Blood Conservation in Cardiopulmonary Bypass 서울대학교병원 김경환.
-
Upload
elwin-gregory -
Category
Documents
-
view
223 -
download
0
Transcript of Blood Conservation in Cardiopulmonary Bypass 서울대학교병원 김경환.

Blood Conservation inCardiopulmonary Bypass
서울대학교병원
김경환

Introduction
• A minority of patients in cardiac surgery (15~20%) consume more than 80% of the blood products.
• Blood must be viewed as a scarce source that carries risks and benefits.
• Careful review of available published evidence can provide guidelines.
As CABG became accepted surgical intervention, there was concern that the nation’s entire blood supply might be consumed by cardiac surgery alone.– Tector et al. Reduction of blood usage in open heart surgery. Chest 197
6;4:283-287.

ACC/AHA guideline

Risks of blood transfusion
• Infection– HIV, HBV, HCV, bacterial infection
• Immunologic reactions– Febrile nonhemolytic transfusion reaction (1%)– Anaphylactic transfusion reaction (1/20000~50000)– ABO mismatch– Hemolysis (1/60000)– Death (1/600000)– Transfusion-related acute lung injury (1/2000)– Posttrasfusion purpura (rare)– Leukocyte-related target organ injury (2%)

Transfusion on CPB (1)
• class IIa (level of evidence C)– During CPB with moderate hypothermia, transfusion of
red cells for a hemoglobin of 6.0 g/dl or less is reasonable.
– In high risk patients, higher hemoglobin is needed.• stroke history, DM, cerebrovascular ds, carotid stenosis
– Transfusion : reasonable in case of• patient-related factors: age, severity of illness, cardiac functio
n, critical end organ ischemia• massive or active blood loss• Lab: abnormal EKG, elevated cardiac enzyme etc…

Transfusion on CPB (2)
• Transfusion during CPB: associated poor
outcomes
• In Cleveland clinic, 15,000 operations using
CPB
– strong association between the use of transfusions
and postoperative infection
– If for transfusion, notify to staff surgeons.


Postoperative considerations
Class IIa
– After cardiac operations with hemoglobin 6 g/dl or les
s, red blood cell transfusion is reasonable and can be
life-saving.
– Transfusion in patients of hemoglobin below 7.0 g/dl i
s reasonable, but no high-level evidence supports this
recommendation

Comprehensive Approach for blood
conservation !!
NovoVII
Autotransfusion
Ultrafiltration
Special CPB circuit

Topics
• Introduction
• Autologous blood donation
• Red cell saving with cell savor
• Retrograde autologous priming
• Ultrafiltration
Heparin bonded circuit
• Drugs: Aprotinin, NovoSeven
• Conclusions

Autotransfusion

Autotransfusion
• Inexpensive simple method for providing fresh blood that is essential
ly free of risk from transmission of disease, allergic reaction, alloim
munization, and blood banking mishaps.

Should be deferred from autoTf
• Evidence of infection and bacteremia
• Scheduled for AS surgery
• Unstable angina, High grade left main ds
• AMI or CVA with 6m
• Active seizure disorder (within last 3m)
• Significant cardiopulmonary disease without optimal medical Mx
• Cyanotic heart ds
• Uncontrolled hypertension

Erythropoietin
• High-dosage erythropoietin regimen of 300 U/kg IV load, m
aintenance 500 U/kg subcutaneously every other day, sup
plemented by IV iron, folate, vit C.
→ Hct increases of 2~3%/day within 5~7 days
– Effective even in hemolysis from perivalvular prosthetic leaks (endo
genous Epo levels & erythropoiesis would be maximized)
– Cost: 4,000 US dollars

Red cell scavenging

heparin10000-100000 IU/
1L NS


Intraop blood scavenging
• Final Hct 70%
• Revoming freeHb, coagulation factors, debris, other plasma components
• Concerns:– Bacteria, malignant cells, certain drugs
– Topical hemostatics: Avitene, Surgicel

Retrograde autologous priming

Retrograde Autologous Priming (RAP)

Retrograde Autologous Priming (RAP)

Retrograde Autologous Priming (RAP)

During RAP Process…
• Minimum systolic BP of 100 mmHg during entire RAP
• After ACT reached 400 seconds
• Exclusion:– Age: < 16, > 80 years old
– Exclusion for comparison of homologous transfusion
• LV dysfunction(EF<30%)
• Aorta surgery
• TCA case

Retrograde Autologous Priming (RAP)

Patient Characteristics
Control Group RAP Group
Age(yrs) 41±15 46 ±17
Female 28/50(56%) 19/37(51.3%)
BSA(m2) 1.64 ±0.18 1.64 ±0.16
Preop hct(%) 39.5±4.3 39.1±4.9
CPB(min) 105.5±58.1 174.0±84.7
ACC(min) 51.1±43.1 107.2±55.4
Kim, KJTCS 2005;38:821-7

1500
0
1381.9
613.5
0
500
1000
1500
2000
Total prime Removed vol
ml
control RAP
RAP Volume Removed(ml)

411.6
678.8
357.2
599
0
200
400
600
800
6h 24h
ml
control RAP
Postoperative Chest Tube Drainage(ml)
* P<0.05
*
*

Ultrafiltration

Ultrafiltration in Cardiac Surgery


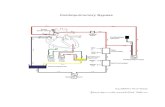
Pre-bypass UF, CUF circuit
CUF: conventional UF

Prebypass UF• Following addition of blood to CPB circuit, ultrafiltrate rem
oval is initiated, and volume replacement with a balanced electrolyte solution is titrated to maintain a minimum reservoir level.
• Reduce bradykinin, FXIII, prekallikrein, HMWK• Eliminate initial drop in blood pressure commonly seen wi
th initiation of CPB
• Reduce edema, cardiac impairment and pulmonary dysfunction– Nagashima et al. ATS 2000;70:1901-06– Nagatsu et al. Japanese JTCS 1995;48:281-85

Z-BUF circuit

Z-BUF
• Removal of large volume of ultrafiltrate and the subsequent replacement of volume with a balanced electrolyte solution.
• Water soluble inflammatory mediators are removed from circulation during ultrafiltration.
• Journois et al: removal of TNF, IL-10, myeloperoxidase, C3a

MUF circuit

MUF in adults
• Effectiveness is thought to diminish as the patient size increases.
• Little clinical impact?– Grunenfelder et al. EJCTS 2000;17:77-83– Tassani et al. J CT Vasc Anesth 1999;13:285-91
• Significant morbidity reduction?– Luciani et al. Circulation 2001;104:1253-1259

Heparin bonded circuit

Biomaterial-dependent strategies to minimize blood activation from CPB
• Biomembrane mimicry: phosphorylcholine
• Heparin-coated circuits
• Surface with modified protein adsorption

What is coating ?
Like wax on the surface of your car, it protects and keep out unwanted deposits.
Similarly the surface of plastics in Perfusion products are bonded with Carmeda or Trillium to prevent platelets and protein deposits
Trillium surfaceWax
Paint

Heparin coating
• Ionic bonding
– Gott shunt, Duraflo II
• Dispersion
– KIST shunt
• Covalent bonding
– Carmeda,Trillium
• “Burst effect”

Carmeda and Trillium bonded surface mimics the blood vessels, it reduces blood activation
1. Platelets sticks onto the wall of an artificial surface
2. Carmeda and Trillium bonded surface is less reactive to blood
Blood flow
Blood flow

Uncoated oxygenator fiber Carmeda or Trillium™
coated fiber
Massive platelet deposition Less platelet deposition

How Do The Coatings Compare to Natural Blood Vessels
Heparin Bonded Negatively Charged
Hydrophilicity
Carmeda® Yes – covalent
(non-leaching)
Yes Yes
Trillium™ Yes – covalent (non-leaching)
Yes Yes
Duraflo® II Yes – ionic (leaching) Yes Yes
Xcoating ™ No No Yes
Smart® No No Yes
Safeline® No No Yes
Bioline® Yes – ionic+ covalent
(some leaching)
Yes Yes

Comparison of two heparin-coated CPB circuits with reduced systemic
anticoagulation in routine CABG
• Carmeda BioActive Surface system
• Duraflo II coating system
Ovrum E. J Thorac Cardiovasc Surg. 2001;121(2):324-30.Ovrum E. J Thorac Cardiovasc Surg. 2001;121(2):324-30.

Clinical results favorable in both groups,

Pharmacologic Intervention

Medications ass with bleeding
• Aspirin: Irreversible platelet inhibition by blocking platelet cyclooxygenase
• Heparin: Inhibition of factors II and X, both direct and indirect thrombocytopeni
a mostly antibody-mediated (HIT)
• Coumadin: Multiple factor deficiency by blocking gamma-carboxylation Vitamin
K–dependent factors
• Antibiotics: Multiple factor deficiency owing to vitamin K malabsorption
• Multiple drugs: Thrombocytopenia owing to bone marrow inhibition of platelet p
roduction

Acquired ds with risk of bleeding
• ESRD/uremia
• Liver disease
• Malabsorption
• SLE
• Amyloid
• Malignancy

Herbs with adverse effects
• Garlic Increased bleeding
• Ginger Platelet dysfunction
Hypertension
• Gingko Increased bleeding
Platelet dysfunction
• Ginseng Hypertension
• Licorice Hypertension

Antifibrinolytics • Epsilon-aminocaproic acid (Amicar): forms a complex with
plasminogen through lysine-binding sites, thus blocking their adhesion to fibrin
• Tranexamic acid (Cyklokapron): forms a complex with plasminogen through lysine-binding sites, thus blocking their adhesion to fibrin
• Aprotinin (Trasylol): Serine protease inhibitor with an antifibrinolytic effect carried by the inhibition of plasmin and kallikrein Protection of platelet GP Ib, reducing thrombin-mediated consumption of the platelets

Antifibrinolytic agents (Class I)Antifibrinolytic agents (Class I)
– High dose aprotinin (level of evidence A)
• Is indicated to reduce total blood loss to limit reexploration in high risk pts.
• Benefits of use should be balanced against risk of renal function
– Low dose aprotinin (level of evidence A)
• Indicated to reduce the number of patients requiring transfusion and to reduce the total blood loss after cardiac surgeries
– Transamine : lysin analogue (level of evidence A)
• Indicated to reduce the number of patients requiring transfusion and to reduce the total blood loss after cardiac surgeries
• Less potent blood sparing drugs and the safety profile is less well studied compared with aprotinin.
Limits transfusion_drug

Safety of aprotinin
– May be associated with thrombotic risk, especially renal dysfunction– FDA suggestions
• should be used with caution• only for patients in whom the benefits of the drug outweighs the risks, m
ostly of renal dysfunction and of hypersensitivity– Renal dysfunction: its affinity for the proximal renal tubules– D’Ambra et al.
• Higher rate of renal dysfunction in patients undergoing valve surgery• esp. DM (16% vs. 5%)
– Kincaid et al.• In CABG, combination with ACE inhibitors was associated with increased r
ate of ARF (OR 2.9)
Limits transfusion_drug

High dose aprotinin vs. low dose
SNUH (Kim et al, 2008)
– 28 patients, prospective randomized
– Compare the risks and effects on bleeding and
inflammatory response.
Limits transfusion_drug

Limits transfusion_drug
• No difference on transfusion requirement• No difference on renal dysfunction

NovoSeven
• Recombinant factor VIIa (rFVIIa) (Bagsvaerd, Denmark)
• First used to decrease hemorrhage in hemophilia A or B
• In 1999, US FDA licensed rFVIIa for this purpose and in 2005 it was furth
er approved for surgical procedures in the same patient group, and for pat
ients with factor VII (FVII) deficiency.
• Although off-label use of rFVIIa has been reported in cardiac surgery.

NovoSeven
• Relatively little is known about the molecular mec
hanisms by which rFVIIa induces the formation of
a stable hemostatic plug.
– no direct effect on hemostatic plug formation, but exer
ts an effect by enhancing thrombin generation at sites
of tissue injury.

NovoSeven– When vessel injury occurs in normal subjects, subendothe
lial cells that express TF are exposed to the blood.
– The resulting TF-FVIIa complex catalyzes the conversion of factor X into its active form (Xa) leading to thrombin formation and platelet activation.


NovoSeven
(1) prophylactically, with an aim of reducing p
ostoperative bleeding
(2) as a "rescue" therapy in hemorrhage refr
actory to other treatments

NovoSeven, Cost….
– A single 90 µg/kg dose of rFVIIa to an 80 kg patient costs $4,500.
– may be offset against the costs of multiple transfusions, length of hospital stay, or even death.
– multicenter trials, and cost-effectiveness analyses should be a part of any future trial involving rFVIIa.


Conclusions
With improving technology, awareness of blood conservation
techniques, and better pharmacologic agents, a
multidisciplinary approach to blood conservation can make
bloodless heart surgery possible.
Using a team approach that both optimizes and integrates the
use of each of these measures, the use of homologous blood
can be markedly reduced in a majority of cardiac surgical
patients.


![[법무법인 민후 | 김경환 변호사] 빅데이터산업과 개인정보보호](https://static.fdocument.pub/doc/165x107/5871d53d1a28ab423c8b67a1/-5871d53d1a28ab423c8b67a1.jpg)
![[법무법인 민후 | 김경환 변호사] 제13회 프로보노 지식나눔 콘서트 강연자료](https://static.fdocument.pub/doc/165x107/58ec83f01a28abf06f8b45c7/-13-58ec83f01a28abf06f8b45c7.jpg)


![[법무법인 민후 | 김경환 변호사] 지방자치단체를 위한 전자소송과 소송실무(전자소송법)](https://static.fdocument.pub/doc/165x107/5871d4e51a28ab423c8b66d5/-5871d4e51a28ab423c8b66d5.jpg)
![[법무법인 민후 | 김경환 변호사] 특허분쟁시 대처방안](https://static.fdocument.pub/doc/165x107/55c9ca42bb61eb92328b47d1/-55c9ca42bb61eb92328b47d1.jpg)
![[법무법인 민후 l 김경환 변호사] 비트코인과 개인정보 (개인정보보호, 개인정보법)](https://static.fdocument.pub/doc/165x107/55c4a651bb61eb671f8b45c5/-l-55c4a651bb61eb671f8b45c5.jpg)

![[법무법인 민후 | 김경환 변호사] 소프트웨어산업진흥법의 한계와 개선방향](https://static.fdocument.pub/doc/165x107/55ce6e4abb61eba57e8b4854/-55ce6e4abb61eba57e8b4854.jpg)


![[법무법인 민후 | 김경환 변호사] 정보보호 관련 법령과 대응방안 (정보보호법,개인정보보호법)](https://static.fdocument.pub/doc/165x107/55ce3147bb61eb341c8b4755/-55ce3147bb61eb341c8b4755.jpg)
![[법무법인 민후 l 김경환 변호사] 교육정보의 활용과 보호 (개인정보, 교육정보활용)](https://static.fdocument.pub/doc/165x107/55ce6e72bb61eb9e7e8b4877/-l-55ce6e72bb61eb9e7e8b4877.jpg)
![[법무법인 민후 | 김경환 변호사] 개인정보보호의 국제동향 (잊혀질권리)](https://static.fdocument.pub/doc/165x107/55cb5d9abb61ebb26d8b47dd/-55cb5d9abb61ebb26d8b47dd.jpg)
![[법무법인 민후 | 김경환 변호사] 조문순으로 정리한 개정상법 설명 (1)](https://static.fdocument.pub/doc/165x107/55d22c09bb61eb8d438b475b/-55d22c09bb61eb8d438b475b.jpg)