Kos Maghhlski 2012
-
Upload
muhammad-wim-adhitama -
Category
Documents
-
view
221 -
download
0
Transcript of Kos Maghhlski 2012
-
7/25/2019 Kos Maghhlski 2012
1/6
Advances in Medical Sciences Vol. 57(1) 2012 pp 65-70 DOI: 10.2478/v10039-012-0017-7 Medical University of Bialystok, Poland
Inappropriate metformin prescribing in elderlytype 2 diabetes mellitus (T2DM) patients
Department of Internal Disease, Diabetology and Clinical Pharmacology, Medical University of Lodz, Zgierz, Poland
Kosmalski M, Drozdowska A, Sliwinska A, Drzewoski J*
ABSTRACT
Purpose:Metformin is the most commonly prescribed anti-diabetic medication. However, it is often used despite the presence
of contraindications and in unlicensed indications. The main aim of this study was to evaluate the frequency of metformin
use before hospitalization in spite of contraindications in patients with type 2 diabetes mellitus (T2DM) and to evaluate the
prevalence of metformin - associated side effects.
Material/Methods:558 hospitalized patients (mean age = 66.6512.73 years) with poorly controlled T2DM were enrolled.
Detailed medical history including the duration of T2DM, duration of hypoglycemic agents usage prior to hospitalization and
possible metforminassociated side effects was recorded. Patients were subjected to a thorough physical examination and
indispensable biochemical and diagnostic research panel was performed to establish the degree of heart failure, sufficiency of
the respiratory system and kidney function.
Results: 335 out of 558 patients were treated before hospitalization with metformin alone or in combination with other
hypoglycemic agents, mostly sulfonylureas. Contraindications to metformin were found in 275 patients and despite this 120
of them were using this medication in an average dose of 1793.91701.61 mg. However, none of them reported any serious
adverse effects and no significant pH changes were observed. Only three patients reported moderate dyspepsia.
Conclusions:The results of this study indicate a relatively good tolerability of metformin by patients with the traditional
contraindications to this drug. These findings support other authors suggestion that indications and contraindications to
metformin should be re-evaluated.
Key words:diabetes mellitus, metformin, off label use, prescription, side effects
* CORRESPONDING AUTHOR:Department of Internal Disease, Diabetology and Clinical Pharmacology,Medical University of Lodz,Parzeczewska 35,95-100 Zgierz, PolandTel./Fax: +48 42 714 45 51,e-mail: [email protected] (Jozef Drzewoski)
Received 13.12.2011Accepted 07.03.2012Advances in Medical SciencesVol. 57(1) 2012 pp 65-70DOI: 10.2478/v10039-012-0017-7 Medical University of Bialystok, Poland
INTRODUCTION
Metformin is an oral antihyperglycemic agent that has
been used in Europe for over 50 years for type 2 diabetes
(T2DM) treatment. Current American Diabetes Association
and European Association for the Study of Diabetes expert
consensus statement on the approach to the management of
hyperglycemia in individuals with T2DM underlines the role
of using metformin as a safe, effective antihyperglycemic agent
available in inexpensive generic form, together with lifestyle
changes at the time of diagnosis [1]. Therefore, metformin has
become the most frequently prescribed antidiabetic medication
in the world.
When used as labeled, metformin is effective and generally
well - tolerated with the most common adverse effects being
gastrointestinal. However, this old drug is often used off-label
to assist with weight loss, polycystic ovary syndrome, non
alcoholic fatty liver disease, gestational diabetes and HIV
lipodystrophy syndrome. Moreover, the drug is sometimes
prescribed to patients with absolute contraindications, including
kidney, cardiovascular, pulmonary and hepatic disease, and
advanced age. As a result of metformin use in non- approved
indications, the risk of serious side effects, especially life-
threatening lactic acidosis (LA), may substantially increase
[2].
-
7/25/2019 Kos Maghhlski 2012
2/6
Inappropriate metformin prescribing in elderly type 2 diabetes mellitus (T2DM) patients
Given that little information is available on inappropriate
metformin prescribing for elderly T2DM patients in Poland,
we examined the frequency of metformin administration and
occurrence of adverse side effects associated with inappropriate
use of this agent among patients admitted to hospital for poor
metabolic control and coexisting comorbidities.
MATERIAL AND METHODS
The study involved 558 consecutive T2DM patients (mean
age = 66.65 12.73 years) diagnosed and treated by general
practitioners (GPs) or diabetologists, hospitalized in the
Department of Internal Diseases, Diabetology and Clinical
Pharmacology of the Medical University of Lodz from 2009 to
2011 for management of uncontrolled hyperglycemia, diabetes
complications and/or associated comorbidities.
On admission we obtained information concerning current
symptoms, duration of diabetes, history of hyperglycemia
treatment, the dose of metformin taken before hospitalization
and the duration of exposure to this agent, presence or absence
of chronic renal, liver, lungs, and cardiovascular diseases,
and the history of alcohol overuse from the patients using a
combination of patient-self report or family members report,
physical examination, and a review of clinical records.
Congestive heart failure (CHF) was recognized in the
presence of symptoms reported by the patient making it possible
to identify a III or IV class according to the classification of
the New York Heart Association (NYHA). This diagnosis was
verified by additional physical examination and laboratory
or imaging test according to the guidelines proposed by the
European Society of Cardiology (ESC) in 2008.
Chronic renal dysfunction was defined as a GFR 3- fold above normal range and
the presence of common symptoms of liver dysfunction.
Patients were considered to have chronic respiratory failure
if the diagnosis was made before hospitalization and if they
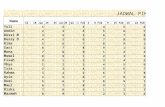
Mean SD
Group A (n= 120) Group B (n= 155)
Age (years) 68.77 11.80 73.00 12.40 P=0.004
Duration of diabetes (years) 7.48 4.82 7.65 6.12 P=0.803
Body mass (kg) 83.12 20.20 77.80 14.55 P=0.012
BMI (kg/m2) 30.48 5.95 29.47 4.87 P=0.123
Waist circumference (cm) 106.27 14.26 103.55 10.92 P=0.074
Hip circumference (cm) 111.40 14.72 108.36 10.71 P=0.049
WHR 0.95 0.07 0.95 0.07 P=1
Systolic blood pressure (mmHg) 139.44 30.56 133.60 24.14 P=0.078
Diastolic blood pressure (mmHg) 78.56 15.01 75.18 11.14 P=0.033
Creatinine (mmol/l) 105.82 59.14 112.98 66.79 P=0.355
Urea (mmol/l) 9.13 5.91 9.98 6.79 P=0.277
GFR (ml/min/1.73m2) 69.09 34.68 67.77 42.49 P=0.782
Fasting glycemia (mmol/l) 9.92 4.04 8.66 4.14 P=0.012
Postprandial glycemia (mmol/l) 12.82 6.79 12.55 6.64 P=0.741
A1C (%) 9.12 2.08 8.56 1.94 P=0.022
Urea acid (umol/l) 365.70 120.73 354.37 121.79 P=0.443
TCH (mmol/l) 4.31 1.25 4.16 1.20 P=0.314
LDL-CH (mmol/l) 2.52 1.15 2.38 1.07 P=0.299
HDL-CH (mmol/l) 1.02 0.43 1.05 0.40 P=0.551
TG (mmol/l) 1.85 1.44 1.74 1.45 P=0.532
Total bilirubine (umol/l) 13.08 8.04 14.43 23.50 P=0.547
ALT (U/l) 44.75 59.54 28.31 28.51 P=0.003
ASP (U/l) 45.46 62.79 32.71 51.02 P=0.067
GGT (U/l) 80.77 116.88 86.97 233.96 P=0.791
Table 1. Characteristics of the patients with contraindications to metformin who were (Group A) and who were not treated with the
drug (Group B).
A1C - glycated hemoglobin , ALT - alanine aminotransferase, ASP - aspartate aminotransferase, BMI - body mass index, GFR - glomerular
filtration rate, GGT - gamma-glutamyl transferase, HDL-CH - HDL cholesterol, LDL-CH - LDL cholesterol, TCH- Total cholesterol,
TG - triglycerides, WHR - waist to hip ratio.
66
-
7/25/2019 Kos Maghhlski 2012
3/6
Kosmalski M et al.
were taking medication for the underlying cause of respiratory
dysfunction.
For each patient, blood pressure and the following
anthropometric indicators were measured: height, body mass,
waist and hip circumference (to calculate BMI and WHR
indexes). Fasting blood sample was taken for the following
analyses: glucose, glycated hemoglobin (A1C), urea,
creatinine, total bilirubin, uric acid, lipid profile and activity of
ALT, ASP and gamma-glutamyl transferase (GGT). Using the
Cocrofta-Gaults formula the glomerular filtration rate (GFR)
was calculated.
The patients with diagnosed contraindications to metformin
were assigned to two groups: patients who were treated with
metformin despite contraindications and patients who were
not treated with metfromin according to the current guideline.
Statistical analysis: Mean and standard deviations
were calculated for normally distributed data. Groups were
compared for significance by One-way ANOVA (Tab. 1).Chi-
square tests (Tab. 2)were used to assess the distributions of
contraindications to metformin. A value of p
-
7/25/2019 Kos Maghhlski 2012
4/6
Inappropriate metformin prescribing in elderly type 2 diabetes mellitus (T2DM) patients
years. Interestingly enough, no cases of LA were noticed and
metformin usage, even in the presence of contraindications,
did not affect the risk of hospitalization or death comparing
with non-users of this drug [3-6]. Although the incidence of LA
in metformin-treated patients is quite rare, this complication
involves very high mortality [7]. Of note, LA occurs also innon-diabetic patients in case of severe infection, cancer, liver
and renal failure, with fatal outcome unless the underlying
condition is corrected. Therefore, pure type B LA (caused by
the accumulation of the drug) in metformin-treated patients,
without coexisting hypoxic factors is diagnosed extremely
rarely [8].
Several studies have shown that plasma metformin levels
were not correlated to blood lactate levels, which raises doubts
whether this drug is a causal factor in LA [7-9]. It should be
stressed that in our study in all patients with contraindications
to metformin no cases of significant pH blood changes were
noted. Similarly to other studies, among contraindications,
we found the prevalence of chronic renal insufficiency and
congestive heart failure, 56 and 46%, respectively.
The incidence of LA in metformin users, reported in
several studies, is equal or even lower in comparison with the
general population of T2DM patients. Of note, in the majority
of LA cases, especially fatal ones, the primary cause of this
life-threatening complication was the presence of underlying
conditions rather than metformin usage per se. Among
coexisting disorders influencing LA development, renal and
congestive heart failure were most often diagnosed [4,10-12].
It is well established that long lasting hyperglycemia in
patients with T2DM connected with accelerated coronary
atherosclerosis is associated with the higher cardiovascularrisk. Metformin, having insulin-sensitizing properties,
has a beneficial effect on cardiovascular risk factors but is
contraindicated in advanced or decompensated heart failure
[13].
Shah et al. [14], observing 401 patients with T2DM and
advanced systolic heart failure using metformin for 14 years
found that the treatment was safe and associated with better
survival. Independently of antihyperglycemic effect, metformin
was proved to improve the function of the myocardium via
activation of a signaling mechanism (AMP-activated protein
kinase), acting at the molecular level. Such a beneficial impact
of metformin may in the future contribute to the usage of thisdrug in the treatment of heart failure, irrespective of coexisting
diabetes.
It is also well known that the positive influence of
metformin on the reduction of total and LDL-cholesterol
as well as triglycerides, body weight and blood pressure in
patients treated with metformin may positively affect cardiac
muscle performance [15]. Additionally, metformin-associated
enhanced fibrinolysis and reduced platelet hyper-aggregation
activity may reduce cardiovascular risk [16].
Lamanna et al. [17] stress that the reduction of
cardiovascular risk in metformin-treated patients with T2DM
seems to be duration-dependent, but according to Khurana
et al. [8] we have no published trails or registry data linking
metformin-associated LA with cardiac catheterization in
patients with T2DM. Even in those with renal impairment,
the data to support a causal relationship with LA is weak.
Moreover, there are doubts whether procedures requiring
iodinated contrast interfere with metformin usage.Metformin is excreted unchanged by the kidneys and renal
function determines the clearance of the drug. The higher risk
of LA in patients with renal impairment taking metformin is
then connected with the accumulation of the drug. According
to insert package information metformin is contraindicated in
patients with creatinine clearance 60ml/min.
Recent investigations aiming to establish pragmatic limits of
renal impairment in patients being considered for treatment
with metformin concluded that an estimated glomerular
filtration rate (GFR) of 30 mL/min should be an absolute
contraindication to the drug. Metformin may be continued
(or initiated) with GFR
-
7/25/2019 Kos Maghhlski 2012
5/6
Kosmalski M et al.
acutely and in those patients in whom oxygenation, tissue
perfusion or liver function are severely compromised [24].
However, in patients with T2DM and stable chronic kidney
disease, clinicians are doing their patients a disservice by
prematurely and unnecessarily withdrawing metformin
treatment. In the latest issue of Diabetologia, Panossian et al.[25], report severe deterioration of glycemic control (an increase
in HbA1c by 3% from baseline within 3-12 months) after
too rash withdrawal of this drug. Metformin was discontinued
because of concern about renal and cardiac function, hepatic
dysfunction or side effects. After careful analysis whether
metformin was truly contraindicated the authors of that report
decided to re-introduce the drug. A significant improvement of
glycemic control and good tolerability after re-introduction of
metformin was observed.
CONCLUSIONS
Althought off-label prescribing is legal and common, it is often
done in the absence of adequate supporting data. In our study
we did not observe any serious adverse effects of metformin
even in patients who had simultaneously as many as several
organ dysfunctions considered as contraindications to this
agent. Therefore, in accordance with others we suggest that
the indications for metformin usage should be reconsidered.
Metformin dosage must be individualized on the basis of
both effectiveness and tolerance, while not exceeding the
maximum recommended daily intake. However, keeping in
mind that unlicensed use of metformin may increase the risk
of serious adverse effects, every patient with T2DM receivingmetformin must have the opportunity to visit his/her medical
doctor frequently and be carefully monitored. Physicians who
prescribe metformin should mandatorily provide appropriate
counseling for patients who receive this drug and be made
aware that they may be liable for deviating from the standard
of care of the patients medical condition.
ACKNOWLEDGEMENTS
This study was supported by grant number 503/0-077-09/503-01
from the Medical University of Lodz, Poland.
REFERENCES
American Diabetes Association. Standards for1.
medical care in diabetes. Diabetes Care. 2011 Jan;34(Suppl.
1):11-61.
Misbin RI. The phantom of lactic acidosis due to2.
metformin in patients with diabetes. Diabetes Care. 2004
Jul;27(1):1791-3.
Calabrese AT, Coley KC, DaPos SV, Swanson D,3.
Rao RH. Evaluation of prescribing practices: risk of lactic
acidosis with metformin therapy. Arch Intern Med.2002 Feb
25;162(4):434-7.
Emslie-Smith AM, Boyle DI, Evans JM, Sullivan F,4.
Morris AD. Contraindications to metformin therapy in patients
with type 2 diabetes a population based study of adherence
to prescribing guidelines. Diabet Med.2001 Jun;18(6):483-8.
Sweileh WM. Contraindications to metformin5.
therapy among patients with type 2 diabetes mellitus. PharmWorld Sci. 2007 Dec;29(6):587-92.
Pongwecharak J, Tengmeesri N, Malanusorn N,6.
Panthong M, Pawangkapin N. Prescribing metformin in type
2 diabetes with a contraindication: prevalence and outcome.
Pharm World Sci. 2009 Aug;31(4):481-6.
Kennedy L, Herman WH. GOAL A1C Study Team.7.
Renal status among patients using metformin in a primary care
setting. Diabetes Care. 2005 Apr;28(4):922-4.
Khurana R, Malik IS. Metformin: safety in cardiac8.
patients. Postgrad Med J. 2010 Jun;86(1016):371-3.
Jones GC, Macklin JP, Alexander WD.9.
Contraindications to the use of metformin. BMJ. 2003
Jan;326(7379):4-5.
Almirall J, Bricull M, Gonzalez-Clemente JM.10.
Metformin-associated lactic acidosis in type 2 diabetes
mellitus: incidence and presentation in common clinical
practice. Nephrol Dial Transplant. 2008 Jul;23(7):2436-8.
Stang M, Wysowski DK, Butler-Jones D. Incidence11.
of lactic acidosis in metformin users. Diabetes Care. 1999
Jun;22(6):925-7.
Cryer DR, Nicholas SP, Henry DH, Mills DJ, Stadel12.
BV. Comparative outcomes study of metformin intervention
versus conventional approach: the COSMIC approach study.
Diabetes Care. 2005 Mar;28(3):539-43
Inzucchi SE. Metformin and heart failure: innocent13.until proven guilty. Diabetes Care. 2005 Oct;28(10):2585-7.
Shah DD, Fonarow GC, Horwich TB. Metformin14.
therapy and outcomes in patients with advanced systolic heart
failure and diabetes. J Card Fail. 2010 Mar;16(3):200-6.
DeFronzo RA, Goodman AM. The Multicenter15.
Metformin Study Group. Efficacy of metformin in patients
with non-insulin-dependent diabetes mellitus. N Engl J
Med.1995 Aug;333(9):541-9.
Nagi DK, Yudkin JS. Effects of metformin on16.
insulin resistance, risk factors for cardiovascular disease, and
plasminogen activator inhibitor in NIDDM subjects. A study
of two ethnic groups. Diabetes Care 1993 Apr;16(4):621-9.Lamanna C, Monami M, Marchionni N, Mannucci17.
E. Effect of metformin on cardiovascular events and mortality:
a meta-analysis of randomized clinical trials. Diabetes Obes
Metab. 2011 Mar;13(3):221-8.
Lipska KJ, Bailey CJ, Inzucchi SE. Use of metformin18.
in the setting of mild-to-moderate renal insufficiency. Diabetes
Care. 2011 Jun;34(6):1431-7.
Kazory A, Walsh K, Harman E, Talor Z. Is metformin19.
safe in patients with mild renal insufficiency? Diabetes Care.
2007 Feb;30(2):444.
National Kidney Foundation. K/DOQI clinical20.
practice guidelines for chronic kidney disease: evaluation,
69
-
7/25/2019 Kos Maghhlski 2012
6/6
Inappropriate metformin prescribing in elderly type 2 diabetes mellitus (T2DM) patients
classification, and stratification. Am J Kidney Dis. 2002
Feb;39(2 Suppl 1):S1-266.
Gregorio F, Manfrini S, Testa I, Filipponi P.21.
Metformin treatment in elderly type II diabetic patients. Arch
Gerontol Geriatr. 1996;22(Suppl.1):261-70.
McCormack J, Johns K, Tildesley H. Metformins22.contraindications should be contraindicated. CMAJ. 2005
Aug;173(5):502-4.
Holstein A, Stumvoll M. Contraindications can23.
damage your health-is metformin a case in point? Diabetologia.
2005 Dec;48(12):2454-9.
Nye HJ , Herrington WG: Metformin: The safest24.
hypoglycaemic agent in chronic kidney disease?. Nephron
Clin Pract 2011;118(4):c3803.
Panossian Z, Drury PL, Cundy T. Reversible25.
severe deterioration of glycaemic control after withdrawal of
metformin treatment. Diabetologia 2012 Jan;55(1):267-9.
70