Oxidative stress pathways in noncancerous human liver tissue to predict hepatocellular carcinoma...
-
Upload
shinji-tanaka -
Category
Documents
-
view
213 -
download
0
Transcript of Oxidative stress pathways in noncancerous human liver tissue to predict hepatocellular carcinoma...
Oxidative Stress Pathways in Noncancerous HumanLiver Tissue to Predict Hepatocellular CarcinomaRecurrence: A Prospective, Multicenter StudyShinji Tanaka,1* Kaoru Mogushi,2* Mahmut Yasen,2 Daisuke Ban,1 Norio Noguchi,1 Takumi Irie,1
Atsushi Kudo,1 Noriaki Nakamura,1 Hiroshi Tanaka,2 Masakazu Yamamoto,3 Norihiro Kokudo,4
Tadatoshi Takayama,5 Seiji Kawasaki,6 Michiie Sakamoto,7 and Shigeki Arii1
The prediction of cancer recurrence holds the key to improvement of the postoperativeprognosis of patients. In this study, the recurrence of early-stage hepatocellular carcinoma(HCC) after curative hepatectomy was analyzed by the genome-wide gene-expressionprofiling on cancer tissue and the noncancerous liver tissue. Using the training set of 78cases, the cytochrome P450 1A2 (CYP1A2) gene in noncancerous liver tissue was identi-fied as the predictive candidate for postoperative recurrence (hazard ratio [HR], 0.447;95% confidence interval [CI], 0.249-0.808; P 5 0.010). Multivariate analysis revealed thestatistically significant advantage of CYP1A2 down-regulation to predict recurrence (oddsratio, 0.534; 95% CI, 0.276-0.916; P 5 0.036), and the expression of CYP1A2 proteinwas confirmed immunohistochemically. An independently multi-institutional cohort of211 patients, using tissue microarrays, validated that loss of expression of CYP1A2 in non-cancerous liver tissue as the only predictive factor of recurrence after curative hepatectomyfor early-stage HCC (HR, 0.480; 95% CI, 0.256-0.902; P 5 0.038). Gene set-enrichmentanalysis revealed close association of CYP1A2 down-regulation with oxidative stress path-ways in liver tissue (P < 0.001, false discovery rate [FDR] 5 0.042; P 5 0.006, FDR 50.035). Our results indicate these pathways as the molecular targets to prevent recurrence,as well as the potential prediction of the super high-risk population of HCC using livertissue. (HEPATOLOGY 2011;54:1273-1281)
Hepatocellular carcinoma (HCC) is one of themost common malignancies, accounting fornearly 700,000 deaths per year, and the inci-
dence is still increasing worldwide.1 A major obstaclein treatment is the high frequency of tumor recurrencethat is mostly limited to liver tissue, even after curative
resection.2 There have been a number of studies report-ing that advanced tumor factors, including size, num-ber, and vascular invasion of cancer, were significantlyassociated with HCC recurrence.3 Genome-wide gene-expression analysis by DNA microarray offers a system-atic approach to unfold comprehensive information
Abbreviations: AIC, Akaike information criterion; AUC, area under the ROC curve; CI, confidence interval; CNDP1, carnosine dipeptidase 1; CYP1A2,cytochrome P450 1A2; FDR, false discovery rate; GSEA, gene set enrichment analysis; HR, hazard ratio; HCC, hepatocellular carcinoma; NES, normalizedenrichment score; OAT, ornithine aminotransferase; OR, odds ratio; ROC, receiver operating characteristic.From the 1Department of Hepato-Biliary-Pancreatic Surgery, Tokyo Medical and Dental University, Tokyo, Japan; 2Department of Computational Biology, Graduate
School, Tokyo Medical and Dental University, Tokyo, Japan; 3Department of Surgery, Institute of Gastroenterology, Tokyo Women’s Medical University, Tokyo, Japan;4Hepato-Biliary-Pancreatic Surgery Division, Department of Surgery, Graduate School of Medicine, University of Tokyo, Tokyo, Japan; 5Department of DigestiveSurgery, Nihon University School of Medicine, Tokyo, Japan; 6Department of Hepatobiliary-Pancreatic Surgery, Juntendo University School of Medicine, Tokyo, Japan;and 7Department of Pathology, Graduate School of Medicine, Keio University, Tokyo, Japan.Received May 26, 2011; accepted June 24, 2011.This work was supported by a Health and Labour Sciences Research Grant (H20-Kanen-Ippan-001) from the Ministry of Health, Labour and Welfare of Japan
and by Grant-in Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan.*These authors contributed equally to this study.Address reprint requests to: Shigeki Arii, M.D., Ph.D., Department of Hepato-Biliary-Pancreatic Surgery, Tokyo Medical and Dental University, Graduate
School of Medicine, 1-5-45 Yushima, Bunkyo-ku, Tokyo 113-8519, Japan. E-mail: [email protected]; fax: þ81-3-5803-0263.CopyrightVC 2011 by the American Association for the Study of Liver Diseases.View this article online at wileyonlinelibrary.com.DOI 10.1002/hep.24536Potential conflict of interest: Nothing to report.Additional Supporting Information may be found in the online version of this article.
1273
regarding transcription profiles.4 Furthermore, suchstudies should potentially lead to the development of anovel, molecular-targeting therapy of HCC.5 We havepreviously analyzed the genome-wide gene expression ofadvanced HCC with recurrence exceeding Milan crite-ria6 (solitary, �5 cm or up to three nodules �3 cm,without major vascular invasion or distant metastasis)7
and identified novel molecules as therapeutic targets ofHCC.8 Using a prediction system obtained from studiesbased on comprehensive genetic analysis, the selectedgenes may represent different biological characters thatlead to HCC recurrence.On the other hand, there has been little understanding
of the mechanisms of recurrence from the early stage ofHCC.9 It has been reported that gene-expression profil-ing with DNA microarray of noncancerous liver tissuewas closely related to the prognosis in patients withearly-stage HCC.10 Additionally, the translation of suchprofiling data to the bedside requires that gene expressionbe validated as protein expression, and that annotatedclinical samples be available for prospective studies toassess the clinical context and usefulness of putative bio-markers. Tissue microarrays are promising tools of array-based technology in cancer research, and their impor-tance in pathology is increasing because of their role inthe clinical validation of DNA microarrays.11 Tissue-microarray technology allows researchers to examine theexpression and location of protein on hundreds of tissuesamples while preserving morphology. This increasedthroughput accelerates the discovery of important bio-logic markers, compared to traditional marker studies,using whole slide sections and has made this technologyan essential tool in human protein profiling.12
The present study aimed at seeking a biomarkerpredictive for the recurrence after curative resection forearly-stage HCC,3 from both of the cancerous andnoncancerous gene-expression profiles in DNA micro-array data.7 Using a prediction system obtained fromstudies based on training analysis, the biomarker wasindependently validated by the prospective, multicenteranalysis on tissue microarray. Our training and valida-tion studies might indicate this molecule as a novelbiomarker predictive for the postoperative recurrenceof the patients with early-stage HCC. It might also bepotentially useful for the screening of the super high-risk group of HCC using liver tissue.
Patients and Methods
Patients for the Training Set. One hundred eighty-seven patients underwent curative hepatectomy for
HCC from 2004 to 2007 at Tokyo Medical andDental University Hospital (Tokyo, Japan). Amongthem, 98 cases met Milan criteria,6 (Barcelona Clinicliver cancer tumor stage 0-A),3 and written informedconsent from 78 patients, as well as institutionalreview board approval, was obtained. Cancer tissue ofHCC and noncancerous liver tissue adjacent to HCCwere separately divided into two specimens immedi-ately after surgery: one was snap-frozen in liquid nitro-gen and stored at �80�C for microarray analysis, andthe other was fixed in 10% formaldehyde solution andembedded in paraffin for histopathological analysis.Patients were followed up with assays of serum level ofalpha-fetoprotein and protein induced by vitamin Kabsence or antagonists-II every month and with ultra-sonography, computed tomography, and magnetic res-onance imaging every 3 months. Median observationtime was 15.0 months (95% confidence interval [CI],14.0-21.0 months).Gene-Expression Analysis. Total RNA was extracted
from cancer and adjacent noncancerous tissues usingthe RNeasy kit (Qiagen, Hilden, Germany), and integ-rity of obtained RNA was assessed using the Agilent2100 Bioanalyzer (Agilent Technologies, Palo Alto,CA). All samples had an RNA Integrity Numbergreater than 5.0. Contaminant DNA was removed bydigestion with RNase-free DNase (Qiagen). Using 2lg of total RNA, complementary RNA was preparedusing one-cycle target labeling and a control reagentskit (Affymetrix, Santa Clara, CA). Hybridization andsignal detection of HG-U133 Plus 2.0 arrays (Affyme-trix) was performed after the manufacturer’s instruc-tion. A total of 127 microarray datasets were normal-ized using robust multiarray average method under Rstatistical software (version 2.12.0), together with theBioConductor package. Estimated gene-expression lev-els were obtained in log2-transformed values, and 62control probe sets were removed for further analysis.Selection of Predictive Genes for HCC Recurren-
ce. To identify candidate genes for prediction of recur-rence in early-stage HCC, we applied the combinationof criteria for selection of gene probe sets (Fig. 1).First, probe sets corresponding to known genes wereselected based on the NetAffx annotation file, version31 (available at: http://www.affymetrix.com/analysis/index.affx). Then, we selected probe sets marked as‘‘present’’ by Gene Expression Console software version1.1 (version 1.1; Affymetrix) for more than 70% ofpatients. Next, the univariate Cox proportional hazardsregression model was used to estimate the relationshipbetween a gene-expression pattern and tumor recur-rence rate for each probe set. Separate analyses were
1274 TANAKA ET AL. HEPATOLOGY, October 2011
conducted for the cancer tissues, and the adjacent non-cancerous tissues. Probe sets that satisfy P < 0.01 bythe likelihood ratio test and more than 2-fold change inmean expression values between recurrence and nonre-currence groups were selected. Furthermore, probe setsthat satisfied P < 0.01 by the Wilcoxon signed-ranktest and more than 2-fold change between the pairedcancer and adjacent noncancerous tissues were selected.To identify the set of genes that best explain the recur-rence of HCC, a multivariate Cox regression analysiswith a forward variable-selection procedure, based onAkaike information criterion (AIC), was performed as,essentially, described by Lu et al.13 At each step, a vari-able showing the lowest AIC value was added. This pro-cedure was started with a null model (i.e., a model withonly the intercept parameter) and terminated if therewas no improvement in the AIC value.Optimal Predictive Model for HCC Recurrence.
Clinicopathological factors associated with recurrencewere examined by a univariate Cox regression analysis.Factors that satisfied P < 0.05 were subjected to fur-ther analysis. A multivariate Cox regression analysiswith a forward variable-selection procedure was thenperformed in an identical manner to the gene-selectionmethod described above using the candidate factors.To establish the optimal predictive model for HCCrecurrence, expression levels of the candidate genes andclinicopathological factors were combined. Usingselected genes and clinicopathological characteristics bythe procedures described above, a multivariate logisticregression analysis with forward variable-selection pro-
cedure, based on AIC, was performed in a similarmanner to that of Cox regression analysis. Diagnosticperformance was examined by the receiver operatingcharacteristic (ROC) curve and the area under theROC curve (AUC).Immunohistochemical Analysis. Substantial evalua-
tion of the expression of the candidate gene wasassessed by immunohistochemical staining on tissuesections from the patients with HCC meeting Milancriteria. The immunohistochemical studies wereperformed using anti-CYP1A2 antibody (3B8C1:sc-53614; Santa Cruz Biotechnology, Inc., Santa Cruz,CA) at 1:500 dilution with phosphate-buffered salinecontaining 1% bovine serum albumin (Sigma-Aldrich,St. Louis, MO), with reaction in an automated immu-nostainer (Ventana XT System; Ventana MedicalSystems, Inc., Tucson, AZ), using heat-induced epitoperetrieval and a standard diaminobenzidine detectionkit (Ventana). Positivity was defined as more than25% of cells staining with anti-CYP1A2 antibody. Im-munohistochemical staining was estimated under alight microscope by two independent investigators.Validation Study on Tissue Microarrays. To vali-
date the clinical significance of the candidate molecule,it was assessed prospectively using a multicenter cohortfrom 2008 to 2009: Tokyo Medical and DentalUniversity Hospital, The University of Tokyo Hospi-tal, Tokyo Women’s Medical University Hospital,Nihon University Hospital, and Juntendo UniversityHospital. All 211 enrolled patients with early-stageHCC meeting Milan criteria provided written
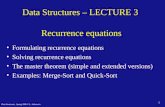
Fig. 1. Flowchart of gene-selec-tion procedures in the training study.
HEPATOLOGY, Vol. 54, No. 4, 2011 TANAKA ET AL. 1275
informed consent, and the relevant institutional reviewboard approved the study. Using the surgically resectedsamples, tissue microarrays were performed with anautomated immunostainer (Ventana XT System). Theimmunohistochemical staining was evaluated under alight microscope by two independent investigators.Gene Set Enrichment Analysis. To investigate bio-
logical backgrounds correlated to a gene-expressionpattern, we used gene set enrichment analysis (GSEA)version 2.0.7 with MSigDB gene sets version 3.0.14
Probe sets marked as present in more than 30% ofpatients were used for this analysis to reduce noise atlow expression levels. Gene set category C5, which isbased on the Gene Ontology database, was used. Genesets satisfying both P < 0.05 and a false discovery rate(FDR) <0.05 were considered as significant.Statistical Analysis. All statistical analyses were per-
formed using R statistical software (version 2.12.0),
including the microarray analysis, as mentioned above.Fisher’s exact test was used for analysis of categoricaldata, and an exact Wilcoxon rank-sum test and anexact Wilcoxon signed-rank test were performed usingthe wilcox_exact function provided by the ‘‘coin’’ pack-age (The Comprehensive R Archive Network), and thesignificance level was set at 0.05.
Results
Candidate Marker Genes for Prediction of HCCRecurrence. Identification of candidate genes for re-currence of HCC was performed using the gene-expression profiles obtained by the DNA microarray(Fig. 1). Of 54,613 probe sets included in the HG-U133 Plus 2.0 array, 41,751 probe sets correspondingto the known human genes were selected. Amongthem, the numbers of probe sets marked as ‘‘present’’
Table 1. Cox Regression Analysis of Recurrence-Free Survivals in 78 Training Cases
Univariate Analysis Variable Selection
Variables HR (95% CI) P Value HR (95% CI) P Value
Molecular factors
IGK (cancer) 0.798 (0.671-0.949) 0.009 — —
FAM134B (cancer) 0.783 (0.655-0.937) 0.006 — —
CYP1A2 (noncancer) 0.662 (0.515-0.850) 0.001 0.662 (0.515-0.850) 0.001
CNDP1 (noncancer) 0.695 (0.554-0.872) 0.002 — —
OAT (noncancer) 0.617 (0.457-0.834) 0.002 — —
Clinicopathological factors
Age 1.033 (0.994-1.074) 0.084
Sex (female versus male) 1.067 (0.535-2.129) 0.853
HBs Ag 0.849 (0.353-2.039) 0.709
HCV Ab 2.095 (1.048-4.188) 0.031 — —
Background liver 0.199
Normal liver 1
Chronic hepatitis 2.842 (0.371-21.753)
Liver cirrhosis 3.971 (0.535-29.475)
ALT 0.998 (0.991-1.004) 0.443
AST 1.007 (0.998-1.016) 0.133
Albumin 0.447 (0.248 -0.808) 0.010 0.447 (0.249-0.808) 0.010
Total bilirubin 1.555 (0.652-3.707) 0.332
Child-Pugh A versus B 2.907 (0.996-8.482) 0.070
AFP (ng/mL) 1.264 (0.915-1.746) 0.171
PIVKA-II (mAU/mL) 0.946 (0.599-1.492) 0.808
Tumor size (cm) 1.058 (0.745-1.501) 0.753
Tumor number (multiple) 1.293 (0.456-3.670) 0.640
Histological differentiation 0.216
Well 1
Moderate 1.553 (0.589-4.099)
Poor 3.497 (0.913-13.394)
Portal vein invasion 1.335 (0.629-2.834) 0.464
Hepatic vein invasion 8.590 (1.074-68.697) 0.118
eg versus ig 0.936 (0.283-3.091) 0.913
fc (�) versus (þ) 1.571 (0.652-3.785) 0.290
fc-inf (�) versus (þ) 1.131 (0.589-2.169) 0.711
sm (�) versus (þ) 0.774 (0.298-2.012) 0.588
Abbreviations: HR, hazard ratio; CI, confidence interval; IGK, immunoglobulin kappa locus; FAM134B, family with sequence similarity 134, member B; CYP1A2, cyto-
chrome P450 1A2; CNDP1, carnosine dipeptidase 1; OAT, ornithine aminotransferase; HBs Ag, hepatitis B surface antigen; HCV Ab, hepatitis C virus antibody; ALT, ala-
nine aminotransferase; AST, aspartate aminotransferase; AFP, alpha-fetoprotein; PIVKA-II, protein induced by vitamin K absence or antagonists-II; sm, surgical margin.
1276 TANAKA ET AL. HEPATOLOGY, October 2011
in >70% of samples derived from cancer tissue andadjacent noncancerous tissue were 17,303 and 16,431,respectively. Using cancer tissue samples, 11 probe setssatisfied the criteria by the Cox likelihood ratio test forrecurrence free (P < 0.01) and more than 2-foldchange between the recurrence and nonrecurrencegroups (Supporting Table 1). Among them, the criteriaby Wilcoxon signed-rank test (P < 0.01) and morethan 2-fold change between the paired cancer andnoncancerous tissues were satisfied by two probe sets:immunoglobulin kappa locus and family withsequence similarity 134, member B (Table 1). Usingnoncancerous tissue samples, five probe sets satisfiedthe criteria by Cox regression analysis and more than2-fold change (Supporting Table 1). Among them,three probe sets, cytochrome P450 1A2 (CYP1A2),carnosine dipeptidase 1 (CNDP1), and ornithine ami-notransferase (OAT), showed significant down-regula-tion in paired cancer tissue. It is of interest that bothcarnosine and ornithine are known as amino acidsclosely related to oxidative stress in the liver.15,16 Themultivariate Cox regression analysis with the forward
variable-selection procedure revealed that a model con-taining only the gene-expression pattern of CYP1A2(HR, 0.447; 95% CI, 0.249-0.808; P ¼ 0.010) wasthe best predictive model for the recurrence of HCC(Table 1).Clinicopathological Factors Associated With HCC
Recurrence. We examined the association betweenclinicopathological factors and recurrence-free survivalsof 78 patients with early-stage HCC meeting theMilan criteria (Table 1; lower). Median recurrence-freesurvival time was 23.7 months. Univariate Cox regres-sion analysis demonstrated that HCV infection(HR, 2.095; 95% CI, 1.048-4.188; P ¼ 0.031) andlow serum albumin level (HR, 0.447; 95% CI, 0.248-0.808; P ¼ 0.010) correlated with the cumulative re-currence-free rate. Other clinicopathological factorswere not statistically significant. We further performedthe forward variable-selection procedure using the twofactors, and the serum albumin level was identified asthe only risk factor for recurrence after curative resec-tion for early-stage HCC (Table 1).Optimal Prediction Model for HCC Recurrence. To
evaluate the best predictive model for patients withHCC meeting the Milan criteria, we considered thecombined model using the serum albumin level andthe gene-expression pattern of CYP1A2 (Table 2). Amultiple logistic regression analysis demonstrated thatCYP1A2 (OR, 0.534; 95% CI, 0.276-0.916; P ¼0.036) was the only factor that contributed to theprediction of the recurrence. Moreover, the variable-selection procedure by logistic regression analysis
Table 2. Multivariate Logistic Regression Analysis ofRecurrence-Free Survivals in 78 Training Cases
Multivariate Analysis Variable Selection
Variables OR (95% CI) P Value OR (95% CI) P Value
CYP1A2 0.534 (0.276-0.916) 0.036 0.493 (0.273-0.787) 0.008
Albumin 0.649 (0.126-3.181) 0.594 — —
Abbreviations: OR, odds ratio; CI, confidence interval; CYP1A2, cytochrome
P450 1A2.
Fig. 2. Training study. (A) Recurrence-free survivals of postoperative patients with early-stage HCC associated with expression of CYP1A2 genein the noncancerous liver tissue. The median expression level for each gene was used as a cut-off value. Red and green lines indicate Kaplan-Meier curves for patients with relative overexpression and underexpression, respectively. The log-rank test was used to assess the statistical dif-ference between the two groups (P ¼ 0.00993). (B) Prediction accuracy of CYP1A2 for HCC recurrence using logistic regression. The AUC was0.747. (C) Immunohistochemical analysis of CYP1A2 in adjacent noncancerous liver tissues from the training study. Upper panel: CYP1A2-highcase; lower panel: CYP1A2-low case (magnification, �200).
HEPATOLOGY, Vol. 54, No. 4, 2011 TANAKA ET AL. 1277
identified that CYP1A2 was the best predictor for therecurrence of HCC meeting the Milan criteria(OR, 0.493; 95% CI, 0.273-0.787; P ¼ 0.008).Cumulative recurrence-free survivals were signifi-
cantly associated with CYP1A2 expression (Fig. 2A).Lower expression of CYP1A2 was statistically relatedto the recurrence of early-stage HCC (P ¼ 0.00993).The predictive accuracy of the CYP1A2 for the HCCrecurrence was assessed by the ROC curve, and theAUC value was 0.747 (Fig. 2B). Protein expression ofCYP1A2 was confirmed by immunohistochemicalstaining on adjacent liver tissues. The CYP1A2 proteinlocalized to the membrane of the endoplasmic reticu-lum of hepatocytes (Fig. 2C).Validation Study on Tissue Microarrays. To exam-
ine the predictive significance of the CYP1A2 expres-sion, we prospectively conducted a multicenter valida-tion study on 211 patients with HCC meeting theMilan criteria. Median observation time was 14.2months (95% CI, 12.9-14.7) in the validation cases.As compared to that in the training cases (15.0months), no significant difference was recognized (P ¼0.108 by the Wilcoxon rank-sum test). Median recur-rence-free survival time was 23.7 and 21.1 months inthe training and validation cases, respectively; indicat-ing no significant difference of recurrence (P ¼ 0.583by log-rank test; Supporting Fig. 1). According to thetissue microarray analysis of noncancerous liver tissuesadjacent to HCC in the validation study (Fig. 3A), 15of 211 patients were identified as CYP1A2 (�), andthe cumulative recurrence-free rates of CYP1A2 (�)patients were significantly lower than CYP1A2 (þ)
patients (Fig. 3B; P ¼ 0.020 by log-rank test). Wealso investigated the association between cumulative re-currence-free rates, clinicopathological factors, and by
Fig. 3. Validation study using a prospective multicenter cohort. (A) Immunohistochemical analysis of CYP1A2 in adjacent noncancerous livertissues using tissue microarray. Left panels: CYP1A2 (þ) cases; right panels, CYP1A2 (�) cases (magnification,, �100). (B) Cumulative recur-rence free rate and protein expression of CYP1A2. Green and red line indicate CYP1A2 (�) and (þ) patients, respectively. Statistically poor prog-nosis was related to loss expression of CYP1A2 (P ¼ 0.020).
Table 3. Cox Regression Analysis of Recurrence-FreeSurvivals in 211 Validation Cases
Variables HR (95% CI) P Value
Molecular factor
CYP1A2 (noncancer) 0.480 (0.256-0.902) 0.038
Clinicopathological factors
Age 1.003 (0.982-1.024) 0.808
Sex (female versus male) 1.100 (0.664-1.823) 0.710
HBs Ag 1.134 (0.684-1.879) 0.630
HCV Ab 1.016 (0.667-1.547) 0.942
Background liver 0.677
Healthy liver 1
Chronic hepatitis 0.734 (0.332-1.623)
Liver cirrhosis 0.844 (0.376-1.895)
Albumin 1.108 (0.742-1.654) 0.615
Total bilirubin 0.760 (0.412-1.404) 0.369
Child-Pugh A versus B 0.271 (0.038-1.947) 0.101
AFP (ng/mL) 1.182 (0.945-1.479) 0.152
PIVKA-II (mAU/mL) 0.917 (0.678-1.240) 0.568
Tumor size (cm) 0.887 (0.728-1.079) 0.223
Tumor number (multiple) 1.616 (0.973-2.683) 0.077
Histological differentiation 0.258
Well 1
Moderately 0.682 (0.418-1.112)
Poorly 0.962 (0.443-2.091)
Portal vein invasion 1.218 (0.719-2.065) 0.473
Hepatic vein invasion 0.450 (0.165-1.227) 0.077
Invasive growth 1.214 (0.661-2.229) 0.542
Capsular formation 1.227 (0.740-2.033) 0.419
Capsular invasion 1.162 (0.751-1.797) 0.497
Surgical margin 1.328 (0.487-3.624) 0.595
Abbreviations: HR, hazard ratio; CI, confidence interval; CYP1A2, cytochrome P450
1A2; HBs Ag, hepatitis B surface antigen; HCV Ab, hepatitis C virus antibody; AFP,
alpha-fetoprotein; PIVKA-II, protein induced by vitamin K absence or antagonists-II.
1278 TANAKA ET AL. HEPATOLOGY, October 2011
univariate Cox regression analysis (Table 3). Interest-ingly, recurrence was not correlated with any clinicopa-thological factors in the validation cohort, but onlywith the loss expression of CYP1A2 protein in non-cancerous tissue (HR, 0.480; 95% CI, 0.256-0.902;P ¼ 0.038). Further logistic regression analysis, usingthe 19 clinicopathological factors and CYP1A2 expres-sion, also revealed that CYP1A2 (�) was the onlysignificant factor by univariate (OR, 0.256; 95% CI,
0.069-0.778; P ¼ 0.024) and multivariate assessments(OR, 0.247; 95% CI, 0.058-0.860; P ¼ 0.038).GSEA Evaluation for CYP1A2 Expression in
HCC. To identify biological pathways related toCYP1A2 expression, GSEA was performed using thegene-expression profiles of the 49 noncancerous tis-sues.14 Because CYP1A2 is one of the most majorenzymes for xenobiotic metabolism in the liver,17 itwas reasonable that most of the gene sets were
Fig. 4. GSEA evaluation of gene-expression profile associated with CYP1A2. (A) PEROXIOME gene set (P < 0.001; FDR ¼ 0.042; NES ¼1.808). (B) OXIDOREDUCTASE_ACTIVITY gene set (P ¼ 0.006; FDR ¼ 0.035; NES ¼ 1.846). Left panels: enrichment plot; right panels: heatmapof genes in the gene sets.
HEPATOLOGY, Vol. 54, No. 4, 2011 TANAKA ET AL. 1279
associated with hepatic metabolism (Supporting Table2). It is noteworthy that gene sets suppressing oxida-tive stress, such as PEROXISOME (P < 0.001; FDR¼ 0.042; normalized enrichment score [NES] ¼1.808) and OXIDOREDUCTASE_ACTIVITY (P ¼0.006; FDR ¼ 0.035; NES ¼ 1.846) demonstratedsignificantly positive correlation with CYP1A2 expres-sion (Fig. 4). Our GSEA evaluation indicated thatCYP1A2 down-regulation may be associated withdegree of oxidative damage in the background liver.
Discussion
In the present study of the prediction of recurrence,we focused on early-stage HCC cases meeting Milancriteria. According to our results, postoperative recur-rence was not associated with any tumor factor thatmight regulate intrahepatic metastasis (Tables 1 and 2).Indeed, recurrence was clinicopathologically associatedwith two host factors, serum albumin levels and HCVinfection in our training cases (Table 1), suggesting thatmulticentric recurrence was dominant for the patientswith chronic liver damages.18 Therefore, the assessmentof noncancerous background tissue should reflect clini-cal outcomes that are not restricted to tumor progres-sion.19,20 Our retrospective study indicated that thenoncancerous gene expression of CYP1A2, CNDP1,and OAT was significantly associated with recurrence(Table 1). The variable-selection procedure revealed thenoncancerous CYP1A2 gene as the best predictivemodel for the recurrence of HCC, but not includingthe cancer-derived genes (Table 1). Further prospective,multicenter study validated that noncancerous CYP1A2expression was identified as a unique biomarker for theprediction of recurrence after the curative resection ofearly-stage HCC (Table 3). Using tissue microarrays,CYP1A2 showed significant negative correlation withthe cumulative recurrence-free rates (Fig. 3).CYP1A2 is a major form of hepatic cytochorme
P450 oxidative system, which is involved in drug me-tabolism and cholesterol synthesis.17 Decreased expres-sion of hepatic CYP1A2 was known to be significantlycorrelated with fibrotic progression of hepatitis Cpatients21 and pathological progress of nonalcoholicfatty liver disease.22 Barker et al. reported previouslythat CYP1A2 was down-regulated dramatically by oxi-dative stress in hepatocytes, indicating CYP1A2 as aspecific surrogate marker of hepatic oxidative damage.23
According to knockout mice analysis by Shertzer et al.,oxidative stress was significantly elevated in the liver mi-crosomes of CYP1A2-knockout mice, compared tothose of wild-type or CYP1A1-knockout mice.24 In this
regard, CYP1A2 may be considered not only a bio-marker of oxidative stress, but also an antioxidantenzyme. The other noncancerous candidates, CNDP1and OAT, might also be associated with oxidative stressby the modulation of amino acids carnosine15 and orni-thine.16 Oxidative stress is known to induce DNA dam-age, and accumulation of such genetic damage caneventually lead to hepatocarcinogenesis.25
To evaluate the biological pathways associated withCYP1A2 expression, we utilized GSEA on the gene-expression profiles of the noncancerous liver tissues.14
GSEA can directly analyze the changes of gene-expres-sion levels as continuous variables.26 According to ourGSEA assessment, the gene sets of peroxisome and oxi-doreductase activity were significantly correlated withCYP1A2 expression levels (Fig. 4). The peroxisome is anorganelle that participates not only in the generation ofreactive oxygen species, but also in cell rescue from thedamaging effects of such oxidative radicals.27 Becausethe loss of hepatic CYP1A2 might be a surrogate bio-marker of oxidative damage related to hepatocarcinogen-esis, the analysis of CYP1A2 might be useful for thepotential screening of the super high-risk population ofHCC by liver biopsy in patients with chronic hepatitis.1
In conclusion, we identified the down-regulation ofCYP1A2 in noncancerous liver tissue as a predictive fac-tor for the recurrence of early-stage HCC. The signifi-cance of noncancerous CYP1A2 was confirmed by a val-idation study using the prospective, multicenter cohort.Close association of CYP1A2 was implicated with theoxidative stress pathways in liver tissue. With respect toantioxidant agents for the prevention of hepatocarcino-genesis,28,29 further investigation is necessary to verifythe roles of CYP1A2-oxidative signaling in early-stageHCC recurrence and, also, in hepatocarcinogenesis.
Acknowledgment: The authors thank Hiromi Ohnariand Ayumi Shioya for clerical and technical assistance.
References1. Bruix J, Sherman M; American Association for the Study of Liver
Diseases. Management of hepatocellular carcinoma: an update. HEPATO-
LOGY 2011;53:1020-1022.2. Arii S, Yamaoka Y, Futagawa S, Inoue K, Kobayashi K, Kojiro M,
et al. Results of surgical and nonsurgical treatment for small-sized hepa-tocellular carcinomas: a retrospective and nationwide survey in Japan.The Liver Cancer Study Group of Japan. HEPATOLOGY 2000;32:1224-1229.
3. Llovet JM. Updated treatment approach to hepatocellular carcinoma. JGastroenterol 2005;40:225-235.
4. Glinsky GV, Berezovska O, Glinskii AB. Microarray analysis identifiesa death-from-cancer signature predicting therapy failure in patientswith multiple types of cancer. J Clin Invest 2005;115:1503-1521.
5. Tanaka S, Arii S. Molecularly targeted therapy for hepatocellular carci-noma. Cancer Sci 2009;100:1-8.
1280 TANAKA ET AL. HEPATOLOGY, October 2011
6. Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F,et al. Liver transplantation for the treatment of small hepatocellular car-cinoma in patients with cirrhosis. N Engl J Med 1996;334:693-699.
7. Tanaka S, Arii S, Yasen M, Mogushi K, Su NT, Zhao C, et al. Aurorakinase B is a predictive factor for the aggressive recurrence of hepatocel-lular carcinoma after curative hepatectomy. Br J Surg 2008;95:611-619.
8. Aihara A, Tanaka S, Yasen M, Matsumura S, Mitsunori Y, Murakata A,et al. The selective Aurora B kinase inhibitor AZD1152 as a noveltreatment for hepatocellular carcinoma. J Hepatol 2010;52:63-71.
9. Tanaka S, Noguchi N, Ochiai T, Kudo A, Nakamura N, Ito K, et al.Outcomes and recurrence of initially resection of hepatocellular carci-noma meeting Milan criteria: rationale for partial hepatectomy as firststrategy. J Am Coll Surg 2007;204:1-6.
10. Hoshida Y, Villanueva A, Kobayashi M, Peix J, Chiang DY, CamargoA, et al. Gene expression in fixed tissues and outcome in hepatocellularcarcinoma. N Engl J Med 2008;359:1995-2004.
11. Kononen J, Bubendorf L, Kallioniemi A, Barlund M, Schraml P,Leighton S, et al. Tissue microarrays for high-throughput molecularprofiling of tumor specimens. Nat Med 1998;4:844-847.
12. Camp RL, Neumeister V, Rimm DL. A decade of tissue microarrays:progress in the discovery and validation of cancer biomarkers. J ClinOncol 2008;26:5630-5637.
13. Lu C, Soria JC, Tang X, Xu XC, Wang L, Mao L, et al. Prognostic fac-tors in resected stage I non-small-cell lung cancer: a multivariate analy-sis of six molecular markers. J Clin Oncol 2004;22:4575-4583.
14. Subramanian A, Tamayo P, Mootha VK, Mukherjee S, Ebert BL, Gil-lette MA, et al. Gene set enrichment analysis: a knowledge-basedapproach for interpreting genome-wide expression profiles. Proc NatlAcad Sci U S A 2005;102:15545-15550.
15. Aydin AF, Kucukgergin C, Ozdemirler-Erata G, Kocak-Toker N, UysalM. The effect of carnosine treatment on prooxidant-antioxidant balancein liver, heart, and brain tissues of male aged rats. Biogerontology2010;11:103-109.
16. Ye SF, Ichimura K, Wakame K, Ohe M. Suppressive effects of activehexose correlated compound on the increased activity of hepatic and re-nal ornithine decarboxylase induced by oxidative stress. Life Sci 2003;74:593-602.
17. Zhou SF, Wang B, Yang LP, Liu JP. Structure, function, regulation, andpolymorphism and the clinical significance of human cytochrome P4501A2. Drug Metab Rev 2010;42:268-354.
18. Okamoto M, Utsunomiya T, Wakiyama S, Hashimoto M, FukuzawaK, Ezaki T, et al. Specific gene-expression profiles of noncancerous liver
tissue predict the risk for multicentric occurrence of hepatocellular car-cinoma in hepatitis C virus-positive patients. Ann Surg Oncol 2006;13:947-954.
19. Finak G, Bertos N, Pepin F, Sadekova S, Souleimanova M, Zhao H,et al. Stromal gene expression predicts clinical outcome in breast can-cer. Nat Med 2008;14:518-527.
20. Villanueva A, Hoshida Y, Battiston C, Tovar V, Sia D, Alsinet C, et al.Combining clinical, pathology, and gene expression data to predict re-currence of hepatocellular carcinoma. Gastroenterology 2011;140:1501-1512.
21. Nakai K, Tanaka H, Hanada K, Ogata H, Suzuki F, Kumada H, et al.Decreased expression of cytochromes P450 1A2, 2E1, and 3A4 anddrug transporters Naþ-taurocholate-cotransporting polypeptide, organiccation transporter 1, and organic anion-transporting peptide-C corre-lates with the progression of liver fibrosis in chronic hepatitis Cpatients. Drug Metab Dispos 2008;36:1786-1793.
22. Fisher CD, Lickteig AJ, Augustine LM, Ranger-Moore J, Jackson JP,Ferguson SS, Cherrington NJ. Hepatic cytochrome P450 enzyme alter-ations in humans with progressive stages of nonalcoholic fatty liver dis-ease. Drug Metab Dispos 2009;37:2087-2094.
23. Barker CW, Fagan JB, Pasco DS. Down-regulation of P4501A1 andP4501A2 mRNA expression in isolated hepatocytes by oxidative stress.J Biol Chem 1994;269:3985-3990.
24. Shertzer HG, Clay CD, Genter MB, Schneider SN, Nebert DW, Dal-ton TP. Cyp1a2 protects against reactive oxygen production in mouseliver microsomes. Free Radic Biol Med 2004;36:605-617.
25. Sakurai T, He G, Matsuzawa A, Yu GY, Maeda S, Hardiman G, KarinM. Hepatocyte necrosis induced by oxidative stress and IL-1 alpharelease mediate carcinogen-induced compensatory proliferation andliver tumorigenesis. Cancer Cell 2008;14:156-165.
26. Mootha VK, Lindgren CM, Eriksson KF, Subramanian A, Sihag S,Lehar J, et al. PGC-1alpha-responsive genes involved in oxidative phos-phorylation are coordinately downregulated in human diabetes. NatGenet 2003;34:267-273.
27. Schrader M, Fahimi HD. Peroxisomes and oxidative stress. BiochimBiophys Acta 2006;1763:1755-1766.
28. Katzenellenbogen M, Mizrahi L, Pappo O, Klopstock N, Olam D, Bar-ash H, et al. Molecular mechanisms of the chemopreventive effect onhepatocellular carcinoma development in Mdr2 knockout mice. MolCancer Ther 2007;6:1283-1291.
29. Shukla Y, Singh R. Resveratrol and cellular mechanisms of cancer pre-vention. Ann N Y Acad Sci 2011;1215:1-8.
HEPATOLOGY, Vol. 54, No. 4, 2011 TANAKA ET AL. 1281