Basics of Head and Neck Contouring for IMRT · PDF fileBasics of Head and Neck Contouring for...
Transcript of Basics of Head and Neck Contouring for IMRT · PDF fileBasics of Head and Neck Contouring for...
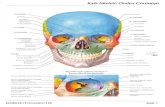
Basics of Head and Neck Contouring for IMRT
Kenneth Hu, MD Associate Professor, Dept of Radiation Oncology Co-Director of the NYU Head and Neck Institute
June 21, 2017 ICARO 2, Vienna
Objectives • Radiation Planning • Delineating and Contouring GTV • Elective treatment of Nodal Stations • Outline organs at risk
IMRT Radiation Planning • Multidisciplinary Plan—Chemotherapy, Definitive surgery
vs. radiation therapy of primary site, neck • Radiation Approach—70Gy to GTV, 60-66Gy high risk,
50-60Gy elective • Sequential Cone Down IMRT Plans—50Gy initial20Gy CD • Dose-painting Plan: 70Gy/60Gy/56Gy in 33-35 Fractions
• Technical Aspects • Five Point Mask to Immobilize Head, Neck and Shoulders • Treatment planning CT with IV contrast • Wire any scars, consider bolus, usually 3mm
• Imaging • Daily vs weekly • Orthogonal pair (kv or mv) vs cone-beam CT (allows to evaluate
rotational changes and soft tissue changes of tumor, normal tissue)
Delineating and Contouring GTV • Physical exam and endoscopy • CT neck, PET/CT standard—iodine contrast enhancing
soft tissue is GTV, not FDG • MRI needed if Nasopharynx, Sinus, Parotid Tumors
• Helps better delineate soft tissue and perineural neural spread • Distinguish mucus from solid tumor
• CTV1 (70Gy) --Add 3-5mm margin to GTV
Incidence of Positive Lymph Nodes • Unilateral versus Contralateral node positive
• Oral Cavity : 30% 5% • Oropharynx: 60-75% 20-30% • Larynx: 55% 20% • Hypopharynx: 75% 10% • Nasopharynx: 90% 50% • Nasal Cavity/PNS: 10% <5%
References for Lymph Node Delineation
• CT-Based Delineation of Lymph Node Levels and Related CTV in Node Negative Neck Dahanca, EORTC, GORTEC,NCIC,RTOG • Gregoire, et al. Radiotherapy and Oncology, 65 2003, 227-
236 • Proposal for the delineation of the nodal CTV in Node-positve and the post-operative neck • Gregoire, et al. Radiotherapy and Oncology, 79 2006, 15-20
• 2013 update: Delineation of neck nodal levels: • Gregoire, et al, Radiotherapy and Oncology, 110 2014, 172-
81
Coverage of Nodal Volumes • Retropharyngeal Nodes—
• Skull Base down to hyoid bone/C2 • Lateral RP LN involved first (spare constrictors) • Medial RP LN if lateral RP LN+
• Jugular Nodal • LN- Inferior margin of C1 Transverse and selective
nodal • jugular foramen if LN+ and comprehensive nodal treatment
• Level VI (pre-tracheal/delphian) for subglottic tumor/hypopharynx/thyroid
• Level VII (superior mediastinum) with level IV, thyroid, cervical esophagus
CTV of LN+ J foramen
Sparing of parotid in LN-
Sup constrictor spared on L
Upper Ib,II,Va
ICA, IJV
L Med RP LN
C1 TVP
• Washington University • 748 pts opx/hpx/lx/unk primary • IMRT—3 generations of elective coverage (1997-2010)in
contralateral node neg neck • A) Bilateral RS/RP, 260pts B)Sparing CL RS 205 pts C)
Spared CL RS/RP 283 pts • Median Followup 37mo’s • MDADI Dysphagia QOL and POF
Swallowing Better in Group C vs A
MDADI at >30mo in group A vs group C Differences >18points are significant NO FAILURES IN SPARED RS/RP LN’S
IMRT Improved Xerostomia: PASSPORT Trial • 94 pts with OP/HP cancer randomized to IMRT vs 3DRT • Whole contralateral parotid < 24Gy
Lent SOMA Score EORTC Dry Mouth Subscale
Nutting CM et al, Lancet Oncol 2011, 12:127
Submandibular Gland Sparing
• 36 pts OPX (n=28) NPX treated with RT • Case matched—18pts with SMG sparing and 18 without. • SMG spared had lower N stage (no N2b-3) vs SMG non-
spared group (59% N2b-3)
Saarilahti et al Radiotherapy and Oncology78 (2006) 270–75.
• 78 pts III/IV Opx prospectively followed after IMRT designed to spare bilateral parotids, oral cavity, contralateral SMG
• Pt and observer reported xerostomia surveys and salivary collection up to 2yrs
Little, et al, IJROBP In press
Dysphagia RTOG-0129 Cisplatin + RT PEG dependence 1yr 30% Measures of dysphagia: Feeding tube dependence videofluoroscopy/silent
aspiration dysphagia qol surveys
Pharyngeal Constrictors
Courtesy Dr. Eisbruch/Le Werbrouch J et al, IJROBP 2009, 73:1187
Superior
Mid
Inferior
0 .1
.2
.3
.4
.5
.6
0 10 20 30 40 50 60 70 80
Dose superior constrictor muscle (Gy)
Cyberknife (3x + 4x)
Brachytherapy implant
No BT / No Cyberknife
Probability Swallowing Problems
3x 4x
Levendag PC, et al. Radiother Oncol. 2007
PEG dependence 1.4% at 1yr Dysphagia related to dose to PC,Lx, Esoph Neck dissection/smoking/t-stage
• 5 pts with strictures • 8 pts with pneumonia—all silent aspirators