An Alumina Ceramic Total Talar Prosthesis for...
Transcript of An Alumina Ceramic Total Talar Prosthesis for...

An Alumina Ceramic Total Talar Prosthesis forOsteonecrosis of the Talus
Akira Taniguchi, MD, PhD, Yoshinori Takakura, MD, PhD, Yasuhito Tanaka, MD, PhD, Hiroaki Kurokawa, MD,Kiyonori Tomiwa, MD, Takenori Matsuda, MD, Tsukasa Kumai, MD, PhD, and Kazuya Sugimoto, MD, PhD
Investigation performed at the Department of Orthopaedic Surgery, Nara Medical University, Nara, Japan
Background: Treatment of osteonecrosis of the talus is challenging. Total talar replacement has the potential to restorethe function of the ankle joint without an associated leg-length discrepancy. The purpose of the present study was toinvestigate postoperative function and pain after total talar replacement in patients with osteonecrosis of the talus.
Methods: Fifty-five ankles in fifty-one consecutive patients with osteonecrosis of the talus who were treated with a totaltalar replacement from 2005 to 2012 were included in the investigation. Scores according to the Japanese Society forSurgery of the Foot (JSSF) ankle-hindfoot scale and the Ankle Osteoarthritis Scale (AOS) were assessed before surgery andat the final follow-up evaluation.
Results: According to the JSSF ankle-hindfoot scale, the score for pain improved from a mean (and standard deviation)of 15 ± 9.4 points (range, 0 to 20 points) to 34 ± 5.6 points (range, 20 to 40 points); the score for function, from 21.2 ±9.7 points (range, 4 to 38 points) to 45.1 ± 4.0 points (range, 37 to 50 points); the score for alignment, from 6.0 ± 2.8points (range, 5 to 10 points) to 9.8 ± 0.9 points (range, 5 to 10 points); and the total score, from 43.1 ± 17.0 points(range, 11 to 68 points) to 89.4 ± 8.4 points (range, 76 to 100 points). According to the AOS scale, the score for “painat its worst” improved from a mean of 6.1 ± 3.3 points (range, 0 to 9.9 points) to 2.0 ± 1.7 points (range, 0 to 6.3points).
Conclusions: Prosthetic talar replacement is a useful procedure for patients with osteonecrosis of the talus as it main-tains ankle function.
Level of Evidence: Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
The blood supply to the talus is mainly provided bybranches of the posterior tibial and peroneal arteries1,2.Because approximately 60% of the surface of the talus is
covered with articular cartilage, the blood supply through theperiosteum is limited3,4. Thus, fractures of the talus often in-terrupt the blood supply, inducing osteonecrosis. The pre-dicted prevalence of traumatic osteonecrosis associated withtalar neck fractures has been reported to range from 0% to10% for Hawkins5 type-I fractures and to be >60% for type-IIIfractures6.
Treatment of osteonecrosis of the talus is quite chal-lenging7. Blair8 introduced the original tibiotalar arthrodesistechnique; subsequently, other investigators reported modifi-cations of this procedure that minimized shortening of theoperatively treated leg9-11. However, arthrodesis eliminates an-kle motion and pseudarthrosis may develop12. In recent years,tibiotalar or tibiocalcaneal arthrodesis using callotasis com-bined with Ilizarov external fixation has been reported12,13.Although a bone allograft can compensate for the bone defect,some countries have cultural problems associated with allografts.
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support ofany aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of thiswork, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, noauthor has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence whatis written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version ofthe article.
Peer Review: This article was reviewed by the Editor-in-Chief and one Deputy Editor, and it underwent blinded review by two or more outside experts. The Deputy Editorreviewed each revision of the article, and it underwent a final review by the Editor-in-Chief prior to publication. Final corrections and clarifications occurred during one ormore exchanges between the author(s) and copyeditors.
1348
COPYRIGHT � 2015 BY THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED
J Bone Joint Surg Am. 2015;97:1348-53 d http://dx.doi.org/10.2106/JBJS.N.01272

In recent years, there have been major developments in artifi-cial bone products such as calcium phosphate or hydroxyap-atite; however, it is unclear whether replacement with the largeamount of artificial bone required after talar body necrosis pro-vides sufficient strength.
Harnroongroj et al.14,15 introduced a stainless-steel talarbody prosthesis designed by slit scanography and reported apostoperative median score of >75 points on the American Or-thopaedic Foot & Ankle Society ankle-hindfoot scoring system.In contrast, we developed two models of custom-made artificialtalar body implants made of alumina ceramic designed withcomputed tomography (CT)16,17. The first-generation implant,which had a peg on the anterior surface of the implant, was inserted
into the head of the talus and fixed with bone cement. Althoughclinical results were initially satisfactory, some implants developedloosening at the fixation site. The second-generation implant wasdesigned without a peg and was not fixed to the talar head. Theoverall clinical results were also initially acceptable with this im-plant, but late collapse of the talar head occurred in some pa-tients17. We therefore decided to replace the whole talus with atotal talar prosthesis (Fig. 1) in 2005, postulating that such an im-plant would restore function of the ankle joint and relieve pain.The purpose of the present study was to assess pain and functionin patients treatedwith an alumina ceramic total talar replacementand determine if it is an acceptable treatment for talar osteone-crosis. The present investigation looked at the primary outcomes
TABLE I Comparison of the JSSF Ankle-Hindfoot Scale Scores at the Preoperative and Final Follow-up Evaluations
Outcome Measure Preoperative* (points) Final Follow-up* (points)
Total score 42.2 ± 17.4 (11 to 68) 89.1 ± 8.6 (76 to 100)
Pain 15.0 ± 9.4 (0 to 20) 34.0 ± 5.6 (20 to 40)
Function 21.2 ± 9.7 (4 to 38) 45.1 ± 4.0 (37 to 50)
Alignment 6.0 ± 2.8 (5 to 10) 9.8 ± 0.9 (5 to 10)
*The values are given as the mean and standard deviation, with the range in parentheses. The difference between the preoperative and finalfollow-up scores was significant for all outcome measures (p < 0.01).
TABLE II Comparison of the Ankle Osteoarthritis Scale Scores at the Preoperative and Final Follow-up Evaluations
Outcome Measure Preoperative* (points) Final Follow-up* (points)
Pain
At its worst? 6.1 ± 3.3 (0 to 9.9) 2.0 ± 1.7 (0 to 6.3)†
Before you get up in the morning? 5.8 ± 3.3 (0 to 9.8) 2.1 ± 3.0 (0 to 9.9)†
When you walked barefoot? 6.2 ± 3.3 (0 to 9.6) 1.7 ± 1.8 (0 to 5.2)†
When you stood barefoot? 5.6 ± 3.2 (0 to 9.9) 1.7 ± 2.0 (0 to 6.9)†
When you walked wearing shoes? 6.2 ± 3.0 (0 to 9.9) 1.6 ± 1.7 (0 to 4.5)†
When you stood wearing shoes? 5.4 ± 3.3 (0 to 9.8) 1.4 ± 1.6 (0 to 5.2)†
When you walked wearing shoe inserts or braces? 4.9 ± 3.2 (0 to 9.6) 2.2 ± 2.2 (0 to 7.2)‡
When you stood wearing shoe inserts or braces? 4.8 ± 3.4 (0 to 9.8) 2.1 ± 2.2 (0 to 7.3)‡
At the end of the day? 7.2 ± 2.8 (0 to 9.8) 2.7 ± 2.5 (0 to 7.4)†
Function
Walking around the house? 4.4 ± 3.2 (0 to 9.8) 1.0 ± 2.1 (0 to 8.8)†
Walking outside on uneven ground? 4.8 ± 3.3 (0 to 9.9) 2.0 ± 2.9 (0 to 8.7)†
Walking four or more blocks? 4.5 ± 3.5 (0 to 10) 1.5 ± 2.8 (0 to 8.8)†
Climbing stairs? 5.4 ± 3.2 (0 to 9.7) 1.9 ± 2.8 (0 to 8.9)†
Descending stairs? 5.7 ± 3.2 (0 to 9.8) 2.4 ± 3.0 (0 to 8.6)†
Standing on tip toes? 5.5 ± 3.5 (0 to 9.6) 2.1 ± 3.2 (0 to 9.4)†
Getting out of a chair? 4.4 ± 3.3 (0 to 9.5) 0.8 ± 1.4 (0 to 6.8)†
Climbing up or down curbs? 5.0 ± 3.4 (0 to 9.5) 1.9 ± 2.7 (0 to 8.7)†
Walking fast or running? 5.9 ± 3.9 (0 to 9.8) 3.2 ± 3.6 (0 to 9.8)‡
*The values are given as the mean and standard deviation, with the range in parentheses. †The difference between the preoperative and finalfollow-up scores was significant (p < 0.01). ‡The difference between the preoperative and final follow-up scores was significant (p < 0.05).
1349
THE JOURNAL OF BONE & JOINT SURGERY d J B J S .ORG
VOLUME 97-A d NUMBER 16 d AUGUST 19, 2015AN ALUMINA CERAMIC TOTAL TALAR PROSTHES I S FOR
OSTEONECROS I S OF THE TALUS

of postoperative function and pain after total talar replacement inconsecutive patients with osteonecrosis of the talus treated at asingle institution.
Materials and Methods
This retrospective review of prospectively collected data was conducted inaccordance with the Declaration of Helsinki
18and the Guideline for Good
Clinical Practice19and was approved by the ethics committee of the NaraMedical
University, Nara, Japan. We treated fifty-four consecutive patients (fifty-eightankles) with osteonecrosis of the talus from October 2005 to May 2012. Two ofthe authors (Y.T. and Y.T.) performed the total talar prosthetic replacements.Three patients were excluded because the distal end of the tibia had degenerativechanges and needed to be replaced with a tibial component. The remaining fifty-five ankles in fifty-one patients (forty-six women and five men) had completefollow-up and are included in this study. Osteonecrosis of the talus was caused byfracture of the talar neck in four patients (four ankles) and was idiopathic in theremaining forty-seven patients (fifty-one ankles). The diagnosis was made withweight-bearing radiographs (Fig. 2-A), and was confirmed with magnetic reso-nance imaging (MRI) (Fig. 2-B). The osteonecrosis was not due to alcohol abuseor corticosteroids in any of the patients. Because our institution treats patientswith chronic orthopaedic conditions from all over Japan, we have a high pro-portion of patients with idiopathic disorders. The average body mass index (andstandard deviation) was 24.3 ± 3.73 kg/m2 (range, 18.7 to 31.6 kg/m2). Theaverage age at the time of surgery was 61.4 ± 8.5 years (range, thirty-nine toseventy-seven years), and the average duration of follow-up was 52.8 ± 22.0months (range, twenty-four to ninety-six months). In this series, no patient hadany osseous deformity other than that of the talus.
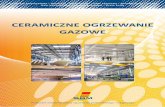
For the production of each prosthesis, the relevant dimensions weremeasured on radiographs and CT scans of the contralateral, normal talus. The
Fig. 1
Alumina ceramic total talar prosthesis that was designed using the data
obtained by CT from the contralateral side.
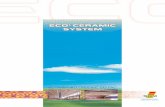
Fig. 2-A Fig. 2-B
Figs. 2-A, 2-B, and 2-C A sixty-two-year-old woman who had a collapsed talus that was due to osteonecrosis. Fig. 2-A Preoperative radiograph of the
ankle. Fig. 2-B Sagittal T1-weighted 1.5-T MRI shows a low-intensity area in the talar body that reveals osteonecrosis of the talus.
1350
THE JOURNAL OF BONE & JOINT SURGERY d J B J S .ORG
VOLUME 97-A d NUMBER 16 d AUGUST 19, 2015AN ALUMINA CERAMIC TOTAL TALAR PROSTHES I S FOR
OSTEONECROS I S OF THE TALUS

CT images were made at 2-mm intervals in the axial and sagittal planes, and athree-dimensional wire model and implant were assembled. Then, a stereo-lithographic model was cast, and from that an alumina ceramic prosthesis wasproduced. These prostheses require four weeks to produce.
In patients with bilateral talar osteonecrosis, the artificial tali were de-signed using imaging data from the less distorted side to produce an image ofthe normal shape.
The surgery was performed via an anterior approach to the ankle joint.After the talus was completely resected, an artificial talus was substituted withmanual traction of the foot. The remaining capsule was repaired to the extentpossible.
Partial weight-bearing was allowed two weeks after surgery and wasgradually increased to full weight-bearing by three weeks after surgery. Ashort leg cast was fitted for the first three postoperative weeks, and a soft,multistrap, soft ankle orthosis was used continuously for more than a monththereafter.
Clinical results were evaluated by assessing scores on the Japanese So-ciety for Surgery of the Foot (JSSF) ankle-hindfoot scale
20,21, which has a
maximum score of 100 points (consisting of 40 points for pain, 50 points forfunction, and 10 points for alignment), and the Ankle Osteoarthritis Scale(AOS)
22before surgery and at the final follow-up visit. The range of motion in
dorsal and plantar flexion was measured at that time. The paired-sample t testand Wilcoxon signed-rank test were used to compare preoperative and post-operative scores. All data were tested for normality, and the paired t test wasused for normally distributed data (i.e., all of the JSSF ankle-hindfoot scalescores and the scores for the question “Pain when you walked wearing shoeinserts or braces?” in the AOS scoring system), while the Wilcoxon signed-ranktest was used for the rest.
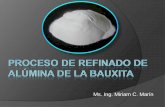
Degenerative changes in adjacent joints were evaluated with a weight-bearing ankle radiograph (Fig. 2-C), and instability was assessed with stressradiography. Osteosclerosis was assessed on the basis of osseous reactions in thetibia, navicular bone, and calcaneus in weight-bearing lateral radiographs of theankle. Ankle instability was evaluated postoperatively with the talar tilt angle ininversion and eversion-stressed anteroposterior radiographs of the ankle,whereas the anterior drawer distance was assessed on anterior drawer stresslateral radiographs.
All clinical assessments, examinations, and radiographic evaluations inthis investigation were performed by one of us (A.T.) at the yearly follow-upexaminations, independent of the operating surgeons.
Source of FundingWe received no external funding for this study.
Results
Preoperative and postoperative scores on the JSSF ankle-hindfoot scale are listed in Table I, and those on the AOS
scoring system are listed in Table II. According to the JSSFankle-hindfoot scale, the mean scores for pain improved from15.0 ± 9.4 points (range, 0 to 20 points) to 34.0 ± 5.6 points(range, 20 to 40 points); the scores for function, from 21.2 ± 9.7points (range, 4 to 38 points) to 45.1 ± 4.0 points (range, 37 to50 points); the scores for alignment, from 6.0 ± 2.8 points(range, 5 to 10 points) to 9.8 ± 0.9 points (range, 5 to 10points); and total scores, from 43.1 ± 17.0 points (range, 11 to68 points) to 89.4 ± 8.4 points (range, 76 to 100 points). Themean score for the AOS category of pain “at its worst” im-proved from 6.1 ± 3.3 points (range, 0 to 9.9 points) to 2.0 ± 1.7points (range, 0 to 6.3 points). The mean preoperative range ofmotion was 0.5� ± 3.7� (range, –8� to 7�) in dorsiflexion and43.7� ± 8.3� (range, 32� to 60�) in plantar flexion. At the time ofthe final follow-up, the mean range of motion was 5.4� ± 4.9�(range, 0� to 17�) in dorsiflexion and 32.0� ± 8.9� (range, 17� to55�) in plantar flexion.
Fig. 2-C
The talus was replaced with an alumina ceramic total talar prosthesis.
Three years after the operation, there was no sinking or osteolytic change
in adjacent bones.
TABLE III Postoperative Results of Radiographic Assessmentof the Fifty-five Ankles
Finding
Radiographic assessment(no. of ankles)
Osteosclerosis of the distalend of the tibia
44% (24)
Osteosclerosis of the navicular 9% (5)
Osteosclerosis of the calcaneus 35% (19)
Stress radiography*
Talar tilt angle in inversion (deg) 5.0 ± 3.6 (21 to 17)
Talar tilt angle in eversion (deg) 1.1 ± 3.0 (23 to 10.3)
Anterior drawer distance (mm) 1.4 ± 0.5 (0.7 to 2.4)
*The values are given as the mean and the standard deviation,with the range in parentheses.
1351
THE JOURNAL OF BONE & JOINT SURGERY d J B J S .ORG
VOLUME 97-A d NUMBER 16 d AUGUST 19, 2015AN ALUMINA CERAMIC TOTAL TALAR PROSTHES I S FOR
OSTEONECROS I S OF THE TALUS

At the time of the final follow-up, osteosclerosis wasnoted at the distal end of the tibia in 44% (twenty-four) of thefifty-five ankles, in the navicular in 9% (five ankles), and in thecalcaneus in 35% (nineteen ankles). The mean talar tilt anglewas 5.0� ± 3.6� (range, –1� to 17�) on inversion stress radio-graphs and 1.1� ± 3.0� (range, –3� to 10.3�) on eversion stressradiographs. Themean anterior drawer distancewas 1.4± 0.5mm(range, 0.7 to 2.4 mm) (Table III). In our case series, no patientwas a top-level athlete or did physically demanding work. Allpatients had returned to work or to the normal activities ofdaily living. No patient had wound dehiscence or infection thatrequired reoperation or amputation.
Discussion
The talus tends to have a precarious circulation because 60%of its surface is covered with articular cartilage3,4; this can
result in traumatic or idiopathic talar osteonecrosis. The pre-dicted prevalence of osteonecrosis has been reported to rangefrom 0% to 10% for Hawkins5 type-I fractures and to be >60%for type-III fractures6. The talus is the third most common siteof idiopathic osteonecrosis, after the femoral head and femoralcondyle23. This condition is reportedly caused by frequent use ofcorticosteroids24-26, heavy consumption of alcohol27, systemic lu-pus erythematosus27, hemophilia28,29, and severe acute respiratorysyndrome30; however, in many patients, no cause is evident.
Although arthrodesis of the ankle achieves acceptablefunction, it eliminates the motion of the ankle and pseudar-throsis may develop. For this reason, tibiocalcaneal fixationsupplemented with iliac crest bone graft is indicated in somecases of extensive osteonecrosis of the talar body.
Replacement of the necrotic talus with an artificial totaltalus maintains leg length and joint function. Harnroongrojand Harnroongroj15 reported mid-term to long-term resultsafter talar replacement with an artificial talar body prosthesismade from 316L stainless steel. In their study, two of thirty-sixprocedures failed because the size of the implant was mis-matched. Our alumina ceramic implants are individually de-signed using data from the contralateral, normal side and aremachine made; no size mismatches occurred in our series. Inone of the patients described byHarnroongroj andHarnroongroj,the prosthesis failed because of necrotic change in the talar neckand head. In the past, we encountered cases of loosening ofthe talar neck or destruction of the talar head after replacementof the talar body17. The total talar prosthesis has been designedto overcome these problems, and none of these types of com-plications occurred in the present series.
Our implants are made of alumina ceramic. The talus issurrounded by the tibia, fibula, navicular bone, and calcaneus,
and 60% of its surface is covered with articular cartilage. It isextremely important to make an artificial talus from a materialwith strong biological affinity. Yoshinaga31 reported that aluminaceramic has less wear than 316L stainless steel. Alumina ceramicis thought to be an ideal material for an artificial talus. Becausethe talus has complicated joint surfaces with surrounding bones,custom-made alumina ceramic implants are ideal for adjustingthe joint, producing stability, preventing degenerative changes inadjacent joints, and dispersing the pressures appropriately.
The limitations of this study are the small number ofpatients and the retrospective design of the investigation. Weplan to perform a prospective cohort study in the near future.In summary, we followed fifty-one patients with fifty-five totaltalar replacements for an average of 52.8 months (range, twenty-four to ninety-six months). None required revision, and themean scores on the JSSF ankle-hindfoot scale improved from15.0 to 34.0 points for pain, from 21.2 to 45.1 points for func-tion, from 6.0 to 9.8 points for alignment, and from 43.1 to 89.4points for the total score. The mean scores for the AOS categoryof pain “at its worst” improved from 6.1 to 2.0 points. Prosthetictotal talar replacement is a useful procedure for patients withosteonecrosis of the talus because the favorable congruency ofthe custom-made implant with the adjacent joints producesstability and maintains ankle function. n
Akira Taniguchi, MD, PhDYasuhito Tanaka, MD, PhDHiroaki Kurokawa, MDKiyonori Tomiwa, MDTakenori Matsuda, MDTsukasa Kumai, MD, PhDDepartment of Orthopaedic Surgery,Nara Medical University,840 Shijyo-cho, Kashihara,Nara 634-8522, Japan.E-mail address for A. Taniguchi: [email protected]
Yoshinori Takakura, MD, PhDDepartment of Orthopaedic Surgery,Nishi Nara Central Hospital,1-15 Tsurumai Nishi-cho, Nara-shi,Nara 631-0022, Japan
Kazuya Sugimoto, MD, PhDDepartment of Orthopaedic Surgery,Nara Prefecture General Medical Center,1-30-1 Hiramatsu, Nara-shi,Nara 631-0846, Nara, Japan
References
1. Kelikian AS, Sarrafian SK, editors. Sarrafian’s anatomy of the foot and ankle:descriptive, topographical, functional. 3rd ed. Philadelphia: Lippincott Williams &Wilkins; 2011.2. Tennant JN, Rungprai C, Pizzimenti MA, Goetz J, Phisitkul P, Femino J, AmendolaA. Risks to the blood supply of the talus with four methods of total ankle arthroplasty:a cadaveric injection study. J Bone Joint Surg Am. 2014 Mar 5;96(5):395-402.
3. Mulfinger GL, Trueta J. The blood supply of the talus. J Bone Joint Surg Br. 1970Feb;52(1):160-7.4. Coughlin MJ, Mann RA, Saltzman CL, editors. Surgery of the foot and ankle.8th ed. Philadelphia: Mosby; 2007.5. Hawkins LG. Fractures of the neck of the talus. J Bone Joint Surg Am. 1970Jul;52(5):991-1002.
1352
THE JOURNAL OF BONE & JOINT SURGERY d J B J S .ORG
VOLUME 97-A d NUMBER 16 d AUGUST 19, 2015AN ALUMINA CERAMIC TOTAL TALAR PROSTHES I S FOR
OSTEONECROS I S OF THE TALUS

6. Vallier HA, Nork SE, Barei DP, Benirschke SK, Sangeorzan BJ. Talar neck frac-tures: results and outcomes. J Bone Joint Surg Am. 2004 Aug;86(8):1616-24.7. Adelaar RS, Madrian JR. Avascular necrosis of the talus. Orthop Clin North Am.2004 Jul;35(3):383-95, xi.8. Blair HC. Comminuted fractures and fracture dislocations of the body of theastragalus. Am J Surg. 1943;59:37-43.9. Lionberger DR, Bishop JO, Tullos HS. The modified Blair fusion. Foot Ankle. 1982Jul-Aug;3(1):60-2.10. Lin SY, Cheng YM, Huang PJ, Tien YC, Yap WK. Modified Blair method for anklearthrodesis. Kaohsiung J Med Sci. 1998 Apr;14(4):217-20.11. Hantira H, Al Sayed H, Barghash I. Primary ankle fusion using Blair technique forseverely comminuted fracture of the talus. Med Princ Pract. 2003 Jan-Mar;12(1):47-50.12. Dennison MG, Pool RD, Simonis RB, Singh BS. Tibiocalcaneal fusion for avas-cular necrosis of the talus. J Bone Joint Surg Br. 2001 Mar;83(2):199-203.13. Kovoor CC, Padmanabhan V, Bhaskar D, George VV, Viswanath S. Ankle fusionfor bone loss around the ankle joint using the Ilizarov technique. J Bone Joint Surg Br.2009 Mar;91(3):361-6.14. Harnroongroj T, Vanadurongwan V. The talar body prosthesis. J Bone Joint SurgAm. 1997 Sep;79(9):1313-22.15. Harnroongroj T, Harnroongroj T. The talar body prosthesis: results at ten to thirty-sixyears of follow-up. J Bone Joint Surg Am. 2014 Jul 16;96(14):1211-8. Epub 2014 Jul 16.16. Tanaka Y, Takakura Y, Kadono K, Taniguchi A, Hayashi K, Iida Z, Sugimoto K,Tohma Y, Ohgushi H. Alumina ceramic talar body prosthesis for idiopathic asepticnecrosis of the talus. Key Eng Mater. 2003;240-242:805-8.17. Taniguchi A, Takakura Y, Sugimoto K, Hayashi K, Ouchi K, Kumai T, Tanaka Y.The use of a ceramic talar body prosthesis in patients with aseptic necrosis of thetalus. J Bone Joint Surg Br. 2012 Nov;94(11):1529-33.18. Nicholson RH, Crawley FP. Revising the Declaration of Helsinki: a fresh start.Bull Med Ethics. 1999 Oct;(151):13-7.19. European Medicines Agency. ICH Topic E 6, Guideline for Good Clinical Practice.2002. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002874.pdf. Accessed 2015 May 7.
20. Niki H, Aoki H, Inokuchi S, Ozeki S, Kinoshita M, Kura H, Tanaka Y, Noguchi M,Nomura S, Hatori M, Tatsunami S. Development and reliability of a standard ratingsystem for outcome measurement of foot and ankle disorders I: development ofstandard rating system. J Orthop Sci. 2005 Sep;10(5):457-65.21. Niki H, Aoki H, Inokuchi S, Ozeki S, Kinoshita M, Kura H, Tanaka Y, Noguchi M,Nomura S, Hatori M, Tatsunami S. Development and reliability of a standard ratingsystem for outcome measurement of foot and ankle disorders II: interclinicianand intraclinician reliability and validity of the newly established standard ratingscales and Japanese Orthopaedic Association rating scale. J Orthop Sci. 2005Sep;10(5):466-74.22. Domsic RT, Saltzman CL. Ankle osteoarthritis scale. Foot Ankle Int. 1998Jul;19(7):466-71.23. Miki H. [Osteonecrosis of ankle with atraumatic osteonecrosis of the femoralhead.] Bessatsu Seikeigeka. 2005;48:229-33. Japanese.24. Delanois RE, Mont MA, Yoon TR, Mizell M, Hungerford DS. Atraumatic osteo-necrosis of the talus. J Bone Joint Surg Am. 1998 Apr;80(4):529-36.25. Adleberg JS, Smith GH. Corticosteroid-induced avascular necrosis of the talus.J Foot Surg. 1991 Jan-Feb;30(1):66-9.26. Tasic V, Trajkovski Z, Zafirovski G, Gucev Z, Trompeter RS. Aseptic necrosis ofboth tali in a child with steroid-dependent nephrotic syndrome. Nephrol Dial Trans-plant. 2006 Jun;21(6):1702-4. Epub 2006 Jan 6.27. Harris RD, Silver RA. Atraumatic aseptic necrosis of the talus. Radiology. 1973Jan;106(1):81-3.28. Kemnitz S, Moens P, Peerlinck K, Fabry G. Avascular necrosis of the talus inchildren with haemophilia. J Pediatr Orthop B. 2002 Jan;11(1):73-8.29. MacNicol MF, Ludlam CA. Does avascular necrosis cause collapse of the domeof the talus in severe haemophilia? Haemophilia. 1999 Mar;5(2):139-42.30. Hong N, Du XK. Avascular necrosis of bone in severe acute respiratory syn-drome. Clin Radiol. 2004 Jul;59(7):602-8.31. Yoshinaga K. Replacement of femoral head using endoprosthesis (aluminaceramics vs metal)—an experimental study of canine articular cartilage. NihonSeikeigeka Gakkai Zasshi. 1987 May;61(5):521-30.
1353
THE JOURNAL OF BONE & JOINT SURGERY d J B J S .ORG
VOLUME 97-A d NUMBER 16 d AUGUST 19, 2015AN ALUMINA CERAMIC TOTAL TALAR PROSTHES I S FOR
OSTEONECROS I S OF THE TALUS