichihashi T et al. Fetal concentration after topical
application of betamethasone 17,21-dipropionate (S-3440) ointment and
teratogenesis in mice and rabbits. [Japanese]. Pharmacometrics 1981; 21: 645-55.
21 Taro. Diflorasone diacetate cream prescribing information. In. Hawthorne: Taro
Pharmaceuticals. 1999.
22 Narama I. Reproduction studies of diflorasone diacetate (DDA). IV.
Teratogenicity study in rabbits by percutaneous administration. [Japanese].
Pharmacometrics 1984; 28: 241-50.
23 Sifton DW, ed. Physicians' Desk Reference, 56th edn. Montvale: Medical
Economics Company. 2002.

18
24 Günther C, Kecskes A, Staks T et al. Percutaneous absorption of
methylprednisolone aceponate following topical application of Advantan lotion
on intact, inflamed and stripped skin of male volunteers. Skin Pharmacol Appl
Skin Physiol 1998; 11: 35-42.
25 Robertson DB, Maibach HI. Topical corticosteroids. Int J Dermatol 1982; 21: 59-
67.
26 Turpeinen M. Adrenocortical response to adrenocorticotropic hormone in relation
to duration of topical therapy and percutaneous absorption of hydrocortisone in
children with dermatitis. Eur J Pediatr 1989; 148: 729-31.
27 Tschen EH, Bucko AD. Assessment of HPA-axis suppression with fluticasone
cream 0.05% in patients with extensive psoriasis or eczema. Clin Drug Investig
1998; 16: 111-6.
28 Kecskes A, Heger-Mahn D, Kuhlmann RK et al. Comparison of the local and
systemic side effects of methylprednisolone aceponate and mometasone furoate
applied as ointments with equal antiinflammatory activity. Journal of the
American Academy of Dermatology 1993; 29: 576-80.
29 Higashi N, Katagiri K. [Percutaneous absorption of 0.1% mometasone furoate
ointment: fate, excretion and adrenocortical suppression]. Skin Research 1990; 32:
395-402.
30 Bressinck R, Williams J, Peets E. Comparison of the effect of mometasone
furoate ointment 0.1%, and hydrocortisone ointment 1%, on adrenocortical
function in psoriasis patients. Today's Ther Trends 1988; 5: 25-34.

19
31 Lagos BR, Maibach HI. Frequency of application of topical corticosteroids: an
overview. Br J Dermatol 1998; 139: 763-6.
32 Turpeinen M, Mashkilleyson N, Bjorksten F et al. Percutaneous absorption of
hydrocortisone during exacerbation and remission of atopic dermatitis in adults.
Acta Derm Venereol 1988; 68: 331-5.
33 Mattison DR. Transdermal drug absorption during pregnancy. Clin Obstet
Gynecol 1990; 33: 718-27.
34 Daley-Yates PT, Kunka RL, Yin Y et al. Bioavailability of fluticasone propionate
and mometasone furoate aqueous nasal sprays. Eur J Clin Pharmacol 2004; 60:
265-8.
35 Allen A, Down G, Newland A et al. Absolute bioavailability of intranasal
fluticasone furoate in healthy subjects. Clin Ther 2007; 29: 1415-20.
36 Corren J. Intranasal corticosteroids for allergic rhinitis: how do different agents
compare? J Allergy Clin Immunol 1999; 104: S144-9.
37 Brazzini B, Pimpinelli N. New and established topical corticosteroids in
dermatology: clinical pharmacology and therapeutic use. Am J Clin Dermatol
2002; 3: 47-58.
38 Mirshahpanah P, Docke WD, Merbold U et al. Superior nuclear receptor
selectivity and therapeutic index of methylprednisolone aceponate versus
mometasone furoate. Experimental dermatology 2007; 16: 753-61.
39 Luger T, Loske KD, Elsner P et al. [Topical skin therapy with glucocorticoids--
therapeutic index]. Journal der Deutschen Dermatologischen Gesellschaft =
Journal of the German Society of Dermatology : JDDG 2004; 2: 629-34.

20
40 Schimmer BP, Parker KL. Adrenocorticotropic hormone; adrenocortical steroids
and their synthetic analogs; inhibitors of the synthesis and actions of
adrenocortical hormones. In: Goodman & Gilman's The Pharmacological Basis of
Therapeutics (Brunton LL, Lazo JS, Parker KL, eds), 11th edn. New York:
McGraw-Hill. 2006; 1587-612.
41 Ho JT, Lewis JG, O'Loughlin P et al. Reduced maternal corticosteroid-binding
globulin and cortisol levels in pre-eclampsia and gamete recipient pregnancies.
Clin Endocrinol (Oxf) 2007; 66: 869-77.
42 Sun K, Yang K, Challis JR. Glucocorticoid actions and metabolism in pregnancy:
implications for placental function and fetal cardiovascular activity. Placenta
1998; 19: 353-60.
43 Murphy BE, Clark SJ, Donald IR et al. Conversion of maternal cortisol to
cortisone during placental transfer to the human fetus. Am J Obstet Gynecol 1974;
118: 538-41.
44 Gitau R, Cameron A, Fisk NM et al. Fetal exposure to maternal cortisol. Lancet
1998; 352: 707-8.
45 Gitau R, Fisk NM, Teixeira JM et al. Fetal hypothalamic-pituitary-adrenal stress
responses to invasive procedures are independent of maternal responses. J Clin
Endocrinol Metab 2001; 86: 104-9.
46 Beitins IZ, Bayard F, Ances IG et al. The transplacental passage of prednisone
and prednisolone in pregnancy near term. The Journal of pediatrics 1972; 81:
936-45.

21
47 Miller NM, Williamson C, Fisk NM et al. Infant cortisol response after prolonged
antenatal prednisolone treatment. BJOG 2004; 111: 1471-4.
48 Murphy VE, Fittock RJ, Zarzycki PK et al. Metabolism of synthetic steroids by
the human placenta. Placenta 2007; 28: 39-46.
49 Hochhaus G. Pharmacokinetic/pharmacodynamic profile of mometasone furoate
nasal spray: potential effects on clinical safety and efficacy. Clin Ther 2008; 30:
1-13.
50 Chi CC, Wang SH, Wojnarowska F et al. Safety of topical corticosteroids in
pregnancy. Cochrane Database Syst Rev 2015; 10: CD007346.
51 Carmichael SL, Ma C, Werler MM et al. Maternal corticosteroid use and
hypospadias. The Journal of pediatrics 2009; 155: 39-44, .e1.
52 Czeizel AE, Rockenbauer M. Population-based case-control study of teratogenic
potential of corticosteroids. Teratology 1997; 56: 335-40.
53 Mygind H, Thulstrup AM, Pedersen L et al. Risk of intrauterine growth
retardation, malformations and other birth outcomes in children after topical use
of corticosteroid in pregnancy. Acta Obstet Gynecol Scand 2002; 81: 234-9.
54 Källén B. Maternal drug use and infant cleft lip/palate with special reference to
corticoids. Cleft Palate Craniofac J 2003; 40: 624-8.
55 Pradat P, Robert-Gnansia E, Di Tanna GL et al. First trimester exposure to
corticosteroids and oral clefts. Birth Defects Research 2003; 67: 968-70.
56 Carmichael SL, Shaw GM, Ma C et al. Maternal corticosteroid use and orofacial
clefts. Am J Obstet Gynecol 2007; 197: 585.e1-.e7.

22
57 Skuladottir H, Wilcox A, McConnaughey R et al. First-trimester nonsystemic
corticosteroid use and the risk of oral clefts in Norway. Ann Epidemiol 2014; 24:
635-40.
58 Skuladottir H, Wilcox AJ, Ma C et al. Corticosteroid use and risk of orofacial
clefts. Birth Defects Res A Clin Mol Teratol 2014; 100: 499-506.
59 Chi CC, Mayon-White RT, Wojnarowska FT. Safety of topical corticosteroids in
pregnancy: a population-based cohort study. J Invest Dermatol 2011; 131: 884-
91.
60 Chi CC, Wang SH, Mayon-White R et al. Pregnancy outcomes after maternal
exposure to topical corticosteroids: a UK population-based cohort study. JAMA
Dermatol 2013; 149: 1274-80.
61 Edwards MJ, Agho K, Attia J et al. Case-control study of cleft lip or palate after
maternal use of topical corticosteroids during pregnancy. Am J Med Genet A
2003; 120: 459-63.
62 Hviid A, Molgaard-Nielsen D. Corticosteroid use during pregnancy and risk of
orofacial clefts. CMAJ 2011; 183: 796-804.
63 Mahé A, Perret JL, Ly F et al. The cosmetic use of skin-lightening products
during pregnancy in Dakar, Senegal: a common and potentially hazardous
practice. Trans R Soc Trop Med Hyg 2007; 101: 183-7.
64 Park-Wyllie L, Mazzotta P, Pastuszak A et al. Birth defects after maternal
exposure to corticosteroids: prospective cohort study and meta-analysis of
epidemiological studies. Teratology 2000; 62: 385-92.

23
65 Gur C, Diav-Citrin O, Shechtman S et al. Pregnancy outcome after first trimester
exposure to corticosteroids: a prospective controlled study. Reprod Toxicol 2004;
18: 93-101.
66 Mehta DK, ed. British National Formulary, 53rd edn. London: BMJ Publishing
Group Ltd and RPS Publishing. 2007.

24
Table 1 Levels of evidence defined by the Oxford Centre for Evidence-Based Medicine
Level 1 Systematic review of randomised trials or n-of-1 trial
Level 2 Randomised trial or (exceptionally) observational study with dramatic effect
Level 3
Non-randomized controlled cohort/follow-up study (post-marketing surveillance)
provided there are sufficient numbers to rule out a common harm. (For long-term
harms the duration of follow-up must be sufficient.)**
Level 4 Case-series, case-control, or historically controlled studies**
Level 5 Mechanism-based reasoning
* Level may be graded down on the basis of study quality, imprecision, indirectness
(study PICO does not match questions PICO), because of inconsistency between studies,
or because the absolute effect size is very small; Level may be graded up if there is a
large or very large effect size.
** As always, a systematic review is generally better than an individual study.

25
Table 2 Grades of recommendation defined by the GRADE Working Group
High We are very confident that the true effect lies close to that of the estimate of
the effect
Moderate
We are moderately confident in the effect estimate: The true effect is likely
to be close to the estimate of the effect, but there is a possibility that it is
substantially different
Low Our confidence in the effect estimate is limited: The true effect may be
substantially different from the estimate of the effect
Very low We have very little confidence in the effect estimate: The true effect is likely
to be substantially different from the estimate of effect
The quality of evidence from randomised trials is initially rated as high and observational
studies as low. Further evaluation may upgrade the quality of evidence for large
magnitude effect, dose response, and confounders likely minimise the effect, and may
downgrade due to study limitations, imprecision, inconsistency of results, indirectness of
evidence and publication bias.

26
Table 3 Placental metabolism and transfer of various corticosteroids
Metabolised by placental 11β-
hydroxysteroid dehydrogenase Placental transfer
Prednisolone 10-12%
Hydrocortisone 85% 15%
Betamethasone 28-33%
Methylprednisolone 44.6%
Dexamethasone 67%
Fluticasone 0%
In summary, it is difficult to predict the effects of topically applied corticosteroid used by
the mother on the unborn child, as there are so many independent factors. Clinical trials
are unethical and therefore have never been conducted.

27
Table 4 Studies on the safety of topical corticosteroids in pregnancy
First author;
publication
year; country;
funding
source
Study design
Setting
Number of participants
Ascertainment of exposure
Outcome measures Results
Czeizel; 1997;
Hungary; not
reported
Case-control
study
Population-
based, using
the dataset
Hungarian
Case-Control
Surveillance of
Congenital
Abnormalities
20,830 cases of congenital
abnormalities, 35,727 controls
Prenatal log book, questionnaire and
interview
Adjusted OR with 95% CI of
maternal ointment
corticosteroid treatment in 14
congenital abnormalities group
An association between cleft lip ± palate and
maternal corticosteroid ointment treatment in the
whole pregnancy [adjusted OR 2.21 (95% CI 1.11-
4.39)] and in the 1st month of gestation [OR 4.19
(95% CI 1.47-11.97)] was revealed. However, the
adjusted OR was not significant in the 2nd and 3rd
months of gestation, which are the critical period
for congenital abnormalities (but the OR statistic
was not reported). Also, no significant association
between maternal corticosteroid ointment use and
other major or mild congenital abnormalities was
found.
Mygind; 2002;
Denmark;
Western Danish
Research Forum
for Health
Sciences, Danish
Medical
Research
Council, and
Foundation of
Hørslev
Retrospective
cohort study
Based on local
population in
North Jutland,
using Danish
Medical Birth
registry
363 primiparous, singleton pregnant
women exposed to topical
corticosteroids within 30 days before
conception and/or during pregnancy,
9263 controls receiving no
prescriptions
Pharmaco-epidemiological prescription
database
Crude and adjusted OR with
95% CI for low birth weight,
malformations, preterm
delivery, and stillbirth
No increased risk of low birth weight,
malformations, preterm delivery and stillbirth
among the exposure group. The adjusted OR (95%
CI) for low birth weight, malformations and
preterm delivery among women receiving
weak/medium strong corticosteroids were 0.7
(0.17–2.85), 0.93 (0.23–3.80) and 1.04 (0.56–
1.92), respectively, and those of strong/very strong
corticosteroids were 1.23 (0.45–3.37), 0.56 (0.14–
2.28) and 0.99 (0.54–1.84), respectively. The
crude OR for stillbirth among women receiving
prescription of topical corticosteroid during
pregnancy was 2.6 (95% CI 0.83-8.05).
Edwards; 2003;
Australia; not
reported
Case-control
study
Single teaching
hospital
48 cases with nonsyndromic cleft lip or
palate, 58 controls
Retrospective interview
OR with 95% CI of topical
corticosteroid use in the first
trimester of pregnancy for
cleft lip or palate, using
univariate and multiple
regression analysis
A significant increase in the prevalence of
maternal first-trimester use of topical
corticosteroid among cases with syndromic cleft
[adjusted OR 18.6 (95% CI 1.29–270), p = 0.032]
Källén; 2003;
Sweden; KA
Wallenberg
Foundation.
Register
analysis
Population-
based, Swedish
Medical Birth
Registry
149,932 women with first-trimester
drug exposure, containing
1094 exposed to topical corticosteroid
Prospective interview at the first
antenatal care visit (usually week 10 to
12)
Expected number of cases
with orofacial cleft, compared
with observed number as risk
ratio (RR; observed/expected)
with 95% CI based on exact
Poisson distribution
No significant association between topical
corticosteroid use in the first trimester of
pregnancy and orofacial clefts [RR 2.01 (95% CI
0.55-5.15)].

28
Pradat; 2003;
multi-national;
not reported
Case-control
study
Multi-centric
database,
Malformation
Drug Exposure
Surveillance
11,150 cases with congenital
malformations, containing 982 cases of
cleft palate or lip
Reported by participating researchers
Mantel-Haenszel OR with
95% CI after stratification by
registry
No correlations of first-trimester exposure to
topical corticosteroids with cleft palate or lip [OR
0.52 (95% CI 0.16-1.64)], cleft palate [OR 0 (95%
CI 0-3.41)], and cleft lip ± palate [OR 0.73 (95%
CI 0.23-2.37)].
Mahé; 2007;
Senegal; not
reported
Cohort study
Single
maternity
hospital
34 of 99 women with exposure to
potent topical corticosteroids (28
clobetasol propionate, 60 g/month).
Compared to non users of very potent
topical corticosteroids
Interviewed at 6-9 months pregnancy,
local area only
Plasma cortisol, Pregnancy
outcome: mode of delivery,
gestational age, birth weight,
placental weight, status of
newborn and mother.
χ2 and Fischer’s two tailed
exact test, Kruskall-Wallis H
test.
Increased frequency of mild vaginal bleeding (p =
0.031), decreased birth weight (P = 0.046),
decreased placental weight (P = 0.043), decreased
placental cortisol (P = 0.07).
Carmichael;
2007; US;
Center for
Disease Control
and Prevention
Case-control
study
Multistate, part
of the National
Birth Defects
Prevention
Study
1110 infants with cleft lip ± cleft palate
and 4079 control infants
Maternal interviews were conducted
with a standardized, computer-based
telephone questionnaire in English or
Spanish, no earlier than 6 weeks and no
later than 24 months after the infant’s
estimated date of delivery
OR with 95% CI of maternal
use of topical corticosteroids
confirmed by clinical
description or surgical or
autopsy report. Each case
received an additional review
by 1 clinical geneticist to
ensure that cases from each
study centre met standard
eligibility criteria.
No significant association between cleft lip ± cleft
palate and maternal use of topical corticosteroids
from 4 weeks before through 12 weeks after
conception [OR 0.9 (95% CI 0.2-4.3)]
Carmichael;
2009; US;
Center for
Disease Control
and Prevention
Case-control
study
Multistate, part
of the National
Birth Defects
Prevention
Study
1165 cases of second- or third-degree
hypospadias and 3000 non-malformed
controls
Maternal interviews were conducted
using a standardized, computer-based
telephone questionnaire in English or
Spanish, no earlier than 6 weeks and no
later than 24 months after the infant’s
estimated date of delivery
OR with 95% CI of maternal
use of topical corticosteroids
confirmed by clinical
description or operative report.
Each case received an
additional review by 1 clinical
geneticist to ensure that cases
from each study centre met
standard eligibility criteria.
No significant association between hypospadias
and maternal use of topical corticosteroids from 4
weeks before through 18 weeks after conception
[OR 0.37 (95% CI 0.12, 1.17)]
Chi; 2011; UK;
British Skin
Foundation and
University of
Oxford
Retrospective
cohort study
Population-
based
35,503 pregnant women prescribed
topical corticosteroids during the period
from 85 days before last menstrual
period to delivery or fetal death and
48,630 unexposed women
Prescription records
Adjusted RR for orofacial cleft
(and its two categories, cleft
lip ± palate and isolated cleft
palate), fetal growth
restriction, preterm delivery,
and fetal death
A significant association of maternal exposure to
potent/very potent topical corticosteroids with
fetal growth restriction [adjusted RR 2.08 (95% CI
1.40-3.10)]. No significant association of topical
corticosteroids of any potency with other
pregnancy outcomes.

29
Hviid; 2011;
Denmark;
Danish Medical
Research
Council and
Lundbeck
Foundation
Retrospective
cohort study
Nationwide
22,480 pregnant women filled
prescriptions for topical corticosteroids
during the first trimester and 810,156
controls receiving no prescriptions for
topical corticosteroids
Danish Prescription Drug Register
Adjusted OR with 95% CI of
cleft lip ± palate and isolated
cleft palate
A significant association of topical corticosteroid
use during first trimester and cleft lip ± palate
[adjusted OR 1.45 (95% CI 1.03-2.05)]. However,
exploratory analyses of the dose-response and
potency-response relations did not support a
causal association. The observed association may
arise from multiple comparisons.
Chi; 2013; UK;
Wellbeing of
Women and
Chang Gung
Memorial
Hospital, Chiayi
Retrospective
cohort study
Population-
based
2658 pregnant women exposed to
topical corticosteroid and 7246
unexposed pregnant women.
Adjusted RR with 95% CI for
orofacial cleft, low birth
weight, preterm delivery, fetal
death, and low Apgar score as
well as mode of delivery
A significantly increased risk of low birth weight
when the dispensed amount of potent or very
potent topical corticosteroids exceeded 300 g
during the entire pregnancy [adjusted RR, 7.74
(95%CI, 1.49-40.11)]. No associations of maternal
topical corticosteroid exposure with orofacial
cleft, preterm delivery, fetal death, low Apgar
score, and mode of delivery.
Skuladottir;
2014; US;
Centers for
Disease Control
and Prevention
Case-control
study
Population-
based
2372 cleft cases (1577 infants with cleft
lip ± palate and 795 infants with cleft
palate alone) and 5922 controls without
major congenital malformations
randomly selected from birth
certificates or birth hospitals
Adjusted OR with 95% CI of
maternal use of topical
corticosteroids during the
periconceptional period
The overall association of corticosteroids and cleft
lip and palate was 1.0 (95% CI, 0.7–1.4).
Skuladottir;
2014; US;
Centers for
Disease Control
and Prevention
Case-control
study
Population-
based
123 cases with cleft lip ± palate and 61
with cleft palate alone identified
through the Medical Birth Registry of
Norway, and 551 control mothers
randomly selected from the Norwegian
Mother and Child Cohort Study
Adjusted OR with 95% CI of
maternal use of topical
corticosteroids during the
periconceptional period
No associations for any cleft type [adjusted OR,
1.0 (95% CI 0.5‒2.2), cleft lip ± palate [adjusted
OR 1.2 (95% CI 0.5‒2.9) nor for cleft palate alone
[adjusted OR 0.6 (95% CI 0.1‒2.6).
Skuladottir;
2014; Norway;
Western
Norwegian
Health
Authorities
Case-control
study
2 specialised
surgical centres
for oral cleft in
Norway
573 cleft cases (377 infants with cleft
lip ± palate and 196 infants with cleft
palate alone) and 763 controls without
major congenital malformations
randomly selected from the Medical
Birth Registry of Norway
Adjusted OR with 95% CI of
maternal first-trimester
exposure to corticosteroids
No significant associations of first-trimester use of
topical corticosteroids with both cleft lip ± palate
(adjusted OR 2.3 ( 95% CI 0.71‒7.7) and cleft
palate alone (adjusted OR, 3.4; CI 0.87‒13)
CI, confidence interval; OR, odds ratio; RR, risk ratio.

30
Table 5 Potency of topical corticosteroids (adapted from the British National Formulary
66 and Chi’s thesis9)
Potency Topical corticosteroids
Mild to moderate Alclometasone dipropionate 0.05%
Betamethasone valerate 0.025%
Clobetasone butyrate 0.05%
Fludroxycortide (flurandrenolone) 0.0125%
Fluocinolone acetonide 0.00625%
Fluocortolone 0.25%
Hydrocortisone 0.1–2.5%
Potent to very potent Betamethasone dipropionate 0.05-0.064%
Betamethasone valerate 0.1-0.12%
Clobetasol propionate 0.05%
Diflucortolone valerate 0.1-0.3%
Fluocinolone acetonide 0.025%
Fluocinonide 0.05%
*Fluticasone propionate 0.005-0.05%
*Hydrocortisone butyrate 0.1%
*Mometasone furoate 0.1%
*Methylprednisolone aceponate 0.1%
Triamcinolone acetonide 0.1%
*The drugs have high potency based on efficacy but fewer adverse effects37,39 (see Figure
1).

31
Figure 1 Therapeutic index of topical corticosteroids (modified from Luger TA et al
200439). BMV, betamethasone valerate; CP, clobetasol propionate; HC, hydrocortisone;
HCB, hydrocortisone butyrate; MF, mometasone furoate; MPA, methylprednisolone
acetate; PC, prednicarbate; TRI, triamcinolone acetonide.

Conflicts of interests The Work Under Consideration for Publication Aberer Chi Gabbud Haustein 1 Grant None None None None 2 Consulting fee or
honorarium None None None None
3 Support for travel to meetings for the study or other purposes
None None None None
4 Fees for participation in review activities, such as data monitoring boards, statistical analysis, end point committees, and the like
None None None None
5 Payment for writing or reviewing the manuscript
None None None None
6 Provision of writing assistance, medicines, equipment, or administrative support
None None None None
7 Other None None None None * This means money that your institution received for your efforts on this study. Relevant financial activities outside the submitted work Aberer Chi Gabbud Haustein 1 Board membership None None None None 2 Consultancy None Received fees
for speaking from Johnson & Johnson Taiwan Ltd, and Pfizer Inc
None None
3 Employment None None Retired from private practice
None
4 Expert testimony None None None None 5 Grants/grants
pending None None None None
6 Payment for lectures including service on speakers bureaus
None Received fees for speaking from Eisai Taiwan Inc, Johnson & Johnson Taiwan Ltd, and Pfizer Taiwan Inc
None None
7 Payment for manuscript preparation
None None None None
8 Patents (planned, pending or issued)
None None None None

9 Royalties None None None None 10 Payment for
development of educational presentations
None None None None
11 Stock/stock options None None None None 12 Travel/accommodati
ons/meeting expenses unrelated to activities listed**
None None None None
13 Other (err on the side of full disclosure)
None None None None
* This means money that your institution received for your efforts. ** For example, if you report a consultancy above there is no need to report travel related to that consultancy on this line. Other relationships Aberer Chi Gabbud Haustein
1 Are there other relationships or activities that readers could perceive to have influenced, or that give the appearance of potentially influencing, what you wrote in the submitted work?
None None None None

Conflicts of interests The Work Under Consideration for Publication Karpati Kirtschig Lipozencic Wojnarowska Zuberbier 1 Grant None None None None None 2 Consulting fee or
honorarium None None None None None
3 Support for travel to meetings for the study or other purposes
None None None None None
4 Fees for participation in review activities, such as data monitoring boards, statistical analysis, end point committees, and the like
None None None None None
5 Payment for writing or reviewing the manuscript
None None None None None
6 Provision of writing assistance, medicines, equipment, or administrative support
None None None None None
7 Other None None None None None * This means money that your institution received for your efforts on this study. Relevant financial activities outside the submitted work Karpati Kirtschig Lipozencic Wojnarowska Zuberbier
1 Board membership None None None None None 2 Consultancy None None None None s. list attached 3 Employment None None None None None 4 Expert testimony None None None None None 5 Grants/grants
pending None None None None s. list attached
6 Payment for lectures including service on speakers bureaus
None None None None s. list attached
7 Payment for manuscript preparation
None None None None None
8 Patents (planned, pending or issued)
None None None None None
9 Royalties None None None None None 10
Payment for development of educational presentations
None None None None None
11
Stock/stock options None None None None None

12
Travel/accommodations/meeting expenses unrelated to activities listed**
None None None None None
13
Other (err on the side of full disclosure)
None None None None None
* This means money that your institution received for your efforts. ** For example, if you report a consultancy above there is no need to report travel related to that consultancy on this line. Other relationships
Karpati Kirtschig Lipozencic Wojnarowska Zuberbier 1 Are there other
relationships or activities that readers could perceive to have influenced, or that give the appearance of potentially influencing, what you wrote in the submitted work?
None None None None None

T:\Dokumente\CoI ‐ Conflict of interests TZ ‐ 2015 2016\CoI ‐ General Disclosure of possible conflict of interest ‐ Torsten Zuberbier ‐ NEU ‐ 180316.docx 25. April 2016
Torsten Zuberbier, MD
Contact details/affiliation:
Department of Dermatology and Allergy
Allergy Centre Charité
Charité ‐Universitätsmedizin Berlin
Charitéplatz 1 / 10117 Berlin, Germany
Phone +4930450518 135/ Fax 49 30 450518919
Email: [email protected]
DISCLOSURE OF POSSIBLE CONFLICT OF INTEREST
Industry consulting, research grants and/or honoraria:
Consulting with the following companies: ALK, Almirall, Abbvie, Astellas, Bayer Health Care, Bencard,
Berlin Chemie, FAES, HAL, Henkel, Kryolan, Leti, Meda, Menarini, Merck, MSD, Novartis,
Pharmasquire, Quintiles, Serono, Stallergenes, Takeda, Teva, UCB
Organizational Affiliations:
Committee member, WHO‐Initiative “Allergic Rhinitis and its Impact on Asthma” (ARIA)
Member of the Board, German Society for Allergy and Clinical Immunology (DGAKI)
Head, European Centre for Allergy Research Foundation (ECARF)
Secretary General , Global Allergy and Asthma European Network (GA²LEN)
Member, Committee on Allergy Diagnosis and Molecular Allergology, World Allergy Organisation (WAO)
Prof. Dr. med. Dr. h. c. Torsten Zuberbier







![[Kuliah 7] Terapi Topical 2015](https://static.fdocument.pub/doc/165x107/55cf8c765503462b138cb174/kuliah-7-terapi-topical-2015.jpg)